What Is Relapsed vs. Refractory Myeloma?

There are so many myeloma phrases, terminology and acronyms that things can get incredibly confusing.
Let's talk about Relapsed Myeloma (sort of self explanatory) and Refractory Myeloma (need a refresher course on this one!).
Relapsed Myeloma
According to Dr. Sagar Lonial, MD of the Winship Cancer Institute at Emory University, Relapsed Myeloma
"specifically includes patients whose first progression occurs in the absence of any therapy following successful initial therapy."
In other words, a patient had active treatment, went off treatment and then the disease came back. The time to relapse is important - a shorter relapse period (less than six months) means a more aggressive disease.
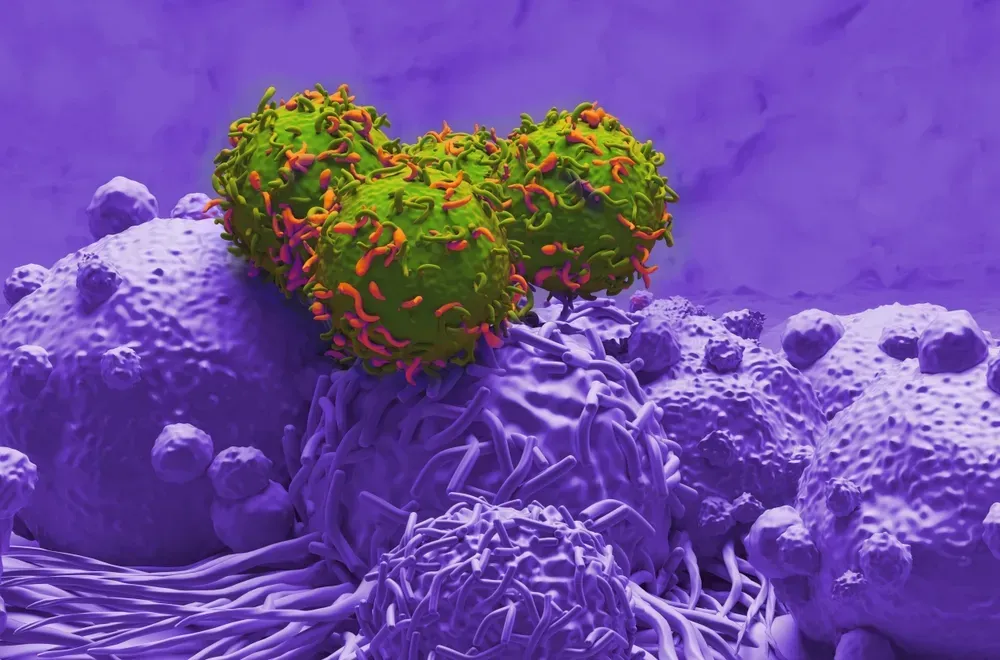
Refractory Myeloma
Dr. Damian Green, MD of the Fred Hutchinson Cancer Center, generally defines Refractory Myeloma as:
"disease that is progressing despite active treatment."
The National Cancer Institute breaks it down even further to say that there are two main types of refractory myeloma patients:
1. Primary refractory patients who never achieve a response and progress while still on induction chemotherapy (or their myeloma never responded to treatment initially).
2. Secondary refractory patients who do respond to induction chemotherapy but do not respond to treatment after relapse. (The myeloma medications worked at the beginning of treatment, but after the disease relapsed, they no longer work.)
What Now?
After the disease has relapsed or become refractory, myeloma specialists will consider many factors as they create a new game plan:
- If a partial or complete remission was achieved
- How long the remission period lasted
- How aggressively the myeloma came back
- Tolerance and effectiveness of the drugs used
- The combination of drugs used
Dr. Lonial gives a few examples of how these factors can be balanced.
- A patient with slow relapse who received a proteasome inhibitor-based treatment, followed by a stem cell transplant high-dose therapy, is a good candidate for a double-agent approach using an immunomodulatory drug and a monoclonal antibody.
- A patient with short duration remission (six months or less) is more likely to benefit from triplet or quad combination therapy, because single agents are less likely to be useful in this circumstance.
- Patients with a high-risk feature, like del 17p, t(4:14) or t(14:16), usually warrant combination therapy approaches, given the rapidity of relapses and its aggressive nature.
If your myeloma has relapsed or has become refractory, talk with your doctor to develop the best plan for you.
There are so many myeloma phrases, terminology and acronyms that things can get incredibly confusing.
Let's talk about Relapsed Myeloma (sort of self explanatory) and Refractory Myeloma (need a refresher course on this one!).
Relapsed Myeloma
According to Dr. Sagar Lonial, MD of the Winship Cancer Institute at Emory University, Relapsed Myeloma
"specifically includes patients whose first progression occurs in the absence of any therapy following successful initial therapy."
In other words, a patient had active treatment, went off treatment and then the disease came back. The time to relapse is important - a shorter relapse period (less than six months) means a more aggressive disease.
Refractory Myeloma
Dr. Damian Green, MD of the Fred Hutchinson Cancer Center, generally defines Refractory Myeloma as:
"disease that is progressing despite active treatment."
The National Cancer Institute breaks it down even further to say that there are two main types of refractory myeloma patients:
1. Primary refractory patients who never achieve a response and progress while still on induction chemotherapy (or their myeloma never responded to treatment initially).
2. Secondary refractory patients who do respond to induction chemotherapy but do not respond to treatment after relapse. (The myeloma medications worked at the beginning of treatment, but after the disease relapsed, they no longer work.)
What Now?
After the disease has relapsed or become refractory, myeloma specialists will consider many factors as they create a new game plan:
- If a partial or complete remission was achieved
- How long the remission period lasted
- How aggressively the myeloma came back
- Tolerance and effectiveness of the drugs used
- The combination of drugs used
Dr. Lonial gives a few examples of how these factors can be balanced.
- A patient with slow relapse who received a proteasome inhibitor-based treatment, followed by a stem cell transplant high-dose therapy, is a good candidate for a double-agent approach using an immunomodulatory drug and a monoclonal antibody.
- A patient with short duration remission (six months or less) is more likely to benefit from triplet or quad combination therapy, because single agents are less likely to be useful in this circumstance.
- Patients with a high-risk feature, like del 17p, t(4:14) or t(14:16), usually warrant combination therapy approaches, given the rapidity of relapses and its aggressive nature.
If your myeloma has relapsed or has become refractory, talk with your doctor to develop the best plan for you.
about the author
Jennifer Ahlstrom
Myeloma survivor, patient advocate, wife, mom of 6. Believer that patients can contribute to cures by joining HealthTree Cure Hub and joining clinical research. Founder and CEO of HealthTree Foundation.
More on Core Education
Trending Articles
Upcoming Events




Get the Latest Multiple Myeloma Updates, Delivered to You.
By subscribing to the HealthTree newsletter, you'll receive the latest research, treatment updates, and expert insights to help you navigate your health.
Together we care.
Together we cure.
3x Faster.