The Myeloma Road Map To Improved Survival - GEP (Gene Expression Profiling)

What’s in your Genes? You've been diagnosed and told what stage of Multiple Myeloma you are in based on your tumor burden. Now your doctor will probably order some genetic testing to understand your “tumor biology.” Every person’s tumor biology is unique and it is imperative for you and your doctor to know as much as you can about your specific disease. Your first treatment protocol will guide and determine treatment options throughout the length of your disease. Prognostic tests are used to predict the risk of disease progression and to help guide clinical management, specifically when therapy should be initiated and how aggressive it should be. The initiation, progression and relapse of MM is influenced by multiple mutations in different pathways and genes. A number of genetic aberrations or chromosomal abnormalities (CA) have been associated with poor survival as in T (4; 14), T (14; 16) and (del17p), with the introduction of novel therapeutics, like Velcade® T(4;14). Is no longer associated with high risk disease and has been moved to the standard risk disease category, as reported on the National Cancer Institute website. The traditional approach utilizing staging, conventional cytogenetics, and FISH cannot sufficiently capture the broad spectrum of genetic abnormalities that account for the clinical outcome variation. There are two types of genetic tests that are routinely used in multiple myeloma Metaphase Cytogenetics and FISH, each with their own drawbacks See below descriptions. "Conventional" Cytogenetics or "Metaphase" Cytogenetics This was the only way a doctor could analyze chromosomes and genes for a long time. This type of analysis really only detects major problems in genetic structure. Single gene mutations cannot be seen. It is common to have a "normal" cytogenetic report by conventional cytogenetics because analysis done in metaphase, can be adversely affected by the low proliferative rate of plasma cells. As a result, cytogenetic analysis detects abnormalities in only 22-40% of cases. Fluorescence in Situ Hybridization (FISH) With FISH you can test at the single gene level and it is therefore much more sensitive. Changes that are completely invisible with conventional cytogenetics are detectable with FISH. You generally only look at one or two genes at a time with FISH. However, FISH analysis performed on bone marrow aspirates of MM patients are technically challenging because the neoplastic plasma cells may represent only a small proportion of the total nuclei present. FISH results are also variable based on the lab who performed the test, the probes that were used and the pathologist that interpreted the results. In addition to numerous reports of “false positives” many physicians have difficulty with the interpretation of the results. Reading a blog recently one patient wrote that when she asked her physician for an interpretation of her FISH test that her doctor said out right "I'm not an expert on FISH testing" and then referred her for a consult with the "transplant doctors." Limitations of current CA detection methods
| Test | Description | Limitations |
| Conventional cytogenetics (karyotype) | Genome-wide survey of chromosomal structural and numeric abnormalities | •Results subject to human error •Cannot detect submicroscopic chromosomal lesions •As many as 70% are uninformative because of low proliferation (growth) rate •Information often complementary to that provided with FISH •Time consuming |
| FISH | Uses fluorescently-labeled nucleic acid probes complementary to specific sequences on a chromosome | •Misses abnormalities not included in the probe sequence (reading frame) Technically demanding •Limited by low proliferation rate |
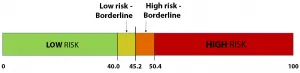
With new therapeutic choices emerging, Metaphase Cytogenetics and FISH testing methods insufficiently characterize mortality risk. Gene expression profiling (GEP) offers additional insight into specific genomic alterations and the biological pathways that control cell signaling and thus cause the different survival and treatment outcomes. GEP reveals the underlying biology of MM by quantifying the expression levels of hundreds of thousands of genes with a single assay. MyPRS®— Myeloma Prognostic Risk Signature, developed at the University of Arkansas for Medical Science (UAMS) and licensed to Signal Genetics™ (Carlsbad, CA USA), is the only clinically validated microarray-based GEP assay used to assist the management of patients with MM currently commercialized in the U.S. Validated over 30 years, 14,500 patients and 17 unique patient data sets in 4 countries. There are three components of MyPRS that differ significantly in both origin and purpose: • The 70-gene Prognostic Risk Score (GEP-70) quantifies the expression of 70 genes commonly altered in MM. Primarily prognostic, GEP-70 assesses risk of disease relapse and survival outcomes. • The Molecular Subtype interrogates 700 genes for common alterations and classifies patients into 7 distinct gene expression clusters associated with different survival outcomes. These 7 distinct MM subtypes are associated with different cytogenetic, prognostic, and treatment-response hallmarks. • The Virtual Karyotype creates a digital assessment of copy number status (i.e. normal, gain or loss) for 13 distinct chromosomes or sub-chromosomal regions based on the expression levels of 816 genes. Similar to a FISH profile. REPORT EXAMPLE: 1. MYELOMA PROGNOSTIC RISK SIGNATURE: Analysis of the prognostic 70–gene signature (GEP70) from your patient’s whole genome expression profile resulted in the following prognosis prediction.
| MyPRS Risk Score | Classification | Prognosis |
| 32.59 | Low Risk | Good |
| High Risk -Poor Prognosis | Low Risk-Good Prognosis |
| Probability of 5 year OS-38% | Probability of 5 year OS-83% |
| Your patient’s subtype: Low Bone disease (LB) |
| Key genes commonly altered in similar patients: CST6 |
| Significant genetic lesions observed in similar patients: — |
| Other characteristics of this molecular subgroup: Little or no bone disease typically seen in this subgroup of patients. CST6 overexpression. |
| Chromosome REGION | PREDICTION |
| 1p | nil |
| 1q | Amp/up |
| 1q21 | Del/down |
| 3 | nil |
| 5 | nil |
| 6q | nil |
| 7 | nil |
| 9 | Amp/up |
| 11 | nil |
| 13 | nil |
| 15 | Del/down |
| 19 | nil |
| 21 | Amp/up |
What’s in your Genes? You've been diagnosed and told what stage of Multiple Myeloma you are in based on your tumor burden. Now your doctor will probably order some genetic testing to understand your “tumor biology.” Every person’s tumor biology is unique and it is imperative for you and your doctor to know as much as you can about your specific disease. Your first treatment protocol will guide and determine treatment options throughout the length of your disease. Prognostic tests are used to predict the risk of disease progression and to help guide clinical management, specifically when therapy should be initiated and how aggressive it should be. The initiation, progression and relapse of MM is influenced by multiple mutations in different pathways and genes. A number of genetic aberrations or chromosomal abnormalities (CA) have been associated with poor survival as in T (4; 14), T (14; 16) and (del17p), with the introduction of novel therapeutics, like Velcade® T(4;14). Is no longer associated with high risk disease and has been moved to the standard risk disease category, as reported on the National Cancer Institute website. The traditional approach utilizing staging, conventional cytogenetics, and FISH cannot sufficiently capture the broad spectrum of genetic abnormalities that account for the clinical outcome variation. There are two types of genetic tests that are routinely used in multiple myeloma Metaphase Cytogenetics and FISH, each with their own drawbacks See below descriptions. "Conventional" Cytogenetics or "Metaphase" Cytogenetics This was the only way a doctor could analyze chromosomes and genes for a long time. This type of analysis really only detects major problems in genetic structure. Single gene mutations cannot be seen. It is common to have a "normal" cytogenetic report by conventional cytogenetics because analysis done in metaphase, can be adversely affected by the low proliferative rate of plasma cells. As a result, cytogenetic analysis detects abnormalities in only 22-40% of cases. Fluorescence in Situ Hybridization (FISH) With FISH you can test at the single gene level and it is therefore much more sensitive. Changes that are completely invisible with conventional cytogenetics are detectable with FISH. You generally only look at one or two genes at a time with FISH. However, FISH analysis performed on bone marrow aspirates of MM patients are technically challenging because the neoplastic plasma cells may represent only a small proportion of the total nuclei present. FISH results are also variable based on the lab who performed the test, the probes that were used and the pathologist that interpreted the results. In addition to numerous reports of “false positives” many physicians have difficulty with the interpretation of the results. Reading a blog recently one patient wrote that when she asked her physician for an interpretation of her FISH test that her doctor said out right "I'm not an expert on FISH testing" and then referred her for a consult with the "transplant doctors." Limitations of current CA detection methods
| Test | Description | Limitations |
| Conventional cytogenetics (karyotype) | Genome-wide survey of chromosomal structural and numeric abnormalities | •Results subject to human error •Cannot detect submicroscopic chromosomal lesions •As many as 70% are uninformative because of low proliferation (growth) rate •Information often complementary to that provided with FISH •Time consuming |
| FISH | Uses fluorescently-labeled nucleic acid probes complementary to specific sequences on a chromosome | •Misses abnormalities not included in the probe sequence (reading frame) Technically demanding •Limited by low proliferation rate |
With new therapeutic choices emerging, Metaphase Cytogenetics and FISH testing methods insufficiently characterize mortality risk. Gene expression profiling (GEP) offers additional insight into specific genomic alterations and the biological pathways that control cell signaling and thus cause the different survival and treatment outcomes. GEP reveals the underlying biology of MM by quantifying the expression levels of hundreds of thousands of genes with a single assay. MyPRS®— Myeloma Prognostic Risk Signature, developed at the University of Arkansas for Medical Science (UAMS) and licensed to Signal Genetics™ (Carlsbad, CA USA), is the only clinically validated microarray-based GEP assay used to assist the management of patients with MM currently commercialized in the U.S. Validated over 30 years, 14,500 patients and 17 unique patient data sets in 4 countries. There are three components of MyPRS that differ significantly in both origin and purpose: • The 70-gene Prognostic Risk Score (GEP-70) quantifies the expression of 70 genes commonly altered in MM. Primarily prognostic, GEP-70 assesses risk of disease relapse and survival outcomes. • The Molecular Subtype interrogates 700 genes for common alterations and classifies patients into 7 distinct gene expression clusters associated with different survival outcomes. These 7 distinct MM subtypes are associated with different cytogenetic, prognostic, and treatment-response hallmarks. • The Virtual Karyotype creates a digital assessment of copy number status (i.e. normal, gain or loss) for 13 distinct chromosomes or sub-chromosomal regions based on the expression levels of 816 genes. Similar to a FISH profile. REPORT EXAMPLE: 1. MYELOMA PROGNOSTIC RISK SIGNATURE: Analysis of the prognostic 70–gene signature (GEP70) from your patient’s whole genome expression profile resulted in the following prognosis prediction.
| MyPRS Risk Score | Classification | Prognosis |
| 32.59 | Low Risk | Good |
| High Risk -Poor Prognosis | Low Risk-Good Prognosis |
| Probability of 5 year OS-38% | Probability of 5 year OS-83% |
| Your patient’s subtype: Low Bone disease (LB) |
| Key genes commonly altered in similar patients: CST6 |
| Significant genetic lesions observed in similar patients: — |
| Other characteristics of this molecular subgroup: Little or no bone disease typically seen in this subgroup of patients. CST6 overexpression. |
| Chromosome REGION | PREDICTION |
| 1p | nil |
| 1q | Amp/up |
| 1q21 | Del/down |
| 3 | nil |
| 5 | nil |
| 6q | nil |
| 7 | nil |
| 9 | Amp/up |
| 11 | nil |
| 13 | nil |
| 15 | Del/down |
| 19 | nil |
| 21 | Amp/up |

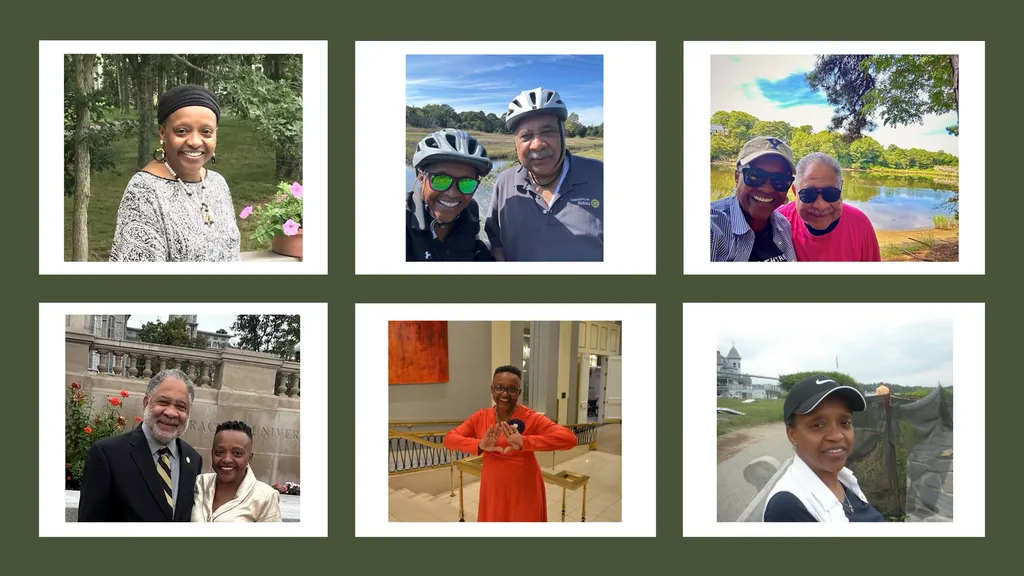
about the author
Gary Petersen
Gary is a myeloma survivor and patient advocate. His work centers around helping patients live longer by helping them to find facilities who are beating the average survival statistics. You can find Gary's site at www.myelomasurvival.com and follow him on Twitter at @grpetersen1
More on Navigating Your Health
Trending Articles
Upcoming Events




Get the Latest Multiple Myeloma Updates, Delivered to You.
By subscribing to the HealthTree newsletter, you'll receive the latest research, treatment updates, and expert insights to help you navigate your health.
Together we care.
Together we cure.
3x Faster.