Which Myeloma Drug will You Respond To? Mayo Clinic Scottsdale Researchers Develop New Test
Myeloma specialists and myeloma patients alike want to know which treatment will work best before they are taken. Mayo Clinic Scottsdale has developed a new test using a "direct-to-drug" screening that helps determine how certain myeloma cells (with specific biomarkers and pretreatment histories) will react to different myeloma therapies. The new test is flexible enough to accommodate new drugs as they become FDA approved and is a way to avoid using drugs that won't provide much impact. This flexibility is required with the rapidly changing environment in myeloma.
Personalized care in myeloma is especially tricky because of the differences in each myeloma patients' cells. A single patient can have an average of 5 different "types" of myeloma at diagnosis and those types can evolve over time. This is called heterogeneity. Add to that the large number of potential treatment combinations, and it becomes an art and a science to treat myeloma patients. This new test will help provide much needed guidance. Today's common treatment strategies are to use proteasome inhibitors (like Velcade or Kyprolis) and immunomodulatory drugs (like Revlimid or Pomalyst) in newly diagnosed patients, yet deep complete remission is only achieved in ~50%, and most patients ultimately relapse, due to innate and acquired drug resistance.
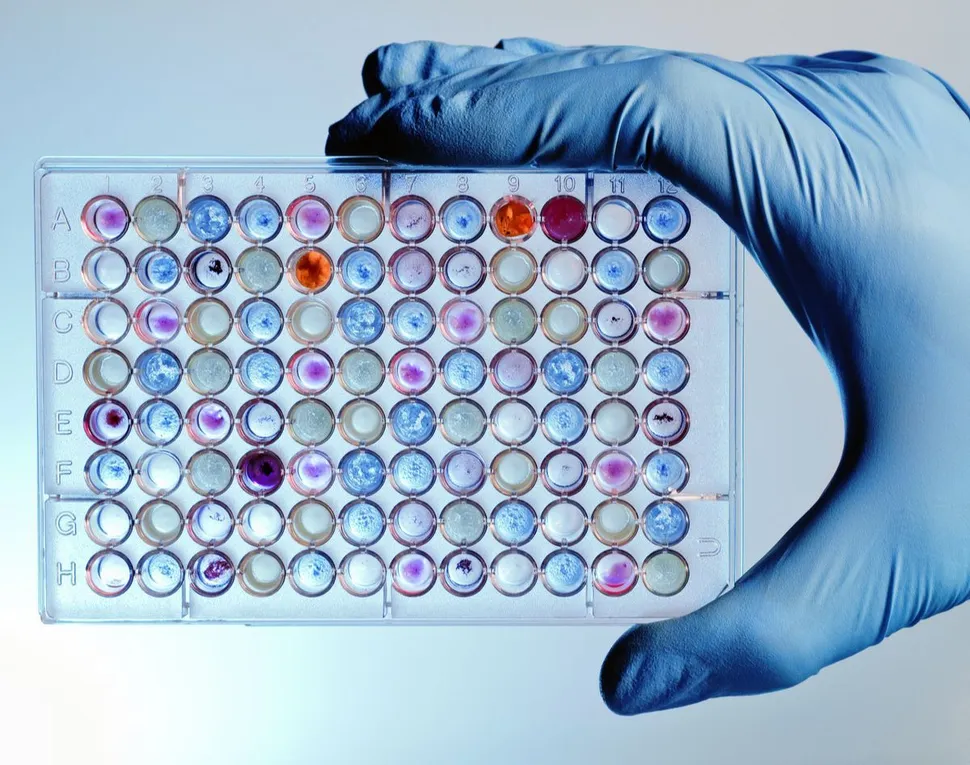
In this amazing research published in Blood Cancer Journal, the researchers led by Keith Stewart, MB, CHB (now at Princess Margaret Cancer Center) studied 76 FDA approved cancer drugs (and drugs in development) in 113 myeloma cell samples. The test was looking at associations with myeloma type, cytogenetics, genetic mutations and other profiles.
Many key findings from the research will be incredibly helpful for patients:
- In untreated myeloma samples, proteasome inhibitors, dinaciclib, selinexor, venetoclax, auranofin, and histone deacetylating agents (HDAC inhibitors) had the broadest myeloma-killing impacts
- Primary patient samples were more sensitive to carfilzomib compared to ixazomib or bortezomib
- Immunomodulators took longer to work (72 hours) whereas all other drugs took 24 hours to work
- Fifteen drugs didn't work at 24 or 72 hours including the negative control, unmetabolized cyclophosphamide
- Drug classes with more scattered impact, but often deep, sensitivities in individual samples included bromodomain inhibitors, DNA synthesis inhibitors and kinase inhibitors (KIs)
- Venetoclax was better for t(11;14) myeloma (as we already knew) but they also found that it was better for newly diagnosed patients who were standard risk and without the gain of 1q or the t(4;14)
- Patients with MYC rearrangements had lower venetoclax sensitivity
- Selinexor was more effective for patients with later relapse and more aggressive myeloma
- Selinexor was more effective for t(4;14) or 17p deletion patients. It was also better for patients with TP53 or ZFHX4 mutations
- The test could determine highly sensitive responders to dexamethasone
- 67 of the patient samples (92%) had an average of three mutations each. The most frequently mutated genes were: KRAS (36%), NRAS (22%), ATM (18%), ZFHX4 (14%), TP53 (12%), FAM46C (12%), DIS3 (11%), BRAF (10%), IRF4 (7%) and CUK4B (5%)
- Active myeloma samples were significantly more sensitive than smoldering MM (SMM) samples to all studied HDAC inhibitors, selinexor, the signal transduction inhibitors targeting ALK (ceritinib), MAPK (cobimetinib, trametinib), CDKs (dinaciclib), RTKs (sunitinib, ponatinib), and AKT (afuresertib)
- Second, we determined that later relapse MM samples, defined as >2 relapses, appeared more sensitive than untreated disease to kinase inhibition across all classes represented in the panel (26/40 inhibitors), to selinexor and four of the DNA synthesis inhibitors. Venetoclax and bromodomain inhibitors were more potent in standard genetic risk MM, while selinexor was more potent in high genetic risk myeloma samples.
- Patients with more than two relapses were more sensitive than untreated disease to kinase inhibition across all classes represented in the panel (26 out of 40 inhibitors), to selinexor and four of the DNA synthesis inhibitors.
- CDK inhibitors (dinaciclib and palbociclib) and DNA synthesis inhibitors (cladribine and clofarabine) had stronger efficacy in samples with 17p deletion
- Double hit MM samples (two high risk genetic mutations) had lower sensitivity than single hit, high-risk samples to cabozantinib, pazopanib, ponatinib, and vorinostat
- Triple hit MM samples (three high risk genetic mutations) appeared exquisitely sensitive to seven KIs, CPI0610, and raloxifene
- Patients with mutations of ACTG1, BRAF, NRAS, KRAS, TGFBR2, and ATM genes had worse response to the drugs
- Patients with mutations of IDH2, IRF4, and TLR4 had better response to the drugs
- Patients with the IRF4 mutation had better outcomes and responded better to MAPK and ALK inhibitors
- One hyperdiploid patient (extra chromosomes) did not have the 11;14 translocation but was treated with venetoclax immediately after the drug screen. This patient was highly relapsed after receiving lenalidomide, pomalidomide, bortezomib, carfilzomib, and daratumumab. "Unexpectedly, given the lack of t(11;14), venetoclax was the most potent agent within the screen (AUC of 0.3277). The patient was treated with venetoclax, achieving a partial response that lasted for ten months. This case exemplifies the significant clinical impact that ex vivo drug screening can have for drug selection and clinical outcome, especially in advanced stage of disease with limited therapeutic options."
The test has short turnaround time and would be appealing to routine clinical practice but note that the test was not able to screen immune therapies, such as monoclonal antibodies and checkpoint inhibitors, which have shown promising anti-myeloma activity.
This information is so valuable for patients and can help determine which drugs will be the most effective for different patients at diagnosis and again at relapse. It will help patients avoid treatments that won't provide benefit and will help test both single and combination therapies using individual patient tumor cells.
Dr. Leif Bergsagel noted:
“For the first time this assay will allow us to tailor therapy to individual patients. Right now it is most promising to identify patients likely to respond to venetoclax, expanding the use of the drug beyond patients with t(11;14). “
We look forward to hearing more about this test and its use in the myeloma clinic!
Myeloma specialists and myeloma patients alike want to know which treatment will work best before they are taken. Mayo Clinic Scottsdale has developed a new test using a "direct-to-drug" screening that helps determine how certain myeloma cells (with specific biomarkers and pretreatment histories) will react to different myeloma therapies. The new test is flexible enough to accommodate new drugs as they become FDA approved and is a way to avoid using drugs that won't provide much impact. This flexibility is required with the rapidly changing environment in myeloma.
Personalized care in myeloma is especially tricky because of the differences in each myeloma patients' cells. A single patient can have an average of 5 different "types" of myeloma at diagnosis and those types can evolve over time. This is called heterogeneity. Add to that the large number of potential treatment combinations, and it becomes an art and a science to treat myeloma patients. This new test will help provide much needed guidance. Today's common treatment strategies are to use proteasome inhibitors (like Velcade or Kyprolis) and immunomodulatory drugs (like Revlimid or Pomalyst) in newly diagnosed patients, yet deep complete remission is only achieved in ~50%, and most patients ultimately relapse, due to innate and acquired drug resistance.
In this amazing research published in Blood Cancer Journal, the researchers led by Keith Stewart, MB, CHB (now at Princess Margaret Cancer Center) studied 76 FDA approved cancer drugs (and drugs in development) in 113 myeloma cell samples. The test was looking at associations with myeloma type, cytogenetics, genetic mutations and other profiles.
Many key findings from the research will be incredibly helpful for patients:
- In untreated myeloma samples, proteasome inhibitors, dinaciclib, selinexor, venetoclax, auranofin, and histone deacetylating agents (HDAC inhibitors) had the broadest myeloma-killing impacts
- Primary patient samples were more sensitive to carfilzomib compared to ixazomib or bortezomib
- Immunomodulators took longer to work (72 hours) whereas all other drugs took 24 hours to work
- Fifteen drugs didn't work at 24 or 72 hours including the negative control, unmetabolized cyclophosphamide
- Drug classes with more scattered impact, but often deep, sensitivities in individual samples included bromodomain inhibitors, DNA synthesis inhibitors and kinase inhibitors (KIs)
- Venetoclax was better for t(11;14) myeloma (as we already knew) but they also found that it was better for newly diagnosed patients who were standard risk and without the gain of 1q or the t(4;14)
- Patients with MYC rearrangements had lower venetoclax sensitivity
- Selinexor was more effective for patients with later relapse and more aggressive myeloma
- Selinexor was more effective for t(4;14) or 17p deletion patients. It was also better for patients with TP53 or ZFHX4 mutations
- The test could determine highly sensitive responders to dexamethasone
- 67 of the patient samples (92%) had an average of three mutations each. The most frequently mutated genes were: KRAS (36%), NRAS (22%), ATM (18%), ZFHX4 (14%), TP53 (12%), FAM46C (12%), DIS3 (11%), BRAF (10%), IRF4 (7%) and CUK4B (5%)
- Active myeloma samples were significantly more sensitive than smoldering MM (SMM) samples to all studied HDAC inhibitors, selinexor, the signal transduction inhibitors targeting ALK (ceritinib), MAPK (cobimetinib, trametinib), CDKs (dinaciclib), RTKs (sunitinib, ponatinib), and AKT (afuresertib)
- Second, we determined that later relapse MM samples, defined as >2 relapses, appeared more sensitive than untreated disease to kinase inhibition across all classes represented in the panel (26/40 inhibitors), to selinexor and four of the DNA synthesis inhibitors. Venetoclax and bromodomain inhibitors were more potent in standard genetic risk MM, while selinexor was more potent in high genetic risk myeloma samples.
- Patients with more than two relapses were more sensitive than untreated disease to kinase inhibition across all classes represented in the panel (26 out of 40 inhibitors), to selinexor and four of the DNA synthesis inhibitors.
- CDK inhibitors (dinaciclib and palbociclib) and DNA synthesis inhibitors (cladribine and clofarabine) had stronger efficacy in samples with 17p deletion
- Double hit MM samples (two high risk genetic mutations) had lower sensitivity than single hit, high-risk samples to cabozantinib, pazopanib, ponatinib, and vorinostat
- Triple hit MM samples (three high risk genetic mutations) appeared exquisitely sensitive to seven KIs, CPI0610, and raloxifene
- Patients with mutations of ACTG1, BRAF, NRAS, KRAS, TGFBR2, and ATM genes had worse response to the drugs
- Patients with mutations of IDH2, IRF4, and TLR4 had better response to the drugs
- Patients with the IRF4 mutation had better outcomes and responded better to MAPK and ALK inhibitors
- One hyperdiploid patient (extra chromosomes) did not have the 11;14 translocation but was treated with venetoclax immediately after the drug screen. This patient was highly relapsed after receiving lenalidomide, pomalidomide, bortezomib, carfilzomib, and daratumumab. "Unexpectedly, given the lack of t(11;14), venetoclax was the most potent agent within the screen (AUC of 0.3277). The patient was treated with venetoclax, achieving a partial response that lasted for ten months. This case exemplifies the significant clinical impact that ex vivo drug screening can have for drug selection and clinical outcome, especially in advanced stage of disease with limited therapeutic options."
The test has short turnaround time and would be appealing to routine clinical practice but note that the test was not able to screen immune therapies, such as monoclonal antibodies and checkpoint inhibitors, which have shown promising anti-myeloma activity.
This information is so valuable for patients and can help determine which drugs will be the most effective for different patients at diagnosis and again at relapse. It will help patients avoid treatments that won't provide benefit and will help test both single and combination therapies using individual patient tumor cells.
Dr. Leif Bergsagel noted:
“For the first time this assay will allow us to tailor therapy to individual patients. Right now it is most promising to identify patients likely to respond to venetoclax, expanding the use of the drug beyond patients with t(11;14). “
We look forward to hearing more about this test and its use in the myeloma clinic!
about the author
Jennifer Ahlstrom
Myeloma survivor, patient advocate, wife, mom of 6. Believer that patients can contribute to cures by joining HealthTree Cure Hub and joining clinical research. Founder and CEO of HealthTree Foundation.
More on Treatment Advances
Trending Articles
Upcoming Events




Get the Latest Multiple Myeloma Updates, Delivered to You.
By subscribing to the HealthTree newsletter, you'll receive the latest research, treatment updates, and expert insights to help you navigate your health.
Together we care.
Together we cure.
3x Faster.