Natural Killer Cells to Fight Multiple Myeloma
Scientific progress in treating multiple myeloma has been moving forward over the past few years at a speed not seen in the more distant past. We have become familiar with biologics/monoclonal antibodies (and many of us are already experiencing the benefit of products such as Darzalex/daratumumab), and are learning rapidly about CAR-T (with some of us already enrolled in one of the various MM-targeted clinical programs). There is also another kid on the block that we will hear from more and more in the near future: myeloma treatment that uses Natural Killer cells, also known as NK-cells. But what are these NK-cells?
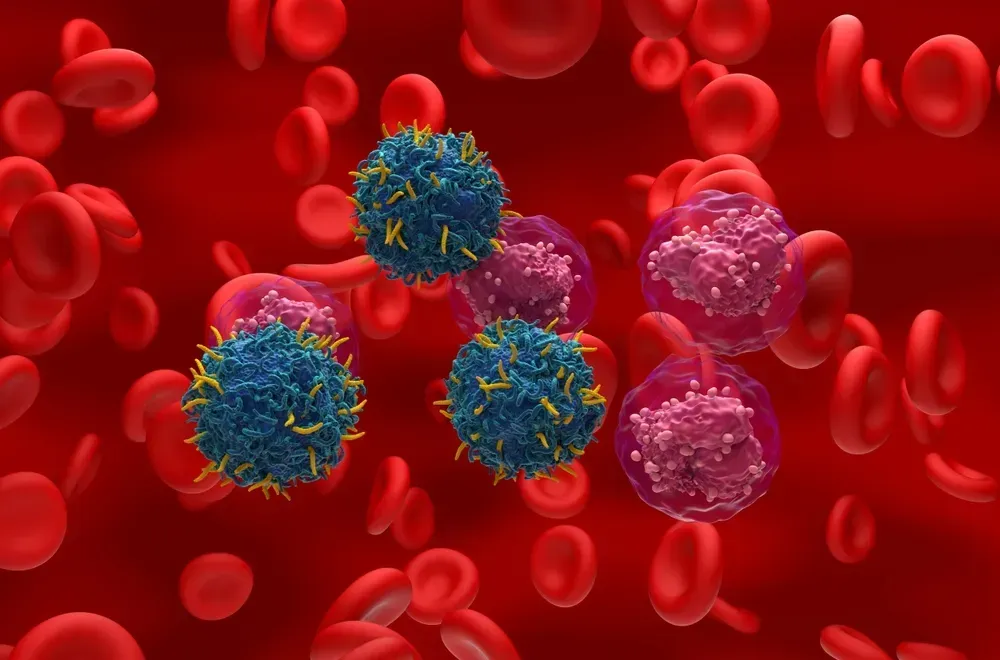
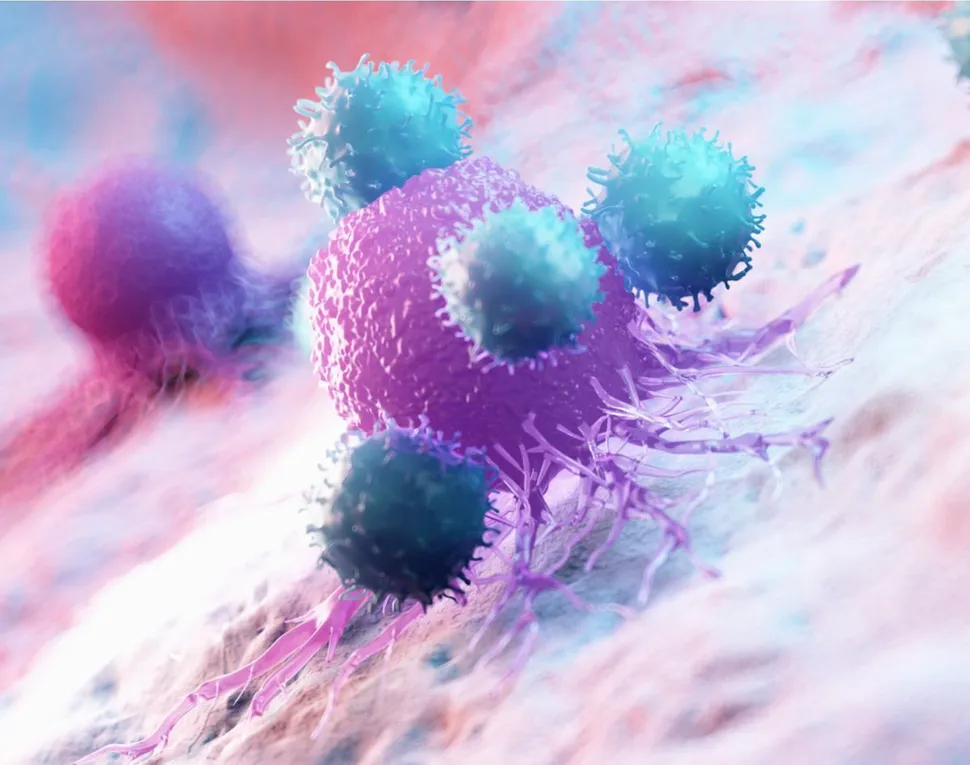
NK-cells are a type of white blood cell and they are part of our natural immune system. NK-cells were discovered in 1975 and were originally identified as lymphocytes (a kind of white blood cell) that can kill tumor cells. Since then, it has been learned that NK-cells have the unique ability to distinguish 'stressed cells' (such as tumor cells, infected cells or damaged cells) from 'normal cells'. NK-cells have tiny granules in their cytoplasm (the material inside the cell membraneexcluding the cell nucleus). These granules contain special proteins (such as perforin) as well as proteases (known as granzymes). When a NK-cell comes close to a cell slated for killing, perforin forms pores in the cell membrane of the target cell through which the granzymes and associated molecules can enter, inducing cell death.
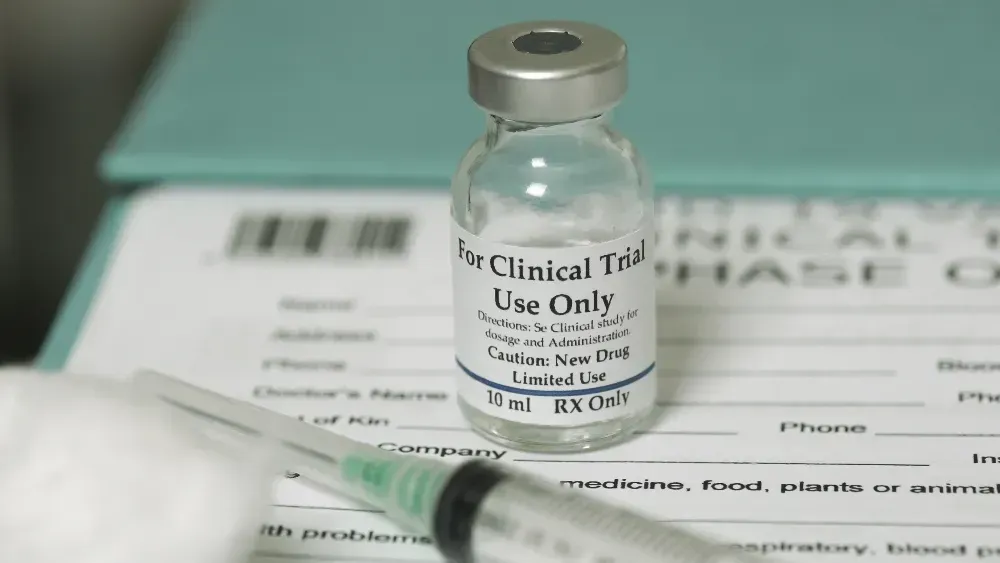
A few days ago, the company Kleo Pharmaceuticals received approval from USFDA to initiate human clinical studies with the investigational compound KP1237 in myeloma. This compound is known as a bi-specific 'antibody recruiting molecule' (ARM) that will form a bridge between the protein CD38 that is prevalent on the surface of myeloma cells and the patient's own NK-cells. This will tightly bind the NK-cells to the myeloma cells and the NK-cells can work their magic.
A nice graphic showing the interaction between KP1237 (the 'antibody recruiting molecule'), the NK-cell (shown as the 'immune cell' and the tumor cell (shown as the 'disease causing cell) can be found on the Kleo website.
There are a few things to know:
- The compound KP1237 is targeted to be used early in myeloma treatment. As indicated above, the targeted patient pool is for post-transplant, newly diagnosed patients.
- The exploratory endpoint for this study is minimal residual disease (MRD) negativity at 90-100 days post-SCT, as MRD neegativity is a good prognosticator for long-term outcomes.
- Patients cannot be treated with biologics/compounds that target CD38 (such as e.g., Darzalex) as those compounds kill NK-cells.
- KP1237 is a 'small molecule' as opposed to a 'large molecule' such as monoclonal antibodies (e.g., Darzalex). Small molecules are less complex and less expensive to manufacture compared to monoclonals. Hopefully, this will also make treatment more cost effective too, compared to biologicals.
- The company expects to start recruiting during the first half of 2020 and expects to have topline results available from the first 25-30 patients during the second half of 2021. This upcoming clinical trial is not yet listed on the clinicaltrials.gov website since FDA just issued the Investigational New Drug approval, but I expect that it will be issued soon.
Scientific progress in treating multiple myeloma has been moving forward over the past few years at a speed not seen in the more distant past. We have become familiar with biologics/monoclonal antibodies (and many of us are already experiencing the benefit of products such as Darzalex/daratumumab), and are learning rapidly about CAR-T (with some of us already enrolled in one of the various MM-targeted clinical programs). There is also another kid on the block that we will hear from more and more in the near future: myeloma treatment that uses Natural Killer cells, also known as NK-cells. But what are these NK-cells?
NK-cells are a type of white blood cell and they are part of our natural immune system. NK-cells were discovered in 1975 and were originally identified as lymphocytes (a kind of white blood cell) that can kill tumor cells. Since then, it has been learned that NK-cells have the unique ability to distinguish 'stressed cells' (such as tumor cells, infected cells or damaged cells) from 'normal cells'. NK-cells have tiny granules in their cytoplasm (the material inside the cell membraneexcluding the cell nucleus). These granules contain special proteins (such as perforin) as well as proteases (known as granzymes). When a NK-cell comes close to a cell slated for killing, perforin forms pores in the cell membrane of the target cell through which the granzymes and associated molecules can enter, inducing cell death.
A few days ago, the company Kleo Pharmaceuticals received approval from USFDA to initiate human clinical studies with the investigational compound KP1237 in myeloma. This compound is known as a bi-specific 'antibody recruiting molecule' (ARM) that will form a bridge between the protein CD38 that is prevalent on the surface of myeloma cells and the patient's own NK-cells. This will tightly bind the NK-cells to the myeloma cells and the NK-cells can work their magic.
A nice graphic showing the interaction between KP1237 (the 'antibody recruiting molecule'), the NK-cell (shown as the 'immune cell' and the tumor cell (shown as the 'disease causing cell) can be found on the Kleo website.
There are a few things to know:
- The compound KP1237 is targeted to be used early in myeloma treatment. As indicated above, the targeted patient pool is for post-transplant, newly diagnosed patients.
- The exploratory endpoint for this study is minimal residual disease (MRD) negativity at 90-100 days post-SCT, as MRD neegativity is a good prognosticator for long-term outcomes.
- Patients cannot be treated with biologics/compounds that target CD38 (such as e.g., Darzalex) as those compounds kill NK-cells.
- KP1237 is a 'small molecule' as opposed to a 'large molecule' such as monoclonal antibodies (e.g., Darzalex). Small molecules are less complex and less expensive to manufacture compared to monoclonals. Hopefully, this will also make treatment more cost effective too, compared to biologicals.
- The company expects to start recruiting during the first half of 2020 and expects to have topline results available from the first 25-30 patients during the second half of 2021. This upcoming clinical trial is not yet listed on the clinicaltrials.gov website since FDA just issued the Investigational New Drug approval, but I expect that it will be issued soon.

about the author
Paul Kleutghen
I am a patient diagnosed in 2014 with primary plasma cell leukemia (pPCL), a rare and aggressive variant of multiple myeloma and have been very fortunate to find successful treatment at the division of Cellular Therapy at the Duke University Cancer Institute. My wife, Vicki, and I have two adult children and two grandsons who are the ‘lights of our lives’. Successful treatment has allowed Vicki and I to do what we love best : traveling the world, albeit it with some extra precautions to keep infections away. My career in the pharmaceutical industry has given me insights that I am currently putting to use as an advocate to lower drug pricing, especially prices for anti-cancer drugs. I am a firm believer that staying mentally active, physically fit, compliant to our treatment regimen and taking an active interest in our disease are keys to successful treatment outcomes.
More on Treatment Advances
Trending Articles
Upcoming Events

Get the Latest Multiple Myeloma Updates, Delivered to You.
By subscribing to the HealthTree newsletter, you'll receive the latest research, treatment updates, and expert insights to help you navigate your health.
Together we care.
Together we cure.