Palliative and Hospice Care for AML Patients
The content provided in this page is to help address the often difficult topics of palliative care and hospice. Content contributions were made by Steve Hodges, a long-time hospice volunteer, hospice patient family advisor, social worker, and AML patient.
“Yes, it’s hard stuff, but it’s a courageous investment that can make your final stretch so much better.” -Steve Hodges
What Type of Care is Best For You?
Patients planning the last stages of their life on earth may only think about funeral arrangements and the location of their final resting place. These individuals may not think about and plan for the type of care they want toward the end of life. The following are ideas and recommendations from Steve’s hospice volunteering and personal journey that patients and their caregivers can include to help better their quality of life during that time.
The Importance of Planning Ahead
"Considering the undeniable fact that someday every one of us will die, it’s arguable that everyone should have a plan. Otherwise, all the important decisions that go with our last months on earth are likely to be made by others. That’s burdensome to whoever ends up with these decisions to make. We are giving them a huge gift when we plan it ourselves. Otherwise, there are anxious moments and extended worry when there’s a dilemma of someone or multiple someones who have to decipher what your wishes are without your direct input. Getting together ahead of time with a lawyer or social worker who specializes in documenting your Advance Directives is a great start."
"Hospice social workers can help. The next steps should include documenting your detailed care wishes with respect to when you’d like to get a palliative care doc, when you want hospice, and specifics about the care to be provided. Good guidelines for documenting your care preferences during the last stretch can include things like: The Five Wishes and The Four Things That Matter Most. The latter is also a call to action to have an important conversation with your loved ones before decline sets in. For my part, my top wish for when I get to my last stretch is to be treated with love and kindness, with valediction and stories, not with sadness. What are your wishes? Express them! Write them down for your loved ones. Inevitably these will be so very valuable to those who matter and for you." - Steve Hodges
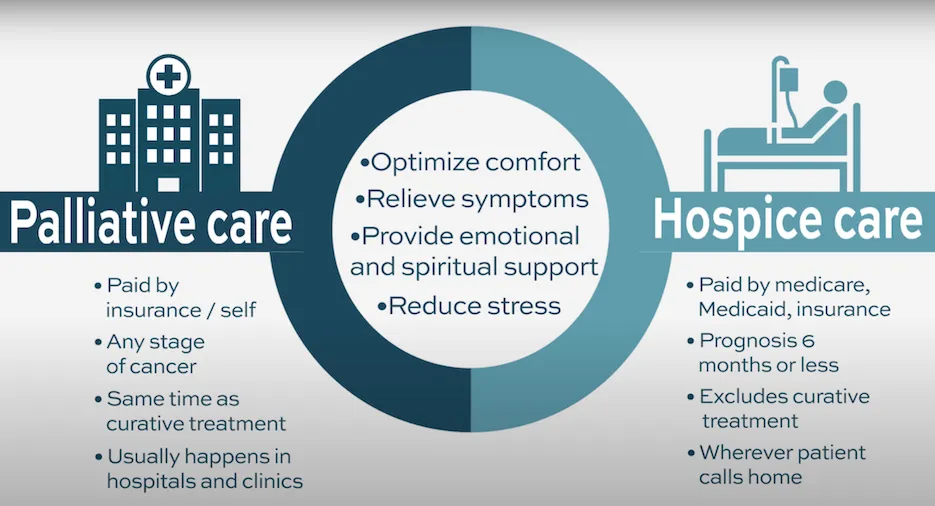
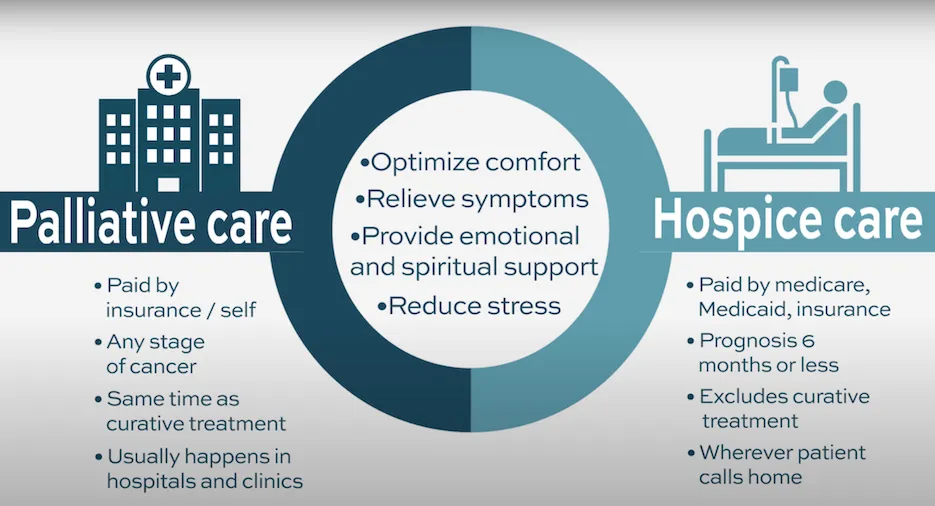
What is the Difference Between Palliative Care and Hospice?
Palliative care sometimes referred to as supportive care, is a comprehensive approach to help better a patient’s quality of life while they live alongside the disease. Patients can request a palliative care professional be added to their care team if they are experiencing pain on a regular basis. This can be during the patient receiving treatment or if they are enrolled in hospice.
Hospice care is a specialized subset of palliative care for patients in their last 6 months of life. It provides all the benefits of palliative care but with a higher level of care focused on symptom relief and comfort for those who are no longer pursuing a cure or long-term remission for their disease.
What is Included in Palliative Care and Hospice?
Many patients experience pain related to the disease throughout its course whether that’s physical, mental/emotional, relationship, financial, or spiritual pain. To help alleviate suffering, trained care team members can help you and your loved ones have a better experience by reducing pain using supportive measures.
Palliative care and hospice may include:
- Doctors, nurses, certified nursing assistants, social workers, home health aides
- Pain-alleviating medicines
- Medical supplies and equipment
- Assistance with daily tasks
- Other therapies like pet therapy, music, reading, and companionship
- A break (respite care) for the patient’s normal caregivers provided by volunteers, homemakers (as needed), and health aides
- Financial planners and legal advisors to help manage and organize matters
- Resources to help with spiritual health such as coordinating with the patient’s preferred religious leader/Chaplain to help talk through spiritual concerns or administer other desired religious services
- Measures to alleviate emotional suffering such as:
- Creating a more joyful and comforting environment around the patient with items like photos of their favorite people and places, important keepsakes, and favorite music
- Reviewing opportunities to include meaningful social interaction for the patient
- Providing counseling if desired to help the patient with personal struggles and/or help to resolve family/friend relationship disputes
- Counseling services for the patient’s family members during and for 13 months after passing, grief counseling
When Do I Request a Palliative Care Consultation?
Patients can request a palliative care consultation if they are experiencing pain on a regular basis.
“Palliative care providers are excellent at fine-tuning your pain meds (from personal experience). Sometimes there are simple fixes to the medication side effects and wonderful alternatives to medications that are causing too much trouble. With AML, we are all on lots of medications. We have meds for cancer from our providers, but the experts on pain meds are the palliative care providers who can be added to your team. They are expert LISTENERS. They take a holistic approach that includes addressing the psychosocial elements of what can improve your quality of life.” -Steve
How Do I Prepare for my Consultation?
- Bring a list of symptoms you are experiencing. Write down what makes the symptoms better or worse and if they affect your ability to go about your daily activities
- Bring a list of medicines and supplements you use and the frequency you take them
- Consider bringing a family member or friend with you to the appointment
- Bring any advance directives and living wills you've completed
What is Included in the Consultation?
Your palliative care team will talk with you about your symptoms, current treatments, and how the cancer is affecting you and your family. You'll make a plan to ease suffering and improve your quality of life. The plan will be carried out in coordination with your primary care team in a way that works well with any other treatment you're receiving.
Visit our palliative care and hospice HealthTree University course.
Is Hospice for Me?
“A hospice consult and afterward writing your wishes down for loved ones can be one of the most freeing experiences you can have with a cancer diagnosis. It also can turn the somber and potentially confusing aspects for those who take care of things at the end, into a more peaceful act of love, of following your stated wishes rather than being wracked with hard decisions. They will realize just how much you cared about them to remove that stress.” - Steve
It is recommended to have a hospice consult in advance of your passing. Patients and their caregivers may consider discussing hospice when:
- Presented with the need for treatment after relapse
- Reviewing how much time the treatment will potentially extend the length of life
- The patient doesn’t have a relapse but is experiencing severe health decline signs/symptoms that the medical team is unable to reverse
- Considering what are the side effects of treatment, how long they last, and does the patient’s quality of life improve after treatment
- Based on the patient’s current health status, what their medical team believes their life expectancy to be (patients will need to be persistent to get this information as medical providers tend to focus mainly on the next line of therapy)
Your physician and the hospice medical director will discuss whether you yet meet the criteria or when you might meet them. The basic criterion being whether the normal course of your disease would lead to your death in future months. Each patient’s disease state varies.
After getting the answers, think hard with whoever’s closest to you about whether you want the treatment or not. If yes, press onward! Talk with your cancer specialist to discuss it. If not, know that your decision to move toward the last stages of life on earth with hospice should be respected regardless of others’ beliefs.
“At the end, I want a sunset, not a nightmare.” -Steve

Empowerment Through Respect: Honoring Your Decisions in Healthcare
The decision to continue treatment options to review ridding the cancer from your body or your decision to stop treatment and let the disease run its course until your passing is your decision.
Your decision for either option is valuable and should always be respected. If you do not feel like stopping curative treatment and you sense disappointment on the part of the medical staff, please know this is often not intentional. Medical team members are frequently trained to keep looking for the next effective line of treatment for patients to help eradicate the disease and prolong the length and quality of a patient's life.
If you choose to stop treatment to let the disease run its course till your passing, please know that your decision should be respected and does have value, even if some medical team members have been instilled to keep looking for the next line of treatment.
Can I Reverse my Hospice Care Decision?
If you decide to enroll in hospice, please know that if at any time you would like to continue treatment to try to reduce the disease and extend your length of life, pulling out of hospice is an option. Another instance that may reverse a patient staying in hospice is if they miraculously improve.
What are Myths About Hospice Care?
- I can no longer see my oncologist when I enroll in hospice
- I have to give up my preferred doctor
- Hospice is giving up, you go there to die
- Hospice gives the patient morphine to die
- It is the doctor’s responsibility to bring up hospice
- There is no turning back after you start hospice
- IV fluids, blood transfusions, and other more invasive procedures are not allowed on hospice
- Hospice enrollment means rapid progression to death
- Hospice is only provided at a Hospice facility (over 95% is provided wherever the patient lives)
Patient Behaviors Loved Ones can Expect Before the Patient Passes Away
Turning Inward
Patients nearing the end of their lives on earth tend to turn inward, which means they may lose interest in the world around them.
“When we are entering our final stretch our thoughts begin to turn inward. We are less aware of or interested in the world around us. We may lose interest in a lot of things that we used to be aware of, including appetite. It’s a slow change in awareness and interest level. At the very end, we lose various senses and are nearly unaware of the outside world except those who are with us. Hearing is the last sense to go, something that visitors need to know and leverage. Long before actively dying, if you and your caregiver consider whether there’s a downward trend in your awareness and engagement over time, of your interest in the world and what’s happening in it, you may discern this “drawing inward.” Staff can help rule out simple depression as the cause, leaving the profound process of drawing near to the end.” -Steve
Possibility of Voluntarily Stop Eating or Drinking
For someone who wishes to have increased control over the time and manner of their passing, a patient may choose to stop eating and drinking (only a little water for moisture) referred to as VSED (Voluntarily Stop Eating or Drinking). VSED is something a patient decides for themselves. It may help with a gentler passing causing the body to shut down and float away mentally. If a patient chooses VSED, caregivers/staff will need to be notified to not bring meals.
What is it Like to Be With Someone at the End of Life?
“When the symptoms are well managed, particularly pain and anxiety, the experience is the only thing I’ve ever experienced that compares to being present at the birth of my children. There is an indescribable aspect that is, like birth, sacred. As for a newborn, soothing is appropriate for the dying. Touch, gentle speech, and gentle music are good. These are priceless well before the actively dying phase.” -Steve
How to Best Support Your Loved One During Passing?
“Memories are good medicine as we start toward the sunset, and can be prompted by photos, discussion, music, taste, smell, foods and people that bring memories and a sense of accomplishment. This is a good time (but not the only time) to talk about The Four Things That Matter Most with loved ones. Memories are where our thoughts go as we turn inward. Make it a beautiful sunset if you can.” -Steve
If you’d like to work with Steve to get more information about palliative care and/or hospice, contact him through our Coach website.
The content provided in this page is to help address the often difficult topics of palliative care and hospice. Content contributions were made by Steve Hodges, a long-time hospice volunteer, hospice patient family advisor, social worker, and AML patient.
“Yes, it’s hard stuff, but it’s a courageous investment that can make your final stretch so much better.” -Steve Hodges
What Type of Care is Best For You?
Patients planning the last stages of their life on earth may only think about funeral arrangements and the location of their final resting place. These individuals may not think about and plan for the type of care they want toward the end of life. The following are ideas and recommendations from Steve’s hospice volunteering and personal journey that patients and their caregivers can include to help better their quality of life during that time.
The Importance of Planning Ahead
"Considering the undeniable fact that someday every one of us will die, it’s arguable that everyone should have a plan. Otherwise, all the important decisions that go with our last months on earth are likely to be made by others. That’s burdensome to whoever ends up with these decisions to make. We are giving them a huge gift when we plan it ourselves. Otherwise, there are anxious moments and extended worry when there’s a dilemma of someone or multiple someones who have to decipher what your wishes are without your direct input. Getting together ahead of time with a lawyer or social worker who specializes in documenting your Advance Directives is a great start."
"Hospice social workers can help. The next steps should include documenting your detailed care wishes with respect to when you’d like to get a palliative care doc, when you want hospice, and specifics about the care to be provided. Good guidelines for documenting your care preferences during the last stretch can include things like: The Five Wishes and The Four Things That Matter Most. The latter is also a call to action to have an important conversation with your loved ones before decline sets in. For my part, my top wish for when I get to my last stretch is to be treated with love and kindness, with valediction and stories, not with sadness. What are your wishes? Express them! Write them down for your loved ones. Inevitably these will be so very valuable to those who matter and for you." - Steve Hodges
What is the Difference Between Palliative Care and Hospice?
Palliative care sometimes referred to as supportive care, is a comprehensive approach to help better a patient’s quality of life while they live alongside the disease. Patients can request a palliative care professional be added to their care team if they are experiencing pain on a regular basis. This can be during the patient receiving treatment or if they are enrolled in hospice.
Hospice care is a specialized subset of palliative care for patients in their last 6 months of life. It provides all the benefits of palliative care but with a higher level of care focused on symptom relief and comfort for those who are no longer pursuing a cure or long-term remission for their disease.
What is Included in Palliative Care and Hospice?
Many patients experience pain related to the disease throughout its course whether that’s physical, mental/emotional, relationship, financial, or spiritual pain. To help alleviate suffering, trained care team members can help you and your loved ones have a better experience by reducing pain using supportive measures.
Palliative care and hospice may include:
- Doctors, nurses, certified nursing assistants, social workers, home health aides
- Pain-alleviating medicines
- Medical supplies and equipment
- Assistance with daily tasks
- Other therapies like pet therapy, music, reading, and companionship
- A break (respite care) for the patient’s normal caregivers provided by volunteers, homemakers (as needed), and health aides
- Financial planners and legal advisors to help manage and organize matters
- Resources to help with spiritual health such as coordinating with the patient’s preferred religious leader/Chaplain to help talk through spiritual concerns or administer other desired religious services
- Measures to alleviate emotional suffering such as:
- Creating a more joyful and comforting environment around the patient with items like photos of their favorite people and places, important keepsakes, and favorite music
- Reviewing opportunities to include meaningful social interaction for the patient
- Providing counseling if desired to help the patient with personal struggles and/or help to resolve family/friend relationship disputes
- Counseling services for the patient’s family members during and for 13 months after passing, grief counseling
When Do I Request a Palliative Care Consultation?
Patients can request a palliative care consultation if they are experiencing pain on a regular basis.
“Palliative care providers are excellent at fine-tuning your pain meds (from personal experience). Sometimes there are simple fixes to the medication side effects and wonderful alternatives to medications that are causing too much trouble. With AML, we are all on lots of medications. We have meds for cancer from our providers, but the experts on pain meds are the palliative care providers who can be added to your team. They are expert LISTENERS. They take a holistic approach that includes addressing the psychosocial elements of what can improve your quality of life.” -Steve
How Do I Prepare for my Consultation?
- Bring a list of symptoms you are experiencing. Write down what makes the symptoms better or worse and if they affect your ability to go about your daily activities
- Bring a list of medicines and supplements you use and the frequency you take them
- Consider bringing a family member or friend with you to the appointment
- Bring any advance directives and living wills you've completed
What is Included in the Consultation?
Your palliative care team will talk with you about your symptoms, current treatments, and how the cancer is affecting you and your family. You'll make a plan to ease suffering and improve your quality of life. The plan will be carried out in coordination with your primary care team in a way that works well with any other treatment you're receiving.
Visit our palliative care and hospice HealthTree University course.
Is Hospice for Me?
“A hospice consult and afterward writing your wishes down for loved ones can be one of the most freeing experiences you can have with a cancer diagnosis. It also can turn the somber and potentially confusing aspects for those who take care of things at the end, into a more peaceful act of love, of following your stated wishes rather than being wracked with hard decisions. They will realize just how much you cared about them to remove that stress.” - Steve
It is recommended to have a hospice consult in advance of your passing. Patients and their caregivers may consider discussing hospice when:
- Presented with the need for treatment after relapse
- Reviewing how much time the treatment will potentially extend the length of life
- The patient doesn’t have a relapse but is experiencing severe health decline signs/symptoms that the medical team is unable to reverse
- Considering what are the side effects of treatment, how long they last, and does the patient’s quality of life improve after treatment
- Based on the patient’s current health status, what their medical team believes their life expectancy to be (patients will need to be persistent to get this information as medical providers tend to focus mainly on the next line of therapy)
Your physician and the hospice medical director will discuss whether you yet meet the criteria or when you might meet them. The basic criterion being whether the normal course of your disease would lead to your death in future months. Each patient’s disease state varies.
After getting the answers, think hard with whoever’s closest to you about whether you want the treatment or not. If yes, press onward! Talk with your cancer specialist to discuss it. If not, know that your decision to move toward the last stages of life on earth with hospice should be respected regardless of others’ beliefs.
“At the end, I want a sunset, not a nightmare.” -Steve

Empowerment Through Respect: Honoring Your Decisions in Healthcare
The decision to continue treatment options to review ridding the cancer from your body or your decision to stop treatment and let the disease run its course until your passing is your decision.
Your decision for either option is valuable and should always be respected. If you do not feel like stopping curative treatment and you sense disappointment on the part of the medical staff, please know this is often not intentional. Medical team members are frequently trained to keep looking for the next effective line of treatment for patients to help eradicate the disease and prolong the length and quality of a patient's life.
If you choose to stop treatment to let the disease run its course till your passing, please know that your decision should be respected and does have value, even if some medical team members have been instilled to keep looking for the next line of treatment.
Can I Reverse my Hospice Care Decision?
If you decide to enroll in hospice, please know that if at any time you would like to continue treatment to try to reduce the disease and extend your length of life, pulling out of hospice is an option. Another instance that may reverse a patient staying in hospice is if they miraculously improve.
What are Myths About Hospice Care?
- I can no longer see my oncologist when I enroll in hospice
- I have to give up my preferred doctor
- Hospice is giving up, you go there to die
- Hospice gives the patient morphine to die
- It is the doctor’s responsibility to bring up hospice
- There is no turning back after you start hospice
- IV fluids, blood transfusions, and other more invasive procedures are not allowed on hospice
- Hospice enrollment means rapid progression to death
- Hospice is only provided at a Hospice facility (over 95% is provided wherever the patient lives)
Patient Behaviors Loved Ones can Expect Before the Patient Passes Away
Turning Inward
Patients nearing the end of their lives on earth tend to turn inward, which means they may lose interest in the world around them.
“When we are entering our final stretch our thoughts begin to turn inward. We are less aware of or interested in the world around us. We may lose interest in a lot of things that we used to be aware of, including appetite. It’s a slow change in awareness and interest level. At the very end, we lose various senses and are nearly unaware of the outside world except those who are with us. Hearing is the last sense to go, something that visitors need to know and leverage. Long before actively dying, if you and your caregiver consider whether there’s a downward trend in your awareness and engagement over time, of your interest in the world and what’s happening in it, you may discern this “drawing inward.” Staff can help rule out simple depression as the cause, leaving the profound process of drawing near to the end.” -Steve
Possibility of Voluntarily Stop Eating or Drinking
For someone who wishes to have increased control over the time and manner of their passing, a patient may choose to stop eating and drinking (only a little water for moisture) referred to as VSED (Voluntarily Stop Eating or Drinking). VSED is something a patient decides for themselves. It may help with a gentler passing causing the body to shut down and float away mentally. If a patient chooses VSED, caregivers/staff will need to be notified to not bring meals.
What is it Like to Be With Someone at the End of Life?
“When the symptoms are well managed, particularly pain and anxiety, the experience is the only thing I’ve ever experienced that compares to being present at the birth of my children. There is an indescribable aspect that is, like birth, sacred. As for a newborn, soothing is appropriate for the dying. Touch, gentle speech, and gentle music are good. These are priceless well before the actively dying phase.” -Steve
How to Best Support Your Loved One During Passing?
“Memories are good medicine as we start toward the sunset, and can be prompted by photos, discussion, music, taste, smell, foods and people that bring memories and a sense of accomplishment. This is a good time (but not the only time) to talk about The Four Things That Matter Most with loved ones. Memories are where our thoughts go as we turn inward. Make it a beautiful sunset if you can.” -Steve
If you’d like to work with Steve to get more information about palliative care and/or hospice, contact him through our Coach website.
Trending Articles
Get the Latest Acute Myeloid Leukemia Updates, Delivered to You.
By subscribing to the HealthTree newsletter, you'll receive the latest research, treatment updates, and expert insights to help you navigate your health.
Together we care.
Together we cure.