Know Your AML Therapy: Venetoclax

Want to Learn More About Important AML Topics?
Sign up for HealthTree's Biweekly AML Newsletter
Dr. Alice S. Mims, acute leukemia section head and associate professor at Ohio State University Comprehensive Cancer Center shared with us information about FDA-approved venetoclax for AML treatment.
Watch the Full Event Here:
Event Summary
Dr. Mims covered several helpful topics related to the use of venetoclax in AML treatment including the study results of AML patients treated with venetoclax + hypomethylating agent (HMA) azacitidine, how the medicines work, the dosing ramp-up schedule, key things patients can expect starting treatment, solutions to certain venetoclax side effects, AML genetic mutation specific reactions to treatment, and exciting upcoming areas of study.
How the landscape of AML treatment has changed
Dr. Mims stated that before 2017, AML doctors would mainly use intensive induction therapy of 7+3 or high-dose cytarabine-based regimens. For AML patients who weren’t candidates of 7+3, they may be able to use different types of treatments like hypomethylating (HMA) agents, low-dose cytarabine, and for some AML patients, they would talk about supportive care/hospice. Below is a brief description of the FDA-approval history for AML therapy.
- 1970’s
- 7+3 induction (cytarabine/daunorubicin)
- Bone marrow transplant
- 2000 Gemtuzumab CD33 antibody
- 2002 Idarubicin an anthracycline can be used instead of daunorubicin
- 2010 Gemtuzumab withdrawn for safety concerns
- 2017
- Gemtuzumab back with adjustments made
- CPX-351, a liposomal version of cytarabine/daunorubicin
- Enasidenib an IDH inhibitor for IDH2 mutations
- Midostaurin a FLIP3 inhibitor given in combination with 7+3
- 2018
- Ivosidinib an IDH inhibitor for IDH1 mutations
- Gilteritinib, a second-generation FLIP3 inhibitor that’s approved in the relapsed/refractory setting
- Venetoclax approved for first-line therapy
- Glasdegib, a hedgehog inhibitor approved in combination with cytarabine
- 2020
- Azacitidine a hypomethylating agent (HMA) used for maintenance therapy
See here for more about these AML medicines.
One thing Dr. Mims noted was that non-intensive treatments such as HMAs don’t mean lower intensity treatment than intensive-induction chemotherapy 7+3. The HMA treatments do have side effects. She stated that hopefully as research continues, patient quality of life outcomes can keep improving.
Dr. Mims is happy about the progress made in the treatment setting for AML patients, however, she wants to continue to move the bar forward. Doctors should be thoughtful of newly diagnosed AML patients when talking about the different treatment options that may be available and what that looks like based on patients’ genetics, not just what used to be the go-to treatment before the 2017 AML medicine advancements.
How Venetoclax with Hypomethylating Agents (HMAs) or Low-dose Cytarabine Work
Venetoclax (venclexta) is a targeted therapy taken via tablets by mouth. It works by targeting cancerous AML cells (it can also bind to healthy B-cells) by blocking the BCL-2 protein, which regulates cell survival and death. Overproduction of BCL-2 is common in cancer cells, and blocking it with venetoclax causes the cancer cells to die.
Newly diagnosed AML patients who are 75 years or older, or patients who have other medical conditions that prevent the use of intensive chemotherapy (7+3) are approved to take venetoclax. Venetoclax is paired with either azacitidine (HMA), decitabine (HMA), or low-dose cytarabine.
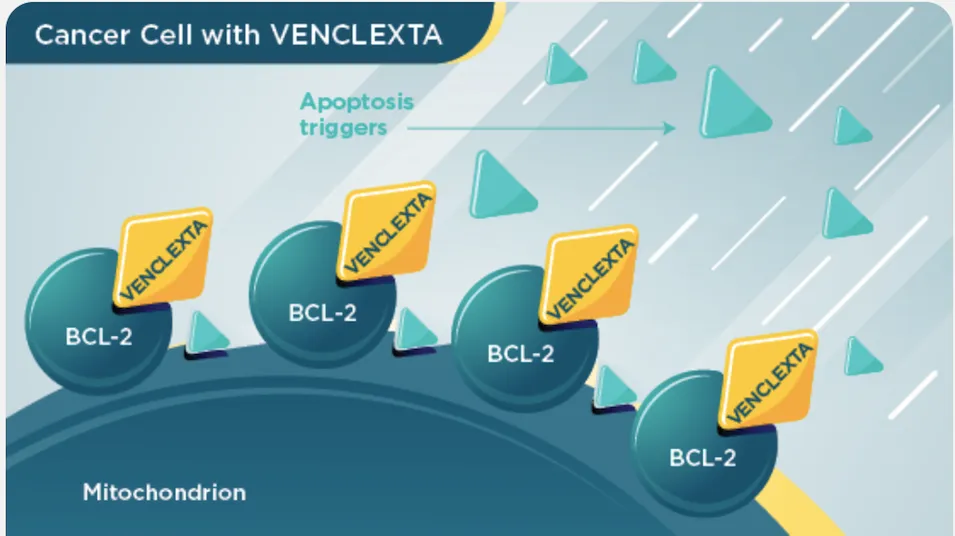
(Image Source: VENCLEXTA)
Hypomethylating Agents (HMAs)
Azacitidine and decitabine are hypomethylating agents (HMA). They work to kill cancerous AML cells by re-activating parts of the cancer cell’s instructions (DNA) that tell the cell to die. These DNA parts in the cancer cell were previously silenced when they shouldn’t have been.
Cytarabine
Cytarabine is a molecule that inserts itself into a cancer cell’s (and some healthy cells’) DNA (the cell’s instructions) messing with the cell to stop DNA from replicating itself, thus leading to cell death.
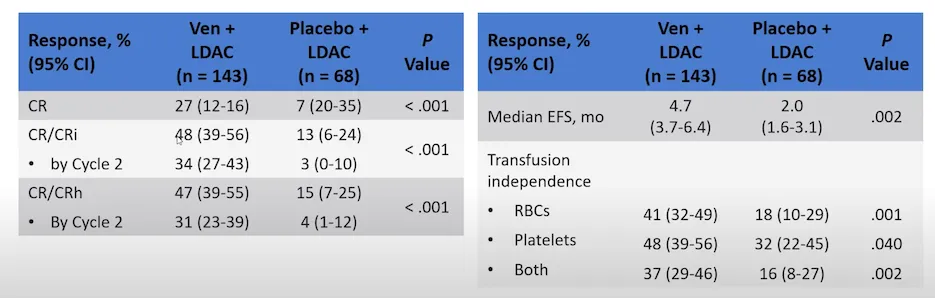
Clinical Trial Results: Venetoclax + Azacitidine (HMA) for Previously-untreated AML
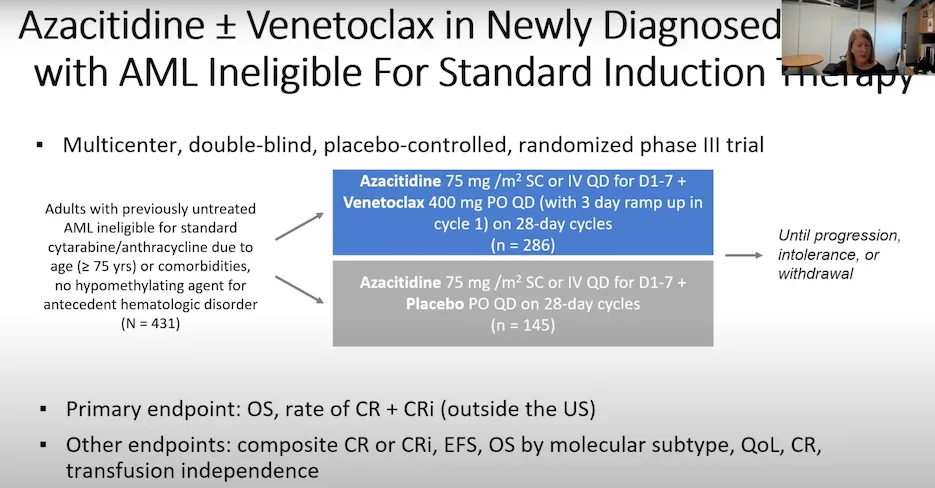
The VIALE study helped get venetoclax for AML treatment FDA-approved. The details of the study along with its results are shown in the images below.
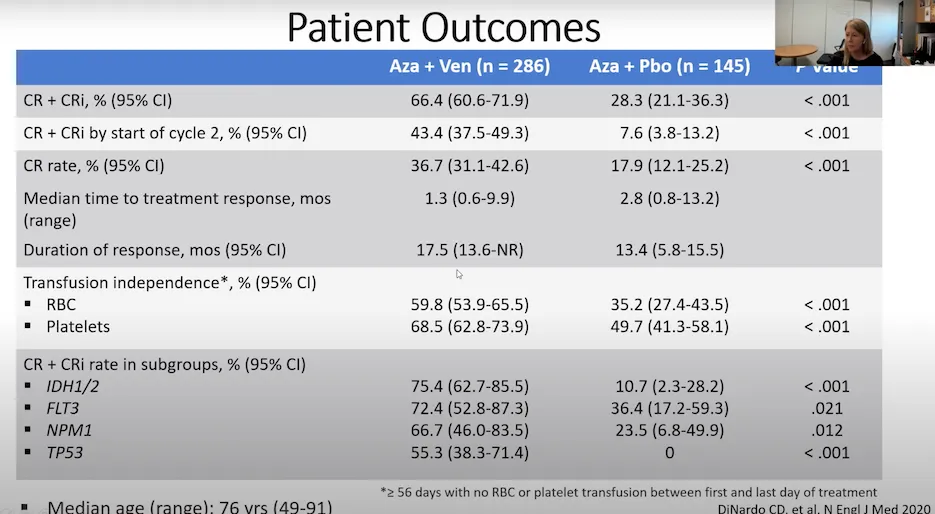
The treatment combination of venetoclax with azacitidine proved to be significantly better than using azacitidine by itself for AML patients.
These areas included:
- Complete remission rate (CR)
- AML cells are less than five percent blast in the bone marrow and the patient’s platelet and neutrophil counts have returned to normal
- Complete remission with incomplete count recovery (CRi)
- AML cells are less than five percent blast in the bone marrow. Either the platelet or neutrophil counts have recovered to normal range, but not both
- Median time to treatment response
- The amount of time it took for the cancer cells to start decreasing since the beginning of treatment
- Duration of response
- The length of time the cancer cells continued to respond to treatment and did not increase
- Transfusion independence
- Patients no longer needed to receive infusions of certain types of blood cells (red blood cells or platelets). Dr. Mims stated AML patients consider this an important quality-of-life factor
The median overall survival results from the study were:
- Venetoclax + azacitidine: 14.7 months
- Azacitidine by itself: 9.6 months
Dosing Schedule of Venetoclax + HMA ramp-up
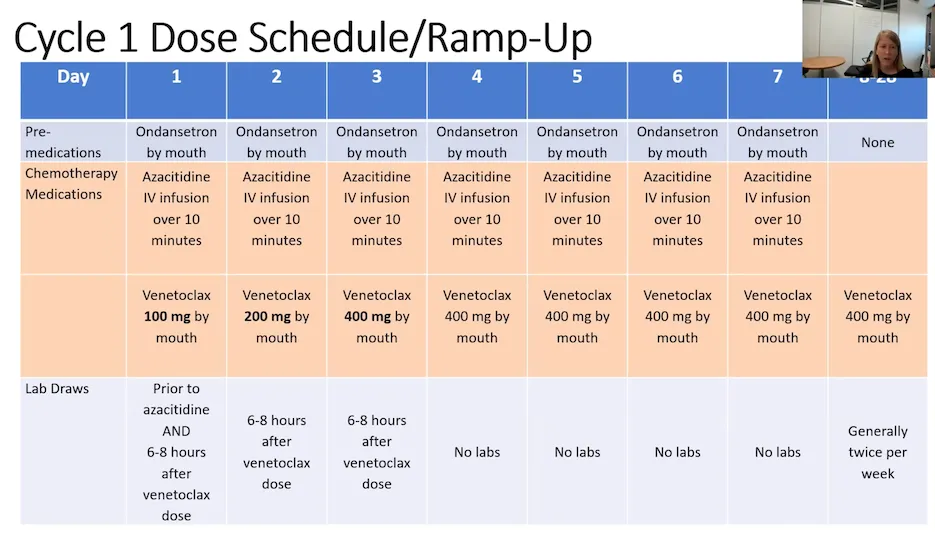
What AML patients can expect ramping up on venetoclax
- Frequent labs during the ramp-up period to check blood counts, risk of infection, and risk of tumor lysis syndrome (rare but treatable)
- The first cycle of treatment can be given inpatient or outpatient. The choice of which one is dependent on individual patient factors and the treatment institution. After the first 28-day cycle, the therapy is transitioned to all outpatient therapy
- Frequent discussions to review if the dose needs to be adjusted based on how the patient is metabolizing the medicine and coordinating around other medicines the patient may be taking
- Patients may be placed on antivirals, antibiotics, and antifungals to help prevent infection
- The second cycle of treatment
- Bone marrow biopsy at the start to review how well the first cycle worked. If not seeing leukemia in the bone marrow, will delay starting cycle two to give the patient’s bone marrow some time to recover
- If the patient still has leukemia cells in the bone marrow after the first treatment cycle, dose adjustments may need to be done because treatment can cause myeloid suppression or decreased blood counts
- Monitor blood counts (in particular platelets and neutrophils). If low, add a growth factor injection to help support blood count recovery
- Shortening the treatment cycles
- If patients’ AML cells are responding to treatment, each cycle after the first may not always be 28 days. Many healthcare providers will decrease the number of days a patient takes the medicine down to 21 days instead of 28. Some providers may decrease the number of days of a patient’s cycle to as little as 10 days. The reason is that 28 days can be too strong for ongoing treatment from the myeloid suppression. One study showed that there was no difference in median overall survival for AML patients who took venetoclax in 21-day cycles vs. the FDA label of 28-day cycles
Venetoclax Side Effects & Side Effect Solutions
Common side effects of venetoclax and solutions to reduce those side effects:
- Low blood cell count (white blood cell, platelet, and/or red blood cell)
- Blood cell growth stimulant injection
- Infections
- Antiviral, antibiotic, antifungal
- Monitor immunoglobulin (IGG) levels. If low, the patient may receive an IV of immunoglobulin (IVIG)
- Diarrhea
- Pepto Bismol
- Imodium
- Fiber
- Nausea
- IV fluids
- Anti-nausea medication
- Cough
- Cough suppressant medicine
- Muscle and joint pain
- Low-dose prednisone (anti-inflammatory)
- Tiredness
- Hydration, nutrient-dense food, rest
- Fluid buildup in the body (swelling of arms, legs, hands, and/or feet)
- Diuretics
- Limit sodium in diet
Rare but serious side effect of venetoclax:
- Tumor lysis syndrome (TLS) is a rare side effect of venetoclax. It is caused by the fast breakdown of cancer cells. Although serious, medical staff can help to reduce the side effect through IV fluids. If left unresolved, TLS may cause kidney failure, the need for dialysis treatment, or death. Tell your doctor right away if you experience symptoms associated with TLS including: fever, chills, vomiting, confusion, shortness of breath, seizures, dark or cloudy urine, or irregular heartbeat.
Notify your AML specialist about any side effects you may be experiencing. HealthTree's Side Effect Solutions tool is also available for patients to find and contribute solutions to common AML-related side effects.
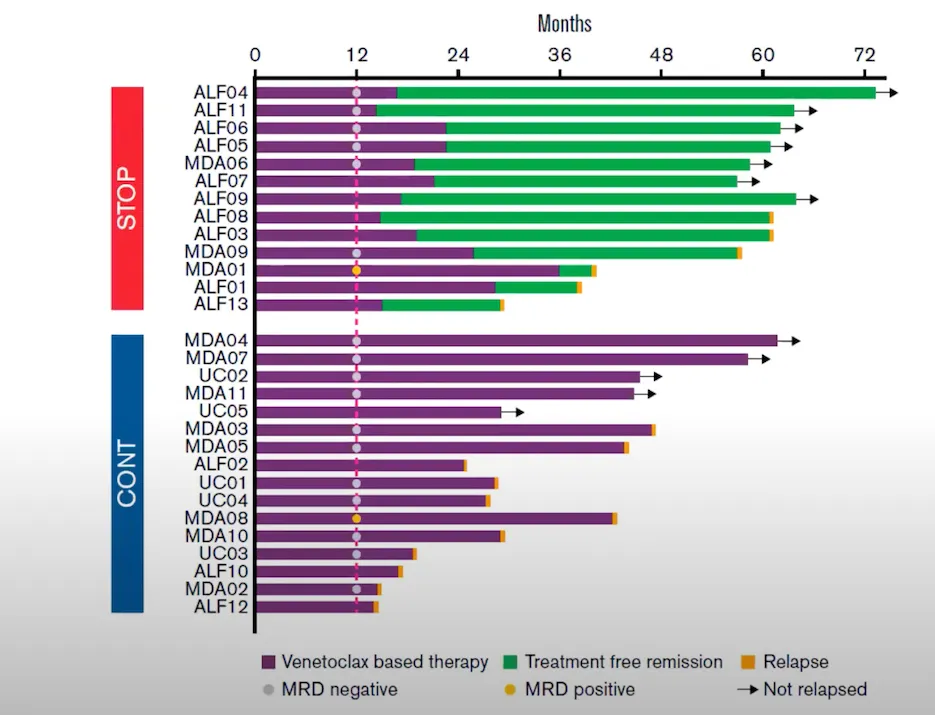
Fixed or continual-duration venetoclax treatment?
AML specialists are currently administering venetoclax with azacitidine as a continual duration therapy unless a patient is planning and able to receive a stem cell transplant. Continual-duration therapy means the AML patient is treated long-term so long as treatment is working (this is your decision, counsel with your AML specialist and discuss all questions that you have).
What if I don’t go towards transplant and do want to stop venetoclax + azacitidine?
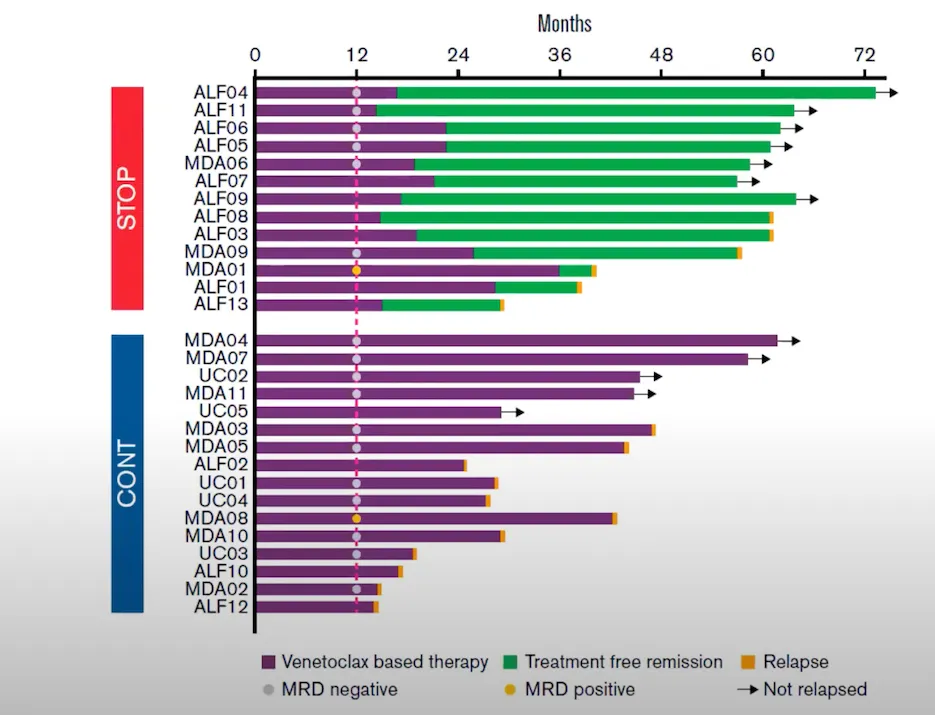
The VIALE study results showed that AML patients who stopped the treatment combination after 12 months, some patients relapsed soon after, whereas others continued to live in complete remission for years afterward.
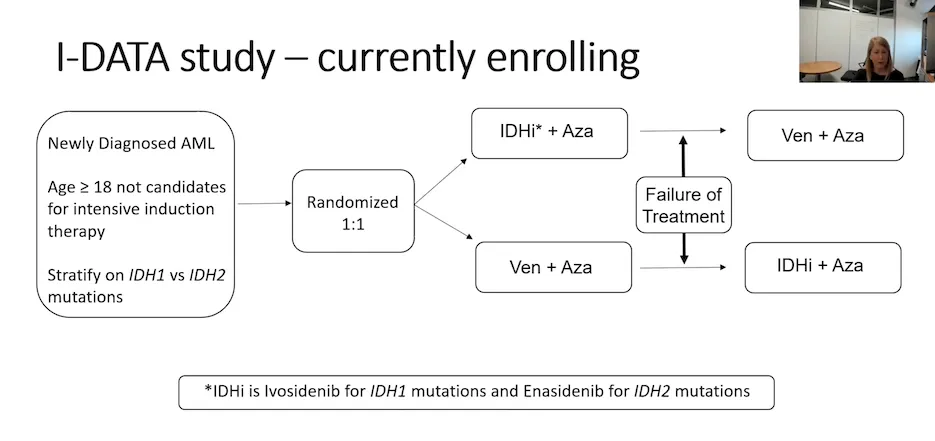
Venetoclax + Azacitidine for AML patients with an IDH mutation
The VIALE study showed promising results for AML patients with an IDH mutation (IDH1/2) as 75.4% of these patients achieved a complete remission (CR)/CRi being treated with venetoclax and azacitidine as well as favored longer overall survival.
Dr. Mims thought this was interesting that the venetoclax + azacitidine treatment combination worked better for these IDH mutation AML patients compared to another study that treated IDH mutation AML patients with the IDH1 inhibitor ivosidenib in combination with azacitidine achieving a 39% CR/CRi and median survival of 24 months.
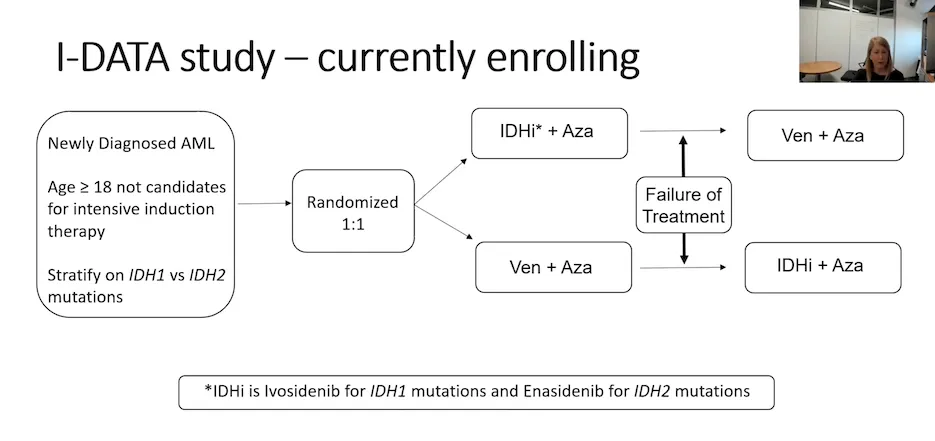
Dr. Mims and her colleague Dr. Eisfeld are conducting the I-DATA study to review which of these treatment regimens is better for AML patients with the IDH mutation. The study involves newly diagnosed AML patients with an IDH 1/2 mutation who are over the age of 18 and are not candidates for intensive induction therapy (7+3). The study is reviewing treating these patients with an IDH inhibitor + azacitidine or venetoclax + azacitidine, and if one of the therapies is not working, switching the patient to the other treatment combination.
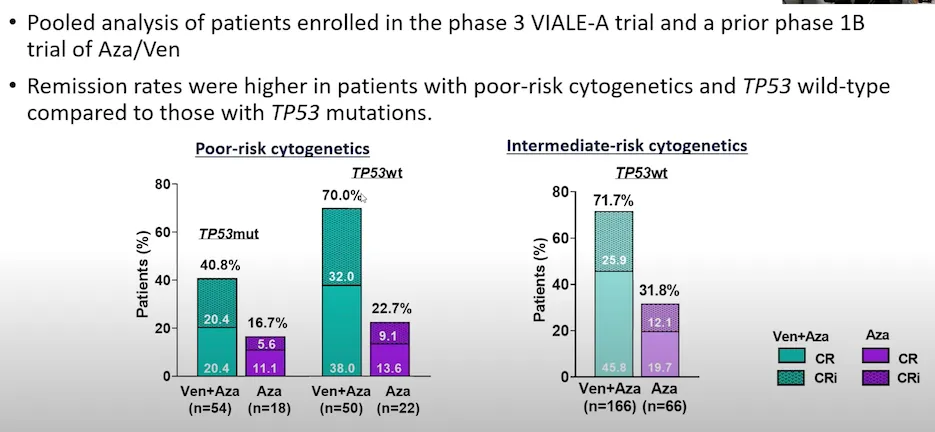
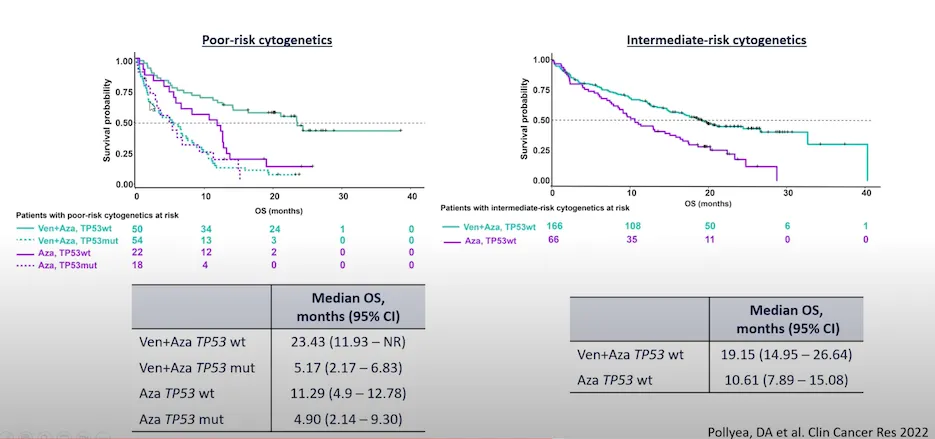
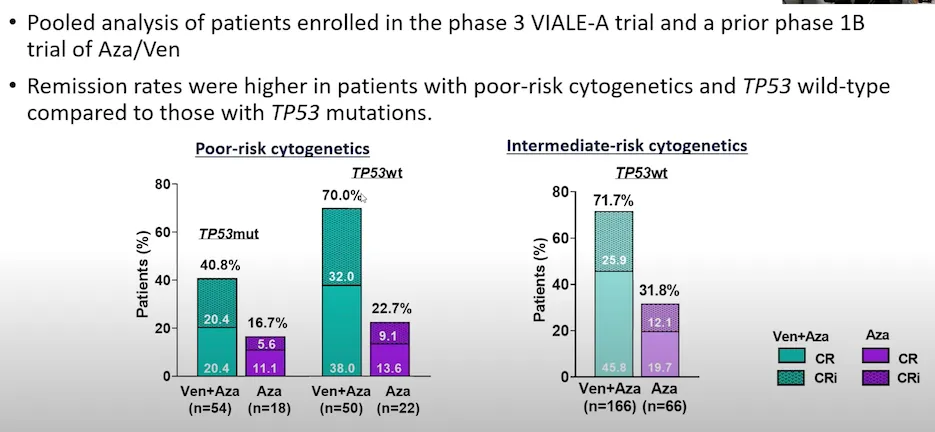
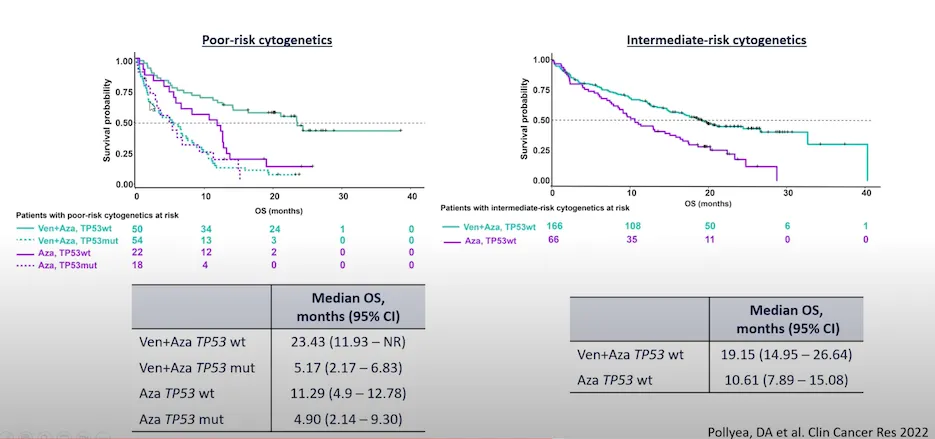
Venetoclax and Azacitidine for AML patients with TP53 mutations
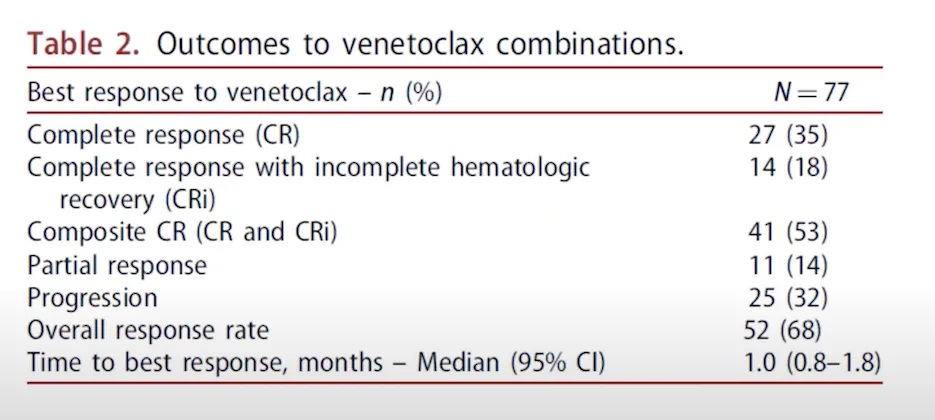
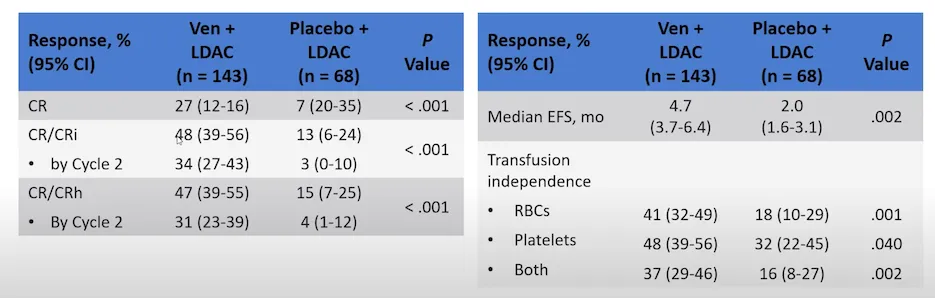
Clinical Trial Results: Venetoclax + Low-dose Cytarabine for Previously-untreated AML
- Venetoclax + low-dose cytarabine: Median overall survival 8.4 months
- Low-dose cytarabine by itself: Median overall survival 4.1 months
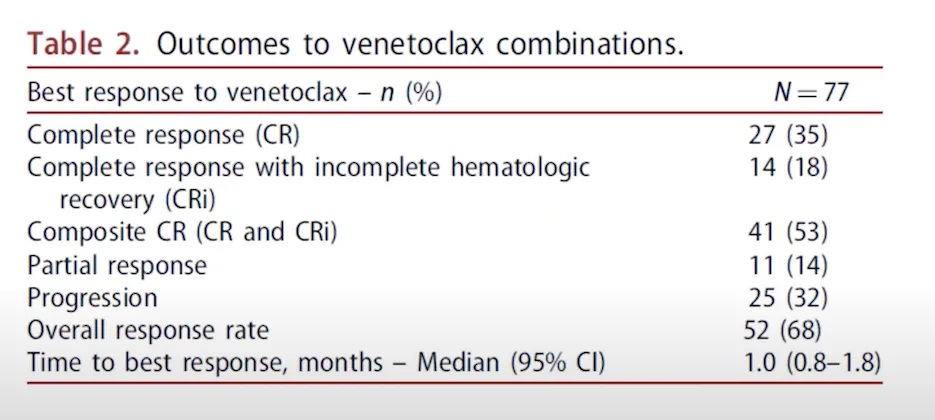
Results for using venetoclax to treat relapsed/refractory AML
What is the right treatment decision for me?
We understand that an AML diagnosis can be overwhelming and there are decisions that need to be made in a timely manner regarding the direction of your treatment path. To determine the best treatment that aligns with your priorities and your type of AML (genetic mutation), inform your doctor what you are trying to achieve. Dr. Mims stated some of the things she asks patients in order to identify the best treatment path for them include:
- What are your top goals for treatment? These could include areas like being interested in moving towards a cure, trying to get a stem cell transplant, spending more quality time with family, being closer to home
- Identifying a support system and caregiver(s): At certain points in their treatment journey, AML patients may visit their medical center multiple times a week and often need support. Identifying a support system such as a family member or friend who can help is beneficial. If a patient does not have a family member or friend available for this role, coordinate with your treatment center’s social worker who can help connect you to caregiver resources
- Impact of working
- Decreasing the risk of infection around loved ones and social events
- Travel, hobbies
Dr. Mims stated that the goals set in these areas may change from when a patient starts treatment towards hopefully achieving a remission. Create a short-term and long-term goal plan with your AML specialist as treatment may get less intensive over time.
Areas Currently Being Studied
- HMA pills instead of HMA infusions so AML patients would no longer need to come to the clinic for seven days in a row and could take venetoclax + the HMA pill at home. This is in clinical trials to get FDA-approved
- Triplet therapy of venetoclax, HMA decitabine, and an IDH inhibitor or FLIP3 inhibitor (depending on the AML patient’s genetic profile)
- After the first 28-day cycle of venetoclax treatment, if the patient has responded to treatment, doctors are reviewing stopping treatment for a period of time before additional cycles “treatment holiday”. Doctors are also reviewing the benefits of stopping venetoclax treatment for AML patients indefinitely after the first cycle
- Combining venetoclax with 7+3 (intensive induction chemotherapy)
- Using venetoclax as a maintenance therapy after transplant
Dr. Mims reiterated that it is important to have a discussion about the patient’s treatment goals with the patient, their support system, and their care team before starting any kind of therapy so that everyone is on the same page. Although the addition of venetoclax with HMA therapy has improved treatment outcomes for AML patients, she understands there is still work to do to continue raising the bar and get to a place of more curative therapies for AML patients.
Want to Learn More About Important AML Topics?
Sign up for HealthTree's Biweekly AML Newsletter
Dr. Alice S. Mims, acute leukemia section head and associate professor at Ohio State University Comprehensive Cancer Center shared with us information about FDA-approved venetoclax for AML treatment.
Watch the Full Event Here:
Event Summary
Dr. Mims covered several helpful topics related to the use of venetoclax in AML treatment including the study results of AML patients treated with venetoclax + hypomethylating agent (HMA) azacitidine, how the medicines work, the dosing ramp-up schedule, key things patients can expect starting treatment, solutions to certain venetoclax side effects, AML genetic mutation specific reactions to treatment, and exciting upcoming areas of study.
How the landscape of AML treatment has changed
Dr. Mims stated that before 2017, AML doctors would mainly use intensive induction therapy of 7+3 or high-dose cytarabine-based regimens. For AML patients who weren’t candidates of 7+3, they may be able to use different types of treatments like hypomethylating (HMA) agents, low-dose cytarabine, and for some AML patients, they would talk about supportive care/hospice. Below is a brief description of the FDA-approval history for AML therapy.
- 1970’s
- 7+3 induction (cytarabine/daunorubicin)
- Bone marrow transplant
- 2000 Gemtuzumab CD33 antibody
- 2002 Idarubicin an anthracycline can be used instead of daunorubicin
- 2010 Gemtuzumab withdrawn for safety concerns
- 2017
- Gemtuzumab back with adjustments made
- CPX-351, a liposomal version of cytarabine/daunorubicin
- Enasidenib an IDH inhibitor for IDH2 mutations
- Midostaurin a FLIP3 inhibitor given in combination with 7+3
- 2018
- Ivosidinib an IDH inhibitor for IDH1 mutations
- Gilteritinib, a second-generation FLIP3 inhibitor that’s approved in the relapsed/refractory setting
- Venetoclax approved for first-line therapy
- Glasdegib, a hedgehog inhibitor approved in combination with cytarabine
- 2020
- Azacitidine a hypomethylating agent (HMA) used for maintenance therapy
See here for more about these AML medicines.
One thing Dr. Mims noted was that non-intensive treatments such as HMAs don’t mean lower intensity treatment than intensive-induction chemotherapy 7+3. The HMA treatments do have side effects. She stated that hopefully as research continues, patient quality of life outcomes can keep improving.
Dr. Mims is happy about the progress made in the treatment setting for AML patients, however, she wants to continue to move the bar forward. Doctors should be thoughtful of newly diagnosed AML patients when talking about the different treatment options that may be available and what that looks like based on patients’ genetics, not just what used to be the go-to treatment before the 2017 AML medicine advancements.
How Venetoclax with Hypomethylating Agents (HMAs) or Low-dose Cytarabine Work
Venetoclax (venclexta) is a targeted therapy taken via tablets by mouth. It works by targeting cancerous AML cells (it can also bind to healthy B-cells) by blocking the BCL-2 protein, which regulates cell survival and death. Overproduction of BCL-2 is common in cancer cells, and blocking it with venetoclax causes the cancer cells to die.
Newly diagnosed AML patients who are 75 years or older, or patients who have other medical conditions that prevent the use of intensive chemotherapy (7+3) are approved to take venetoclax. Venetoclax is paired with either azacitidine (HMA), decitabine (HMA), or low-dose cytarabine.
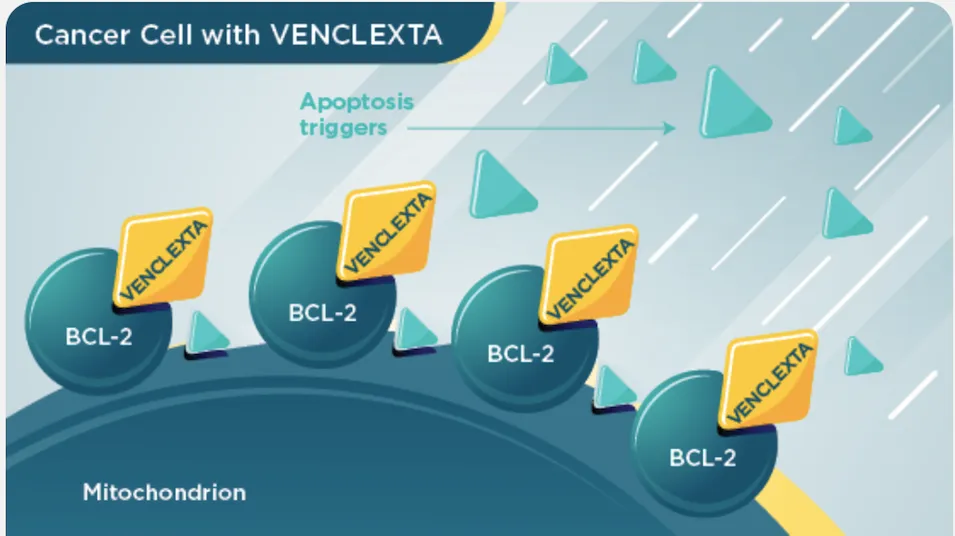
(Image Source: VENCLEXTA)
Hypomethylating Agents (HMAs)
Azacitidine and decitabine are hypomethylating agents (HMA). They work to kill cancerous AML cells by re-activating parts of the cancer cell’s instructions (DNA) that tell the cell to die. These DNA parts in the cancer cell were previously silenced when they shouldn’t have been.
Cytarabine
Cytarabine is a molecule that inserts itself into a cancer cell’s (and some healthy cells’) DNA (the cell’s instructions) messing with the cell to stop DNA from replicating itself, thus leading to cell death.
Clinical Trial Results: Venetoclax + Azacitidine (HMA) for Previously-untreated AML
The VIALE study helped get venetoclax for AML treatment FDA-approved. The details of the study along with its results are shown in the images below.
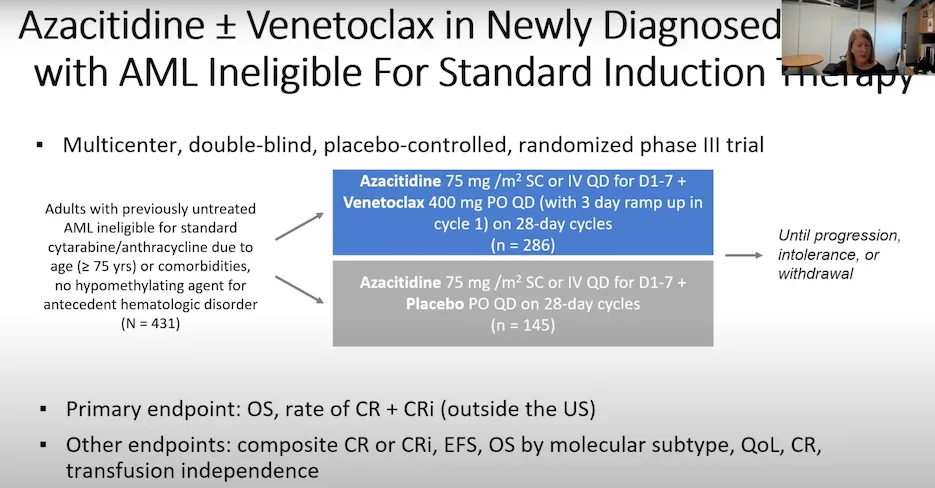
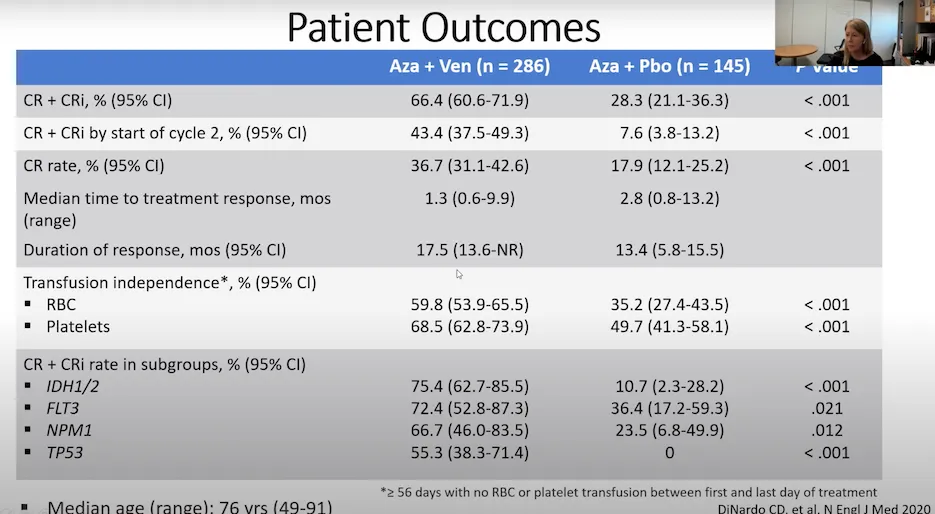
The treatment combination of venetoclax with azacitidine proved to be significantly better than using azacitidine by itself for AML patients.
These areas included:
- Complete remission rate (CR)
- AML cells are less than five percent blast in the bone marrow and the patient’s platelet and neutrophil counts have returned to normal
- Complete remission with incomplete count recovery (CRi)
- AML cells are less than five percent blast in the bone marrow. Either the platelet or neutrophil counts have recovered to normal range, but not both
- Median time to treatment response
- The amount of time it took for the cancer cells to start decreasing since the beginning of treatment
- Duration of response
- The length of time the cancer cells continued to respond to treatment and did not increase
- Transfusion independence
- Patients no longer needed to receive infusions of certain types of blood cells (red blood cells or platelets). Dr. Mims stated AML patients consider this an important quality-of-life factor
The median overall survival results from the study were:
- Venetoclax + azacitidine: 14.7 months
- Azacitidine by itself: 9.6 months
Dosing Schedule of Venetoclax + HMA ramp-up
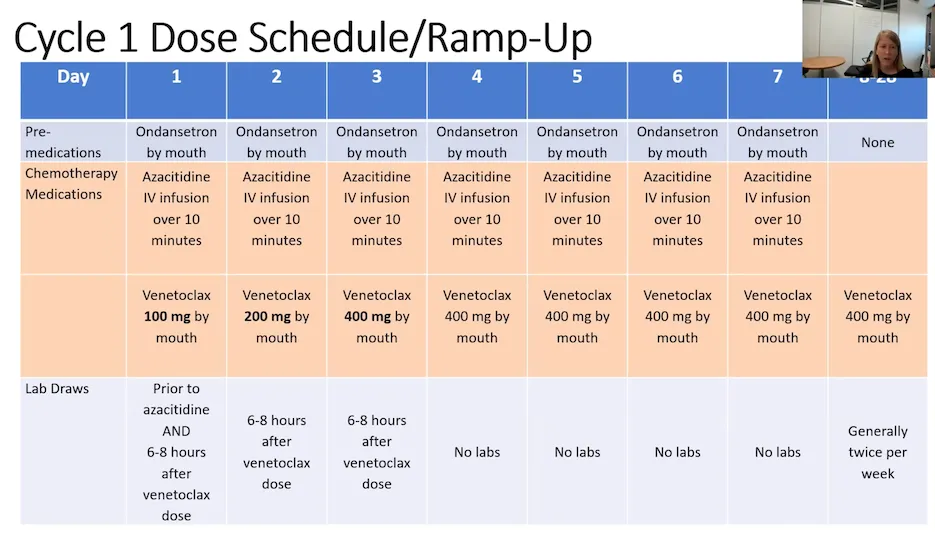
What AML patients can expect ramping up on venetoclax
- Frequent labs during the ramp-up period to check blood counts, risk of infection, and risk of tumor lysis syndrome (rare but treatable)
- The first cycle of treatment can be given inpatient or outpatient. The choice of which one is dependent on individual patient factors and the treatment institution. After the first 28-day cycle, the therapy is transitioned to all outpatient therapy
- Frequent discussions to review if the dose needs to be adjusted based on how the patient is metabolizing the medicine and coordinating around other medicines the patient may be taking
- Patients may be placed on antivirals, antibiotics, and antifungals to help prevent infection
- The second cycle of treatment
- Bone marrow biopsy at the start to review how well the first cycle worked. If not seeing leukemia in the bone marrow, will delay starting cycle two to give the patient’s bone marrow some time to recover
- If the patient still has leukemia cells in the bone marrow after the first treatment cycle, dose adjustments may need to be done because treatment can cause myeloid suppression or decreased blood counts
- Monitor blood counts (in particular platelets and neutrophils). If low, add a growth factor injection to help support blood count recovery
- Shortening the treatment cycles
- If patients’ AML cells are responding to treatment, each cycle after the first may not always be 28 days. Many healthcare providers will decrease the number of days a patient takes the medicine down to 21 days instead of 28. Some providers may decrease the number of days of a patient’s cycle to as little as 10 days. The reason is that 28 days can be too strong for ongoing treatment from the myeloid suppression. One study showed that there was no difference in median overall survival for AML patients who took venetoclax in 21-day cycles vs. the FDA label of 28-day cycles
Venetoclax Side Effects & Side Effect Solutions
Common side effects of venetoclax and solutions to reduce those side effects:
- Low blood cell count (white blood cell, platelet, and/or red blood cell)
- Blood cell growth stimulant injection
- Infections
- Antiviral, antibiotic, antifungal
- Monitor immunoglobulin (IGG) levels. If low, the patient may receive an IV of immunoglobulin (IVIG)
- Diarrhea
- Pepto Bismol
- Imodium
- Fiber
- Nausea
- IV fluids
- Anti-nausea medication
- Cough
- Cough suppressant medicine
- Muscle and joint pain
- Low-dose prednisone (anti-inflammatory)
- Tiredness
- Hydration, nutrient-dense food, rest
- Fluid buildup in the body (swelling of arms, legs, hands, and/or feet)
- Diuretics
- Limit sodium in diet
Rare but serious side effect of venetoclax:
- Tumor lysis syndrome (TLS) is a rare side effect of venetoclax. It is caused by the fast breakdown of cancer cells. Although serious, medical staff can help to reduce the side effect through IV fluids. If left unresolved, TLS may cause kidney failure, the need for dialysis treatment, or death. Tell your doctor right away if you experience symptoms associated with TLS including: fever, chills, vomiting, confusion, shortness of breath, seizures, dark or cloudy urine, or irregular heartbeat.
Notify your AML specialist about any side effects you may be experiencing. HealthTree's Side Effect Solutions tool is also available for patients to find and contribute solutions to common AML-related side effects.
Fixed or continual-duration venetoclax treatment?
AML specialists are currently administering venetoclax with azacitidine as a continual duration therapy unless a patient is planning and able to receive a stem cell transplant. Continual-duration therapy means the AML patient is treated long-term so long as treatment is working (this is your decision, counsel with your AML specialist and discuss all questions that you have).
What if I don’t go towards transplant and do want to stop venetoclax + azacitidine?
The VIALE study results showed that AML patients who stopped the treatment combination after 12 months, some patients relapsed soon after, whereas others continued to live in complete remission for years afterward.
Venetoclax + Azacitidine for AML patients with an IDH mutation
The VIALE study showed promising results for AML patients with an IDH mutation (IDH1/2) as 75.4% of these patients achieved a complete remission (CR)/CRi being treated with venetoclax and azacitidine as well as favored longer overall survival.
Dr. Mims thought this was interesting that the venetoclax + azacitidine treatment combination worked better for these IDH mutation AML patients compared to another study that treated IDH mutation AML patients with the IDH1 inhibitor ivosidenib in combination with azacitidine achieving a 39% CR/CRi and median survival of 24 months.
Dr. Mims and her colleague Dr. Eisfeld are conducting the I-DATA study to review which of these treatment regimens is better for AML patients with the IDH mutation. The study involves newly diagnosed AML patients with an IDH 1/2 mutation who are over the age of 18 and are not candidates for intensive induction therapy (7+3). The study is reviewing treating these patients with an IDH inhibitor + azacitidine or venetoclax + azacitidine, and if one of the therapies is not working, switching the patient to the other treatment combination.
Venetoclax and Azacitidine for AML patients with TP53 mutations
Clinical Trial Results: Venetoclax + Low-dose Cytarabine for Previously-untreated AML
- Venetoclax + low-dose cytarabine: Median overall survival 8.4 months
- Low-dose cytarabine by itself: Median overall survival 4.1 months
Results for using venetoclax to treat relapsed/refractory AML
What is the right treatment decision for me?
We understand that an AML diagnosis can be overwhelming and there are decisions that need to be made in a timely manner regarding the direction of your treatment path. To determine the best treatment that aligns with your priorities and your type of AML (genetic mutation), inform your doctor what you are trying to achieve. Dr. Mims stated some of the things she asks patients in order to identify the best treatment path for them include:
- What are your top goals for treatment? These could include areas like being interested in moving towards a cure, trying to get a stem cell transplant, spending more quality time with family, being closer to home
- Identifying a support system and caregiver(s): At certain points in their treatment journey, AML patients may visit their medical center multiple times a week and often need support. Identifying a support system such as a family member or friend who can help is beneficial. If a patient does not have a family member or friend available for this role, coordinate with your treatment center’s social worker who can help connect you to caregiver resources
- Impact of working
- Decreasing the risk of infection around loved ones and social events
- Travel, hobbies
Dr. Mims stated that the goals set in these areas may change from when a patient starts treatment towards hopefully achieving a remission. Create a short-term and long-term goal plan with your AML specialist as treatment may get less intensive over time.
Areas Currently Being Studied
- HMA pills instead of HMA infusions so AML patients would no longer need to come to the clinic for seven days in a row and could take venetoclax + the HMA pill at home. This is in clinical trials to get FDA-approved
- Triplet therapy of venetoclax, HMA decitabine, and an IDH inhibitor or FLIP3 inhibitor (depending on the AML patient’s genetic profile)
- After the first 28-day cycle of venetoclax treatment, if the patient has responded to treatment, doctors are reviewing stopping treatment for a period of time before additional cycles “treatment holiday”. Doctors are also reviewing the benefits of stopping venetoclax treatment for AML patients indefinitely after the first cycle
- Combining venetoclax with 7+3 (intensive induction chemotherapy)
- Using venetoclax as a maintenance therapy after transplant
Dr. Mims reiterated that it is important to have a discussion about the patient’s treatment goals with the patient, their support system, and their care team before starting any kind of therapy so that everyone is on the same page. Although the addition of venetoclax with HMA therapy has improved treatment outcomes for AML patients, she understands there is still work to do to continue raising the bar and get to a place of more curative therapies for AML patients.

about the author
Megan Heaps
Megan joined HealthTree in 2022. She enjoys helping patients and their care partners understand the various aspects of the cancer. This understanding enables them to better advocate for themselves and improve their treatment outcomes.
More on Navigating Your Health
Trending Articles

Get the Latest Acute Myeloid Leukemia Updates, Delivered to You.
By subscribing to the HealthTree newsletter, you'll receive the latest research, treatment updates, and expert insights to help you navigate your health.
Together we care.
Together we cure.











