MCRT Webcast: Myeloma Genetics with Three Experts
Knowing about genetics is not just for scientists anymore. To be an informed myeloma patient it is essential to know what your specific genetic markers are so that you and your physician can make informed choices about your treatment options. Advances in genetics—classifying high- and standard-risk disease—have refined knowledge about myeloma and are bringing the field closer to realizing personalized, precision medicine.
Three world class myeloma experts discussed what patients should understand about their genetics in the Myeloma Crowd Round Table Interactive Webcast held on July 25, 2020:
Brian Van Ness, PhD, University of Minnesota, Minneapolis: Myeloma Genetics is Personal
- Heterogeneity: differences are inherent in myeloma
- Myeloma evolves over the course of the disease, subgroups can be identified
- Genetics make every tumor unique, are ordered make every individual unique
- DNA expresses genes which are translated into proteins that govern what a cell does
- Genes “get messed up” and create mutations, can over produce mutations or normal functions
- Sequencing genomes (a genome is the sum of genetics in an organism)
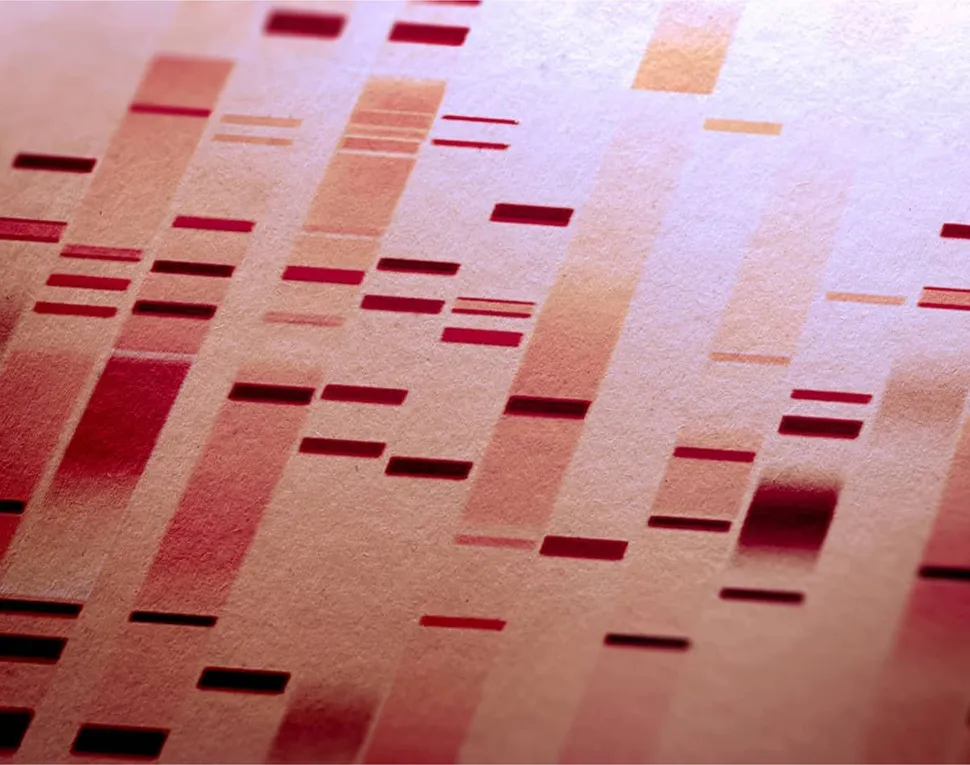
- Technology to sequence an individual’s genome has become cost effective and rapid
- Myeloma is genetically unstable
- DNA changes determine risk and can continue to change with treatment
- Not all myeloma cells respond to treatment, they evolve to become resistant to treatment
- Chromosomes: Every person normally has 22 pairs of chromosomes plus 1 x or y chromosome which determines sex
- In myeloma, abnormalities in chromosomes sometimes over-produce (hyperdiploidy), cause of half of some pairs to disappear (deletion), or part of one can change places, or rearrange, with part of another (translocation)
- Genetic mutations: Some are more common in myeloma, identifying them provides insight to target therapies
- Genomic evolution
- Clones—groups of cells with a common origin—change over time with differing treatments
- Diagnostics are improving to determine both changes and how these changes occur
- Gene expression: Determining how to identify different genes and how they work together to create disease characteristics
- High expression means “lots of bad is being produced”
- Low expression means “not very much is being produced”
- Genetic profiling: Can profile of the genes be correlated to how myeloma treatment might predict response?
- Can “good” responders be separated from “bad” responders?
- This is the goal of personalized medicine
Faith Davies, MBBCh, MRCP, MD, FRCPath, Perlmutter Cancer Center, New York University, New York, NY: Risk Classifications in Myeloma
- Prognostic factors: can outcomes be predicted at diagnosis?
- Standard-risk and high-risk myeloma, low-risk is not considered a category anymore
- Assessing risk
- Dependent on age, fitness, other diseases (comorbidities), frail/not frail
- How much myeloma? Where is it in the body? Effect on organs?
- Genetics have to be considered with other issues, not in isolation
- Chromosomal changes
- In number: amplification (amp or gain) or deletions (del), three copies (trisomies)
- In structure: common translocations are found in chromosome 14
- In code: deletion or gain in small part of chromosome; changes in RAS gene or p53 gene common in myeloma
- Variety of tests available, getting more precise: a reason a specialist matters
- Standard-risk: hyperdiploidy, t(11;14)
- Adverse or high-risk: t(4;14), t(14;16), t(14;20), Del17p, Gain1q
- Possible to have certain abnormalities
- Some have an affinity to other abnormalities, such as chromosome 13 which has an affinity to chromosome 14
- A continuously changing field, what is considered high-risk today may not be tomorrow
- Tests to determine risk stratification
- FISH
- Combining FISH and blood test
- Gene expression profiling (GEP)
- All are different, one can be standard-risk in one test, high-risk in a different one
- One high-risk factor does not necessarily mean high-risk disease, another reason why a specialist matters
- Prognostic is not predictive
Sikander Ailawadhi, MD, Mayo Clinic, Jacksonville, FL: Myeloma Sub-Population Genetic Characteristics
- Overview of major cytogenetic abnormalities in myeloma
- Racial variability and disparities
- Socio-cultural and economic determinants play a major role
- Age, gender, hereditary factors are non-modifiable
- African American: general myeloma patient characteristics
- Have fewer translocations, so disease may be less aggressive
- Lower incidence of high-risk genetic mutations
- Mayo study found difference in mutation frequency
- Del17p less frequent, t(11;14) more frequent
- Variability in cytogenetic testing
- Differences of conventional karyotyping vs FISH
- Activity of testing varies greatly among institutions
- Even tests for numbers of mutations varies within institutions
- Important for patients to find out what kind of testing is done
- Treatment guidelines overview (focusing on mSMART)
- Common regimens for newly diagnosed myeloma, transplant ineligible and eligible
- Refractory and relapsed myeloma not covered in this presentation: high variability that has to be discussed with physicians
- Genetic testing in myeloma is standard of care
- Variability in testing is lessening, but too early for comprehensive standards
Audience Questions & Answers:
- 0:45 - For a patient with high-risk smoldering myeloma and t(11;14) with no other genetic features, with respect to venetoclax [which specifically targets t(11;14)], what should one do? Join the ASCENT trial, or another high-risk smoldering trial, or consider using venetoclax up front?
- 7:25 - Is there an expert consensus relating to Gain1q and how relevant the number of extra copies are? Are there any immunotherapies that are particularly targeted to Gain1q?
- 15:18 - Is peripheral blood sufficient for genetic analysis as compared to bone marrow tests?
- 18:39 - Are there known reasons why African Americans and people of African descent are diagnosed, statistically, with myeloma at a younger age? And could the better outcomes be related to the fact that they are younger when diagnosed?
- 23:00 - When one is in remission, do these abnormalities disappear? Are these chromosomal abnormalities the same thing as mutations?
- 25:29 - Has any correlation been found between minimal residual disease (MRD) testing and genomic profiles?
- 28:52 - Please clarify that high-risk smoldering myeloma is not the same thing as high-risk myeloma genetics.
- 30:59 - What tests should one ask a doctor to be done at relapse? Which is most valuable?
- 39:00 - With respect to nonsecretory myeloma, which does not produce a monoclonal protein to measure, requiring bone marrow biopsies, or light-chain-only myeloma, are the genetics different for those types of myelomas or are they the same?
- 41:32 - Re: t(14;20) is there any new information of this, which affects about 5% of myeloma patients? And the same about del1p, which is not common. [Discussion also goes into other high-risk genetic markers.]
Thanks to our Round Table sponsors
 .
.  .
. 
 .
. 
 .
.  .
. 


Knowing about genetics is not just for scientists anymore. To be an informed myeloma patient it is essential to know what your specific genetic markers are so that you and your physician can make informed choices about your treatment options. Advances in genetics—classifying high- and standard-risk disease—have refined knowledge about myeloma and are bringing the field closer to realizing personalized, precision medicine.
Three world class myeloma experts discussed what patients should understand about their genetics in the Myeloma Crowd Round Table Interactive Webcast held on July 25, 2020:
Brian Van Ness, PhD, University of Minnesota, Minneapolis: Myeloma Genetics is Personal
- Heterogeneity: differences are inherent in myeloma
- Myeloma evolves over the course of the disease, subgroups can be identified
- Genetics make every tumor unique, are ordered make every individual unique
- DNA expresses genes which are translated into proteins that govern what a cell does
- Genes “get messed up” and create mutations, can over produce mutations or normal functions
- Sequencing genomes (a genome is the sum of genetics in an organism)
- Technology to sequence an individual’s genome has become cost effective and rapid
- Myeloma is genetically unstable
- DNA changes determine risk and can continue to change with treatment
- Not all myeloma cells respond to treatment, they evolve to become resistant to treatment
- Chromosomes: Every person normally has 22 pairs of chromosomes plus 1 x or y chromosome which determines sex
- In myeloma, abnormalities in chromosomes sometimes over-produce (hyperdiploidy), cause of half of some pairs to disappear (deletion), or part of one can change places, or rearrange, with part of another (translocation)
- Genetic mutations: Some are more common in myeloma, identifying them provides insight to target therapies
- Genomic evolution
- Clones—groups of cells with a common origin—change over time with differing treatments
- Diagnostics are improving to determine both changes and how these changes occur
- Gene expression: Determining how to identify different genes and how they work together to create disease characteristics
- High expression means “lots of bad is being produced”
- Low expression means “not very much is being produced”
- Genetic profiling: Can profile of the genes be correlated to how myeloma treatment might predict response?
- Can “good” responders be separated from “bad” responders?
- This is the goal of personalized medicine
Faith Davies, MBBCh, MRCP, MD, FRCPath, Perlmutter Cancer Center, New York University, New York, NY: Risk Classifications in Myeloma
- Prognostic factors: can outcomes be predicted at diagnosis?
- Standard-risk and high-risk myeloma, low-risk is not considered a category anymore
- Assessing risk
- Dependent on age, fitness, other diseases (comorbidities), frail/not frail
- How much myeloma? Where is it in the body? Effect on organs?
- Genetics have to be considered with other issues, not in isolation
- Chromosomal changes
- In number: amplification (amp or gain) or deletions (del), three copies (trisomies)
- In structure: common translocations are found in chromosome 14
- In code: deletion or gain in small part of chromosome; changes in RAS gene or p53 gene common in myeloma
- Variety of tests available, getting more precise: a reason a specialist matters
- Standard-risk: hyperdiploidy, t(11;14)
- Adverse or high-risk: t(4;14), t(14;16), t(14;20), Del17p, Gain1q
- Possible to have certain abnormalities
- Some have an affinity to other abnormalities, such as chromosome 13 which has an affinity to chromosome 14
- A continuously changing field, what is considered high-risk today may not be tomorrow
- Tests to determine risk stratification
- FISH
- Combining FISH and blood test
- Gene expression profiling (GEP)
- All are different, one can be standard-risk in one test, high-risk in a different one
- One high-risk factor does not necessarily mean high-risk disease, another reason why a specialist matters
- Prognostic is not predictive
Sikander Ailawadhi, MD, Mayo Clinic, Jacksonville, FL: Myeloma Sub-Population Genetic Characteristics
- Overview of major cytogenetic abnormalities in myeloma
- Racial variability and disparities
- Socio-cultural and economic determinants play a major role
- Age, gender, hereditary factors are non-modifiable
- African American: general myeloma patient characteristics
- Have fewer translocations, so disease may be less aggressive
- Lower incidence of high-risk genetic mutations
- Mayo study found difference in mutation frequency
- Del17p less frequent, t(11;14) more frequent
- Variability in cytogenetic testing
- Differences of conventional karyotyping vs FISH
- Activity of testing varies greatly among institutions
- Even tests for numbers of mutations varies within institutions
- Important for patients to find out what kind of testing is done
- Treatment guidelines overview (focusing on mSMART)
- Common regimens for newly diagnosed myeloma, transplant ineligible and eligible
- Refractory and relapsed myeloma not covered in this presentation: high variability that has to be discussed with physicians
- Genetic testing in myeloma is standard of care
- Variability in testing is lessening, but too early for comprehensive standards
Audience Questions & Answers:
- 0:45 - For a patient with high-risk smoldering myeloma and t(11;14) with no other genetic features, with respect to venetoclax [which specifically targets t(11;14)], what should one do? Join the ASCENT trial, or another high-risk smoldering trial, or consider using venetoclax up front?
- 7:25 - Is there an expert consensus relating to Gain1q and how relevant the number of extra copies are? Are there any immunotherapies that are particularly targeted to Gain1q?
- 15:18 - Is peripheral blood sufficient for genetic analysis as compared to bone marrow tests?
- 18:39 - Are there known reasons why African Americans and people of African descent are diagnosed, statistically, with myeloma at a younger age? And could the better outcomes be related to the fact that they are younger when diagnosed?
- 23:00 - When one is in remission, do these abnormalities disappear? Are these chromosomal abnormalities the same thing as mutations?
- 25:29 - Has any correlation been found between minimal residual disease (MRD) testing and genomic profiles?
- 28:52 - Please clarify that high-risk smoldering myeloma is not the same thing as high-risk myeloma genetics.
- 30:59 - What tests should one ask a doctor to be done at relapse? Which is most valuable?
- 39:00 - With respect to nonsecretory myeloma, which does not produce a monoclonal protein to measure, requiring bone marrow biopsies, or light-chain-only myeloma, are the genetics different for those types of myelomas or are they the same?
- 41:32 - Re: t(14;20) is there any new information of this, which affects about 5% of myeloma patients? And the same about del1p, which is not common. [Discussion also goes into other high-risk genetic markers.]
Thanks to our Round Table sponsors
 .
.  .
. 
 .
. 
 .
.  .
. 



about the author
Greg Brozeit
Greg Brozeit has been with the HealthTree Foundation since 2015 when he began volunteering for the Myeloma Crowd. Prior to that he worked with Dr. Bart Barlogie and the International Myeloma Foundation, inaugurating many myeloma patient advocacy and education programs.
More on HealthTree Programs
Trending Articles
Upcoming Events




Get the Latest Multiple Myeloma Updates, Delivered to You.
By subscribing to the HealthTree newsletter, you'll receive the latest research, treatment updates, and expert insights to help you navigate your health.