Does Your Gut Microbiome Affect Your Myeloma Diagnosis and Treatment?
Research published by the American Association for Cancer Research has identified bacteria and associated metabolites within the gastrointestinal microbiome that are related to positive and negative myeloma outcomes.
Understanding the Gastrointestinal (GI) Microbiome
Everyone isn’t expected to know biology topics like the GI microbiome, so let’s discuss what exactly it is.
The GI tract consists of the mouth (oral cavity), pharynx (also known as the voice box), esophagus, stomach, small intestine, large intestine, appendix, rectum, and anus. The liver and pancreas produce digestive enzymes that empty into the small intestine; therefore, they are a part of the GI tract, but the small and large intestines are where the GI microbiome is mainly contained.
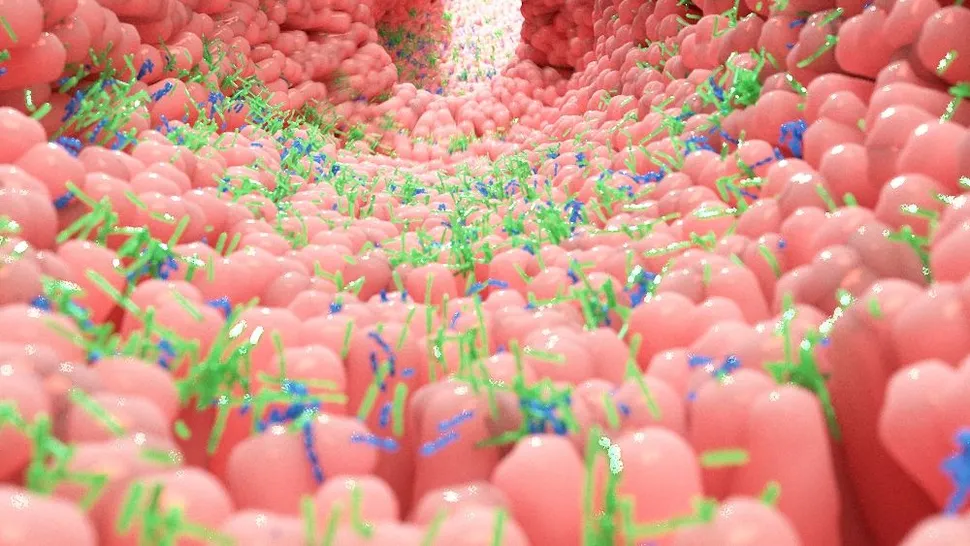
Our GI tracts are filled with bacteria, fungi, and viruses, collectively known as the gut microbiome. There is a balance between the symbiotic and small number of pathogenic (or harmful) microorganisms that coexist as the microbiome; the symbiosis of the microbiome means it is beneficial to our body and aids in the digestion of food and the production of metabolites.
However, Harvard T.H. Chan School of Public Health states, “ if there is a disturbance in that balance—brought on by infectious illnesses, certain diets, or the prolonged use of antibiotics or other bacteria-destroying medications—dysbiosis occurs, stopping these normal interactions. As a result, the body may become more susceptible to disease.”
Therefore, a premalignant or malignant diagnosis associated with myeloma may drastically affect how your GI microbiome works to benefit your health.
What Does the GI Microbiome Do?
The thought of many microorganisms living in our GI tract that support digestion sounds strange, so let us discuss how the GI microbiome maintains our body’s homeostasis.
The GI microbiome's role in the small intestine is to absorb simple sugars and introduce digestive enzymes from the pancreas and liver. More complex carbohydrates travel to the large intestine, where the GI microbiota releases digestive enzymes. Fermentation of indigestible fibers results in the synthesis of short-chain fatty acids (SCFAs); SCFAs “can be used by the body as a nutrient source but also play an important role in muscle function and possibly the prevention of chronic diseases, including certain cancers and bowel disorders.”
Without a GI microbiome, food and ingested toxins would be unable to break down or be neutralized. In addition to neutralizing toxins and digesting food, the GI microbiome synthesizes vitamins, amino acids, and SCFAs. Different areas of the intestine have different colonies of microorganisms responsible for different digestion and synthesis.
What Microorganisms Are Part of the GI Microbiome?
Now that we understand the GI microbiome and what it does, let’s go over what bacterial microorganism families compose the GI microbiome.
More than 10,000 different species of microbial organisms live in and on our bodies, and 95% of the microbiota live in our GI tract. Many bacterial microorganisms residing in the GI tract consist of Prevotella, Ruminococcus, Bacteroides, and Firmicutes; in the large intestine, a portion known as the colon lacks oxygen and has different bacterial microbes. The colon microbes are anaerobic and are called Peptostreptococcus, Bifidobacterium, Lactobacillus, and Clostridium.
Understanding the GI Microbiome in Relation to Multiple Myeloma
There is a lot of information to digest, but with all this information in mind, the research conducted by Rodriguez-Garcia et al. will be easier to understand.
Forty-three patients participated in the study; patients were either affected by monoclonal gammopathy of undetermined significance (MGUS [n=11]), smoldering multiple myeloma (SMM [n=9]), newly diagnosed multiple myeloma (NDMM [n=11]), relapsed/refractory multiple myeloma (n=6), or in complete remission (n=9).
The study was repeated with an additional sample of 62 individuals to validate the initial findings.
Each patient had blood and stool samples taken to quantify SCFAs and identify corresponding microorganisms in the GI microbiome. SCFAs in the blood serum, such as acetate, propionate, and butyrate, were quantified because SCFAs like that of butyrate found in high abundance in myeloma patients had “minimal residual disease treatment response and reduced gastrointestinal toxicity, suggesting an association between microbial signatures and patient outcome.”
Bacterial 16S ribosomal RNA gene-targeted sequencing and polymerase chain reaction (PCR) amplification were utilized to identify bacterial microorganisms in the stool samples. In other words, the bacteria’s genomic information was spliced and replicated to specify the species of bacteria present. SCFAs were quantified using multiple reaction monitoring with liquid chromatography triple quadrupole tandem mass spectrometry (LC-QQQ-MS).
The results of this study are the first to identify SCFAs, along with their corresponding bacteria, as predictors for myeloma progression and patient responses to treatment. “Bacteria involved in SCFA production, including Prevotella, Blautia, Weissella, and Agathobacter, were more represented in the premalignant or complete remission samples, and patients with higher levels of Agathobacter showed better overall survival,” and “serum levels of butyrate and propionate decreased across disease progression, and butyrate was positively associated with a better response.”
Identifying bacteria within the GI microbiome that produce SCFAs in the colon that have antiproliferative effects is potentially revolutionary in managing myeloma conditions!
How to Improve Your GI Microbiome Health
At this time, we understand that the GI microbiome is a supportive organ and can improve myeloma treatment outcomes, and specific bacteria and their metabolites are associated with the aforementioned positive outcomes. However, what do we do with this information?
Nutrition plays an enormous role in how well our GI microbiome works. As previously discussed, ingested fibers (found in fruits and vegetables) reach the colon, meeting anaerobic bacteria that ferment the fiber and produce SCFAs. Therefore, diets high in sugar, animal protein, or saturated fatty acids will reduce the amount of SCFAs produced; with limited SCFA production, myeloma conditions may persist, worsen, or reoccur.
According to MyPlate, the amount of fruits and vegetables you eat daily depends on age, sex, height, weight, and physical activity. Still, a general rule is to have half of your plate consist of fruits and vegetables. For further instruction on a well-balanced diet, visit the MyPlate website or schedule an appointment with a nutritionist or primary care physician.
Probiotics are another method of introducing beneficial bacteria to your GI microbiome; probiotics can be introduced via cultured yogurt (Greek yogurt). However, if you would instead take a probiotic supplement, it is essential to talk with your primary care physician before starting it.
Conclusion
New information will continuously roll out in the field of multiple myeloma, and positive findings like that by Rodriguez-Garcia et al. are essential in improving patient outcomes. The goal of myeloma research and articles like this is to help patients feel involved in their care.
Not everyone feels able to participate in their healthcare because healthcare professionals often use foreign and confusing terminology. As a nurse, I take it upon myself to talk with patients after a physician has spoken to them to clarify any confusion or anxieties about the information presented. Life-altering diagnoses, like that of myeloma or its premalignant precursors, can leave patients feeling overwhelmed and unable to participate in their care plan actively.
You are not alone in feeling confused or overwhelmed about your myeloma diagnosis. The HealthTree Foundation seeks to break down complicated information to empower you with the knowledge to improve your health outcomes. So, if you have any questions regarding your GI microbiome and how it can affect your myeloma, contact your PCP, oncologist, or nutritionist to see how you can nourish your GI microbiome effectively.
Research Articles and Resources
- Burton-Bethke, A. (2021, September 12). Tasty Tuesday: Finding foods for your microbiome with Dr. Urvi Shah. HealthTree Foundation for Multiple Myeloma.
- Harvard T.H. Chan: School of Public Health. (2024). The nutrition source: The microbiome.
- MyPlate U.S. Department of Agriculture. (n.d.). What is MyPlate?
- National Institute of Diabetes and Digestive and Kidney Diseases. (2017). Your digestive system & how it works.
- Nordic Biosite. (2020, June 27). World microbiome day 2020.
- Rodriguez-Garcia, A., Arroyo, A., Garcia-Vicente, R., Morales, M.L., Gomez-Gordo, R., Justo, P., Cuellar, C., Sanchez-Pina, J., Lopez, N., Alonso, R., Puig, N., Mateos, M.V., Ayala, R., Gomez-Garre, D., Martinez-Lopez, J., & Linares, M. (2024, January 11). Short-chain fatty acid production by gut microbiota predicts treatment response in multiple myeloma. American Association for Cancer Research, 1-14.
Research published by the American Association for Cancer Research has identified bacteria and associated metabolites within the gastrointestinal microbiome that are related to positive and negative myeloma outcomes.
Understanding the Gastrointestinal (GI) Microbiome
Everyone isn’t expected to know biology topics like the GI microbiome, so let’s discuss what exactly it is.
The GI tract consists of the mouth (oral cavity), pharynx (also known as the voice box), esophagus, stomach, small intestine, large intestine, appendix, rectum, and anus. The liver and pancreas produce digestive enzymes that empty into the small intestine; therefore, they are a part of the GI tract, but the small and large intestines are where the GI microbiome is mainly contained.
Our GI tracts are filled with bacteria, fungi, and viruses, collectively known as the gut microbiome. There is a balance between the symbiotic and small number of pathogenic (or harmful) microorganisms that coexist as the microbiome; the symbiosis of the microbiome means it is beneficial to our body and aids in the digestion of food and the production of metabolites.
However, Harvard T.H. Chan School of Public Health states, “ if there is a disturbance in that balance—brought on by infectious illnesses, certain diets, or the prolonged use of antibiotics or other bacteria-destroying medications—dysbiosis occurs, stopping these normal interactions. As a result, the body may become more susceptible to disease.”
Therefore, a premalignant or malignant diagnosis associated with myeloma may drastically affect how your GI microbiome works to benefit your health.
What Does the GI Microbiome Do?
The thought of many microorganisms living in our GI tract that support digestion sounds strange, so let us discuss how the GI microbiome maintains our body’s homeostasis.
The GI microbiome's role in the small intestine is to absorb simple sugars and introduce digestive enzymes from the pancreas and liver. More complex carbohydrates travel to the large intestine, where the GI microbiota releases digestive enzymes. Fermentation of indigestible fibers results in the synthesis of short-chain fatty acids (SCFAs); SCFAs “can be used by the body as a nutrient source but also play an important role in muscle function and possibly the prevention of chronic diseases, including certain cancers and bowel disorders.”
Without a GI microbiome, food and ingested toxins would be unable to break down or be neutralized. In addition to neutralizing toxins and digesting food, the GI microbiome synthesizes vitamins, amino acids, and SCFAs. Different areas of the intestine have different colonies of microorganisms responsible for different digestion and synthesis.
What Microorganisms Are Part of the GI Microbiome?
Now that we understand the GI microbiome and what it does, let’s go over what bacterial microorganism families compose the GI microbiome.
More than 10,000 different species of microbial organisms live in and on our bodies, and 95% of the microbiota live in our GI tract. Many bacterial microorganisms residing in the GI tract consist of Prevotella, Ruminococcus, Bacteroides, and Firmicutes; in the large intestine, a portion known as the colon lacks oxygen and has different bacterial microbes. The colon microbes are anaerobic and are called Peptostreptococcus, Bifidobacterium, Lactobacillus, and Clostridium.
Understanding the GI Microbiome in Relation to Multiple Myeloma
There is a lot of information to digest, but with all this information in mind, the research conducted by Rodriguez-Garcia et al. will be easier to understand.
Forty-three patients participated in the study; patients were either affected by monoclonal gammopathy of undetermined significance (MGUS [n=11]), smoldering multiple myeloma (SMM [n=9]), newly diagnosed multiple myeloma (NDMM [n=11]), relapsed/refractory multiple myeloma (n=6), or in complete remission (n=9).
The study was repeated with an additional sample of 62 individuals to validate the initial findings.
Each patient had blood and stool samples taken to quantify SCFAs and identify corresponding microorganisms in the GI microbiome. SCFAs in the blood serum, such as acetate, propionate, and butyrate, were quantified because SCFAs like that of butyrate found in high abundance in myeloma patients had “minimal residual disease treatment response and reduced gastrointestinal toxicity, suggesting an association between microbial signatures and patient outcome.”
Bacterial 16S ribosomal RNA gene-targeted sequencing and polymerase chain reaction (PCR) amplification were utilized to identify bacterial microorganisms in the stool samples. In other words, the bacteria’s genomic information was spliced and replicated to specify the species of bacteria present. SCFAs were quantified using multiple reaction monitoring with liquid chromatography triple quadrupole tandem mass spectrometry (LC-QQQ-MS).
The results of this study are the first to identify SCFAs, along with their corresponding bacteria, as predictors for myeloma progression and patient responses to treatment. “Bacteria involved in SCFA production, including Prevotella, Blautia, Weissella, and Agathobacter, were more represented in the premalignant or complete remission samples, and patients with higher levels of Agathobacter showed better overall survival,” and “serum levels of butyrate and propionate decreased across disease progression, and butyrate was positively associated with a better response.”
Identifying bacteria within the GI microbiome that produce SCFAs in the colon that have antiproliferative effects is potentially revolutionary in managing myeloma conditions!
How to Improve Your GI Microbiome Health
At this time, we understand that the GI microbiome is a supportive organ and can improve myeloma treatment outcomes, and specific bacteria and their metabolites are associated with the aforementioned positive outcomes. However, what do we do with this information?
Nutrition plays an enormous role in how well our GI microbiome works. As previously discussed, ingested fibers (found in fruits and vegetables) reach the colon, meeting anaerobic bacteria that ferment the fiber and produce SCFAs. Therefore, diets high in sugar, animal protein, or saturated fatty acids will reduce the amount of SCFAs produced; with limited SCFA production, myeloma conditions may persist, worsen, or reoccur.
According to MyPlate, the amount of fruits and vegetables you eat daily depends on age, sex, height, weight, and physical activity. Still, a general rule is to have half of your plate consist of fruits and vegetables. For further instruction on a well-balanced diet, visit the MyPlate website or schedule an appointment with a nutritionist or primary care physician.
Probiotics are another method of introducing beneficial bacteria to your GI microbiome; probiotics can be introduced via cultured yogurt (Greek yogurt). However, if you would instead take a probiotic supplement, it is essential to talk with your primary care physician before starting it.
Conclusion
New information will continuously roll out in the field of multiple myeloma, and positive findings like that by Rodriguez-Garcia et al. are essential in improving patient outcomes. The goal of myeloma research and articles like this is to help patients feel involved in their care.
Not everyone feels able to participate in their healthcare because healthcare professionals often use foreign and confusing terminology. As a nurse, I take it upon myself to talk with patients after a physician has spoken to them to clarify any confusion or anxieties about the information presented. Life-altering diagnoses, like that of myeloma or its premalignant precursors, can leave patients feeling overwhelmed and unable to participate in their care plan actively.
You are not alone in feeling confused or overwhelmed about your myeloma diagnosis. The HealthTree Foundation seeks to break down complicated information to empower you with the knowledge to improve your health outcomes. So, if you have any questions regarding your GI microbiome and how it can affect your myeloma, contact your PCP, oncologist, or nutritionist to see how you can nourish your GI microbiome effectively.
Research Articles and Resources
- Burton-Bethke, A. (2021, September 12). Tasty Tuesday: Finding foods for your microbiome with Dr. Urvi Shah. HealthTree Foundation for Multiple Myeloma.
- Harvard T.H. Chan: School of Public Health. (2024). The nutrition source: The microbiome.
- MyPlate U.S. Department of Agriculture. (n.d.). What is MyPlate?
- National Institute of Diabetes and Digestive and Kidney Diseases. (2017). Your digestive system & how it works.
- Nordic Biosite. (2020, June 27). World microbiome day 2020.
- Rodriguez-Garcia, A., Arroyo, A., Garcia-Vicente, R., Morales, M.L., Gomez-Gordo, R., Justo, P., Cuellar, C., Sanchez-Pina, J., Lopez, N., Alonso, R., Puig, N., Mateos, M.V., Ayala, R., Gomez-Garre, D., Martinez-Lopez, J., & Linares, M. (2024, January 11). Short-chain fatty acid production by gut microbiota predicts treatment response in multiple myeloma. American Association for Cancer Research, 1-14.

about the author
Jessica Jones
My name is Jessica Jones, and I am a registered nurse licensed in Utah. I worked as a certified nursing assistant for four years, a licensed practical nurse for one year, and a registered nurse for over two years. Throughout my education and work experience, I have undergone personal hardships where members of my family have either been diagnosed or passed away from cancer. Therefore, I aim to help those in need directly or indirectly through my education and experience as a registered nurse.
More on Navigating Your Health
Trending Articles
Upcoming Events

Get the Latest Multiple Myeloma Updates, Delivered to You.
By subscribing to the HealthTree newsletter, you'll receive the latest research, treatment updates, and expert insights to help you navigate your health.
Together we care.
Together we cure.