Tri-Specific Antibodies and the Fight Against Multiple Myeloma
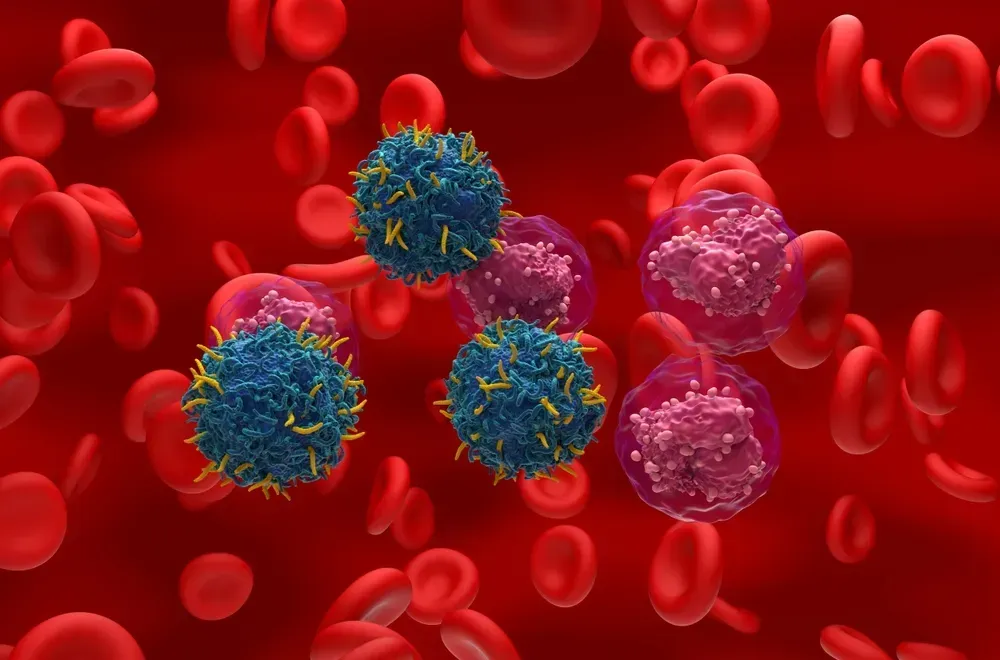
Those of us who already have Darzalex as part of our multiple myeloma treatment will unquestionably be familiar with the term ‘monoclonal antibody’ (mAb). The monoclonals are antibodies that target one specific protein (CD38) that tends to be amply found on the surface of myeloma cells. The rapid growth of the inclusion of Darzalex as a weapon against myeloma, at various stages of our disease, is ample evidence of the value of this product.
More recently we have also seen the introduction of bi-specific antibodies: products that target multiple targets, typically one on the myeloma cell and one on a T-cell that is being marshalled to ‘kill’ the myeloma cell. Unfortunately, these products are still only at clinical stage for myeloma, but chances are good that, at least one and possibly two, may be approved in the year 2020. Phase III clinical trials for several products are being wrapped up and I am quite convinced that regulatory submissions will be made in the US, EU and Japan in the not too distant future. These products fall into the realm of the CAR-T technologies and may come with some of the luggage that has been seen in the administration of CAR-T’s in other hematological cancers (such as one of the acute leukemias and several variants of Non Hodgkins Lymphomas). Problems reported in CAR-T are the release of toxicities post infusion (called cytokine release) and the ‘short’ duration of the efficacy of the treatment in some patients.
An interesting paper was just published in the Journal Nature that introduces us to the world of tri-specific antibodies (tsAb) : at product that targets one protein on the myeloma cell (CD 38) but that targets two proteins present on the surface of T-cells (CD3 and CD28) that have VERY different functions in fighting myeloma. A short and very readable summary of this discovery is available that you may wish to check out (and this has a nice graphic that makes things easier to understand. Unfortunately, this graphic cannot be included here for copyright reasons.) For those who are more interested in the science about it all, want to learn more about myeloma and the importance of T-cells at the cell level can also go to the full journal article that is peppered with all kinds of interesting charts and figures, especially the eye-popping figure 6 that is a MUST SEE. This figure shows the complex structure of the construct of the tri-specific antibody and how it latches onto T-cells and myeloma cells.
You may raise the question about the purpose of the three targeted proteins. I will do my best to explain. The overall purpose of the engineered construct is to bring the myeloma cell in close proximity to a T-cell, so that the T-cell can effectively kill the myeloma cell.
- The CD38 protein on the surface of the myeloma cell provides a mechanism for the tsAb to latch onto the myeloma cell.
- The CD3 protein ‘is part of the T-cell receptor (TCR), which recognizes abnormal cells by binding molecules called antigens. The binding of CD3 by the [tsAb] antibody drives T-cell activation (without requiring antigen recognition by the TCR), which leads to the killing of the myeloma cell and the production and release of toxic cytokine molecules.’ [emphasis added).
- ‘Binding of CD28 protein by the [tsAb] antibody drives expression of the protein[s] [that] blocks T-cell death, which might otherwise occur if there was prolonged TCR activation in the absence of CD28 stimulation by the antibody.’ In other words, binding of the CD28 gives the T-cell longer ‘fighting power’ against our myeloma compared to other bi-specific antibodies (including several CAR-T’s either already on the market or in current clinical development).
At this stage of research, no human data are available, but the animal data are very encouraging.
- The augmented activation of T-cells increased the proliferation of T-cells and the expression of the proteins that that stop/slow down the dying off of the T-cells that do the work of killing the myeloma cells.
- The presence of the CD28 also increased the ability of T-cells to kill different types of myeloma cells ‘even at the lowest dosage level’(giving this tsAb the potential for broader use in myeloma treatment).
- ‘The main limitation of this study is that the risk of a side effect called cytokine release syndrome (CRS), which can occur if the immune system is highly stimulated, is unknown. In CRS, the simultaneous activation of many T cells causes excessive release of signalling molecules called cytokines from cells of the immune system, which drives inflammation. CRS can occur with bispecific antibodies and with CAR-T. It typically manifests as fever, but can progress to fatal multi-organ failure in severe cases. [emphasis added]
- The journal article also notes that the incidence and the severity of CRS were lower when the tsAb was administered subcutaneously (simple injection under the skin) as opposed to administered via IV infusion.
In a nutshell, this discovery will hopefully become a valuable addition to the options available to us in the future. Keep up the optimism in the fight against our multiple myeloma!
Those of us who already have Darzalex as part of our multiple myeloma treatment will unquestionably be familiar with the term ‘monoclonal antibody’ (mAb). The monoclonals are antibodies that target one specific protein (CD38) that tends to be amply found on the surface of myeloma cells. The rapid growth of the inclusion of Darzalex as a weapon against myeloma, at various stages of our disease, is ample evidence of the value of this product.
More recently we have also seen the introduction of bi-specific antibodies: products that target multiple targets, typically one on the myeloma cell and one on a T-cell that is being marshalled to ‘kill’ the myeloma cell. Unfortunately, these products are still only at clinical stage for myeloma, but chances are good that, at least one and possibly two, may be approved in the year 2020. Phase III clinical trials for several products are being wrapped up and I am quite convinced that regulatory submissions will be made in the US, EU and Japan in the not too distant future. These products fall into the realm of the CAR-T technologies and may come with some of the luggage that has been seen in the administration of CAR-T’s in other hematological cancers (such as one of the acute leukemias and several variants of Non Hodgkins Lymphomas). Problems reported in CAR-T are the release of toxicities post infusion (called cytokine release) and the ‘short’ duration of the efficacy of the treatment in some patients.
An interesting paper was just published in the Journal Nature that introduces us to the world of tri-specific antibodies (tsAb) : at product that targets one protein on the myeloma cell (CD 38) but that targets two proteins present on the surface of T-cells (CD3 and CD28) that have VERY different functions in fighting myeloma. A short and very readable summary of this discovery is available that you may wish to check out (and this has a nice graphic that makes things easier to understand. Unfortunately, this graphic cannot be included here for copyright reasons.) For those who are more interested in the science about it all, want to learn more about myeloma and the importance of T-cells at the cell level can also go to the full journal article that is peppered with all kinds of interesting charts and figures, especially the eye-popping figure 6 that is a MUST SEE. This figure shows the complex structure of the construct of the tri-specific antibody and how it latches onto T-cells and myeloma cells.
You may raise the question about the purpose of the three targeted proteins. I will do my best to explain. The overall purpose of the engineered construct is to bring the myeloma cell in close proximity to a T-cell, so that the T-cell can effectively kill the myeloma cell.
- The CD38 protein on the surface of the myeloma cell provides a mechanism for the tsAb to latch onto the myeloma cell.
- The CD3 protein ‘is part of the T-cell receptor (TCR), which recognizes abnormal cells by binding molecules called antigens. The binding of CD3 by the [tsAb] antibody drives T-cell activation (without requiring antigen recognition by the TCR), which leads to the killing of the myeloma cell and the production and release of toxic cytokine molecules.’ [emphasis added).
- ‘Binding of CD28 protein by the [tsAb] antibody drives expression of the protein[s] [that] blocks T-cell death, which might otherwise occur if there was prolonged TCR activation in the absence of CD28 stimulation by the antibody.’ In other words, binding of the CD28 gives the T-cell longer ‘fighting power’ against our myeloma compared to other bi-specific antibodies (including several CAR-T’s either already on the market or in current clinical development).
At this stage of research, no human data are available, but the animal data are very encouraging.
- The augmented activation of T-cells increased the proliferation of T-cells and the expression of the proteins that that stop/slow down the dying off of the T-cells that do the work of killing the myeloma cells.
- The presence of the CD28 also increased the ability of T-cells to kill different types of myeloma cells ‘even at the lowest dosage level’(giving this tsAb the potential for broader use in myeloma treatment).
- ‘The main limitation of this study is that the risk of a side effect called cytokine release syndrome (CRS), which can occur if the immune system is highly stimulated, is unknown. In CRS, the simultaneous activation of many T cells causes excessive release of signalling molecules called cytokines from cells of the immune system, which drives inflammation. CRS can occur with bispecific antibodies and with CAR-T. It typically manifests as fever, but can progress to fatal multi-organ failure in severe cases. [emphasis added]
- The journal article also notes that the incidence and the severity of CRS were lower when the tsAb was administered subcutaneously (simple injection under the skin) as opposed to administered via IV infusion.
In a nutshell, this discovery will hopefully become a valuable addition to the options available to us in the future. Keep up the optimism in the fight against our multiple myeloma!

about the author
Paul Kleutghen
I am a patient diagnosed in 2014 with primary plasma cell leukemia (pPCL), a rare and aggressive variant of multiple myeloma and have been very fortunate to find successful treatment at the division of Cellular Therapy at the Duke University Cancer Institute. My wife, Vicki, and I have two adult children and two grandsons who are the ‘lights of our lives’. Successful treatment has allowed Vicki and I to do what we love best : traveling the world, albeit it with some extra precautions to keep infections away. My career in the pharmaceutical industry has given me insights that I am currently putting to use as an advocate to lower drug pricing, especially prices for anti-cancer drugs. I am a firm believer that staying mentally active, physically fit, compliant to our treatment regimen and taking an active interest in our disease are keys to successful treatment outcomes.
More on Treatment Advances
Trending Articles
Upcoming Events




Get the Latest Multiple Myeloma Updates, Delivered to You.
By subscribing to the HealthTree newsletter, you'll receive the latest research, treatment updates, and expert insights to help you navigate your health.
Together we care.
Together we cure.
3x Faster.