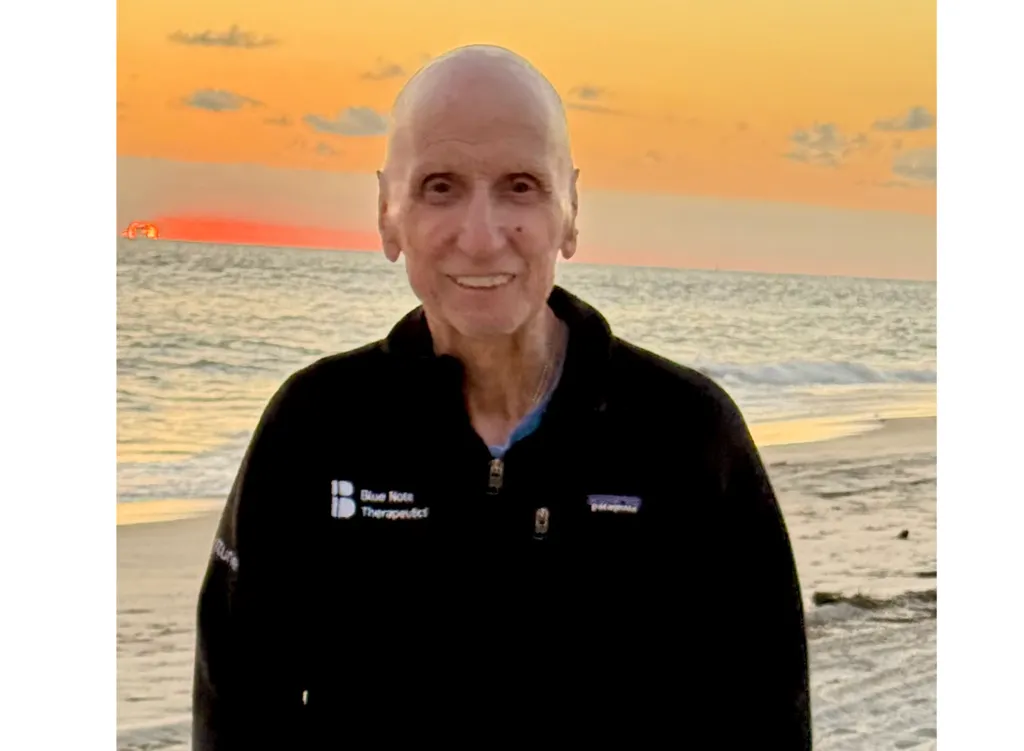
We’re Going to Take Your Blood Counts to Zero by Kenny Hall, AML and Stem Cell Transplant Survivor

There are places we visit during our lives that become part of us. We think of them fondly and run to them for comfort in times of trouble. Galveston Beach is such a place for me. As a young child I vacationed there with my family and the Galveston Jack Tarr Resort was the location of my high school senior trip. As a young adult, one of my first adult vacation sights was Galveston; on the beach during the day and in the Astrodome at night watching my Cardinals play the Astros.
I’ve realized that I most definitely use places for comfort. Regardless of where our place of comfort is, when we are there we are taken back to a place in time that we remember fondly and would love to return. When you are a few days from entering the hospital for a stem cell transplant and wondering about your odds of surviving, visiting a place of comfort is a way to relax. Natalie (my wife) and I went to Galveston on the weekend before my transplant. As the waves churned against the sandy shore on a breezy and mild late October day in 2012, I recalled the happy times with my family, my high school classmates and my adult vacations there.
Discussing the treatment plan following my MDS diagnosis in April 2012, my oncologist in Little Rock described how it’s necessary to put the disease into remission before a stem cell transplant can be done. Putting cancer into remission sounded like a great thing. But to accomplish it, they would put me in isolation, with no bathroom, and give me high dose chemotherapy. I thought, no thank you, let’s just keep the MDS in check with tolerable chemotherapy. But after barely two months of treatment, I had a 58% blast count (percentage of abnormal blood cells my bone marrow was producing) and the dire diagnosis was acute myeloid leukemia (AML).
At this point, thoughts about how long I might live, a funeral, leaving my family and all the life things I’d miss, began to occur, but they were not foreboding. My faith really became so real and meaningful at this point. I found myself becoming quite peaceful. Most of the negative emotions I’ve experienced first appeared about a year to a year and half after the transplant. I’ve always been good in a fight, it’s when the fight is over that I become emotional. It was probably close to three years after the transplant that I finally listened to Natalie and agreed to take some medication. My oncologist said I probably had agitated depression. When I saw my family physician in mid-July (2018), he said he’d been scoring my emotional state and it had improved from 16 a year or so ago, to a five currently. My faith sustained me through the medical care in Houston. I was at peace, trusting the will of God and the skill of my medical team. MD Anderson trains their staff to display confidence and it is powerful. There’s no, “Oh, we hope we can help,” it’s all, “This is what we do.” And the plan is stated in a way that you know, 1) they’ve done it many times before and 2) if it doesn’t work, they have more options. This environment made it easy to forget I was dealing with a terminal and not curable disease. Even today, I feel peaceful and at home in Houston.
Be the Match, is a wonderful program that takes mouth swabs of volunteers and enters them into an American and global registry with the goal of matching stem cell donors to patients who will likely die without a successful stem cell transplant. As my business colleagues discussed hosting a swab/registering event for me, I was amused by multiple calls from friends and colleagues who said, “I went to sign up with Be the Match but learned I’m too old!” Fortunately, the initial search for a donor to help me produced over 250 potential matches. This list was reduced to about a dozen that scored a perfect 10 out of 10 in the matching process. These were then evaluated on an additional four measures and one that scored 13 out of 14 was chosen. I’m just glad a young man who lived near Fargo, North Dakota decided to sign up. Ironically, he was flown to Minneapolis on Election Day 2012, where his miraculous stem cells were removed, flown to Houston and put into my body the very next day—November 7, 2012.
Please register with Be the Match or some other similar registry, you never know whose life you might save.
When I arrived on the isolation floor at MD Anderson Hospital for the high dose chemo, I was sent immediately to a shower room. There I showered and put on a sterile gown and was rushed into my room. Once there, I discovered a bedside commode, aka, potty chair and I was told to bag everything that came out of my body; I’ll just leave this part to your imagination. There was also a sink, where I was instructed on how to bathe and a wise nurse encouraged me to develop a daily routine. So, my years in the country playing alone, prepared me perfectly for 27 days in isolation.
There was a small room adjacent to mine where Natalie and visitors could see me through a window and we communicated by phone. I was just fine being alone and followed a daily routine of eating some breakfast, they cooked perfect bacon, taking my “bird bath,” as I named the sink bath and then, after a week or two, I felt like watching about five years of 24 on my computer. But, I could not read any of the six books I took. My sister brought my mom and kids down for Labor Day weekend. I’ve never seen as beautiful sight as my family in that window.
Natalie spent about 12 hours a day in the little room outside my window. As the days went on, she asked, then debated and finally begged, every nurse or doctor that entered my room to let her come in too. But they would not even consider it. Eventually, I suggested she get a job cleaning floors and once a day she could come in my room. It’s probably good I made that suggestion out of her reach!
On my last day of isolation, NASA flew the Space Shuttle right by my window. In the early 1960s, my dad got me up before daylight to watch history happen right before my eyes. Although I never saw a launch, my dedication to watching the space program makes it a source of comfort for me. So, I was thrilled to see the Space Shuttle on top of a 747 as it flew around Houston on its way to a museum in Los Angeles moments before I left the hospital.
After leaving the hospital, I mentally freaked out in a grocery store because: 1) I had choices I didn’t know what to do with and 2) the people had germs, which I might not be able to fight off. So, I went to the car. Praise the Lord, the high dose chemo worked, and my leukemia was in remission!
We went home the day after my discharge from isolation. We returned to Houston a couple weeks later for another round of chemo that was given outpatient. I was able to carry the chemo in a bag, which allowed us to get out of the hotel. I dubbed the chemo bag, my “European shoulder bag.” Then we were home another couple weeks before returning to Houston for the stem cell transplant.
What do you do with your time, knowing the transplant is coming up? I went to work every day while contemplating the possibility I was living my last days. A day or so before we left for Houston and the transplant, I left the office and drove to Mayflower, but my mom wasn’t home. So, I drove out west of town, where I used to hunt and fish with my dad, uncle and cousin. Then I went north into Conway, where I drove around the University of Central Arkansas campus I attended in the 70s and remembered my college days there. I also visited other places in town where my family and I went many times as I grew up. Front street in Conway had the Sterling’s store where I bought my baseball cards and the dance studio on the corner was where my sister took lessons.
We arrived in Houston for the transplant just before my 57th birthday. I was scanned, x-rayed and tested in about as many ways as you can imagine. Then, on my birthday, they needed to insert a port into a main blood vessel under my collarbone. This procedure created some debate: 1) do I take some medicine to calm me down and potentially not be able to enjoy a birthday dinner, which might be my last, or, 2) just do it. The nurse and I concluded I was fine without the meds. The doctor was behind schedule when she arrived. As she started the procedure, I jokingly said, “I hear you haven’t had much to do today!” I didn’t consider the fact that she had a scalpel and was cutting near the neck area of my body or that my face was covered, and she couldn’t see my smile. Fortunately, the line was successfully installed, and Natalie and I went to Outback where I enjoyed my favorite meal—steak and lobster.
We visited the transplant doctor on a Friday, before I was scheduled to enter the hospital on Wednesday, which just happened to be Halloween. After some discussion the doctor paused, likely to allow me to ask questions. I didn’t see any benefit in asking questions that had no certain answers or no answers that would help in any way. After a moment of my silence, she made two dramatic statements: 1) “We’ve refined the donor matching process so well, almost everyone’s transplant engrafts,” and 2) “We get almost everyone through the process alive.” Months later, a business acquaintance told me his father was told, before his transplant, that the survival rate was about 2/3rds. At this point I mistakenly said, “Wow, I was thinking I had about a 50/50 chance to survive.” She responded, “Well, there’s actually a 50% chance the disease will return after the transplant.” About a year after the transplant I was brave enough to ask if the 50% chance of the disease returning ever reduced and was told the odds reduce about 10% per year. This made surviving five years very meaningful. The challenging answer to my comment about survival confirmed it was best to not ask many questions. So, despite thinking, “Aren’t you dead when your blood counts are zero?” I said nothing when I was told the chemotherapy before the transplant would kill my immune system and take my blood counts to zero!
The day you enter the hospital for a stem cell transplant is called Day -7, I thought it should be called T-minus 7, after all, we were in Houston! The transplant procedure starts with hydration, then chemotherapy is given. The transplant is done on Day 0, or as the nurses call it, your rebirthday. I never liked that phrase because I consider myself reborn already by the blood of Jesus Christ.
The transplant is done using a modified version of isolation, and, this time I had a bathroom! Everyone that came in my room had to wear a mask, gloves and gown, except for Natalie who hardly left the room. This meant I could only see the eyes of my visitors. The isolation protocol required me to wear a mask, gown and gloves when I left the room. No physical contact was allowed anytime, so I couldn’t hug anyone.
The nurses refer to the first two weeks after the transplant as the “ditch,” and I was in it quickly. Just hours after the transplant, I developed a 104 degree fever that lasted over 12 hours. After a few hours break, the 104 degree fever returned for another 12 hours. I got another few hours of a break, then the 104 degree fever came back for eight more hours before it, thankfully, ended. I didn’t know what was happening—likely a very dangerous virus that I was fortunate to survive—and I didn’t ask. During the long periods of fever, I had a half dozen ice packs on my body and I dreamed of driving my boat across a smooth Greers Ferry Lake.
I was advised to gargle regularly. Before I got out of the ditch, I found out why. The chemotherapy caused my throat to feel like knives every time I swallowed. When the nurses found me spitting instead of swallowing, they brought me a suction device. This was a pretty miserable few days. I was in the hospital at Thanksgiving, which was after the fever, but the throat issues were still ongoing when the kids came to town. The kids’ presence helped a lot. I thought a lot about the annual family Thanksgiving meals I took for granted. Although I didn’t want to eat anything, I did think about my favorite Thanksgiving feast foods. I could almost taste my Aunt Nay’s meat beans.
Prior to entering the hospital, we attended a class for patients and caregivers to learn about the transplant process. One of the interesting comments to caregivers was to not be concerned when their loved one/patient did not eat. I may have eaten a little early in the month-long hospitalization, but after that I ate almost nothing. My pre-diagnosis weight dropped from 208 to under 160. My blood counts were approaching a safe level the week after Thanksgiving. But, the day I thought I would be released the doctor decided to keep me in the hospital. The next day when it appeared she was going to keep me another night I said, “If the only reason you’re keeping me is I’m malnourished, then the best thing you could do is let me out.” The doctor agreed, and we headed to our apartment.
On the way to the apartment, Natalie asked me what I’d like to eat, and I said, “chicken wings.” I’m not sure I’d ever eaten chicken wings, other than part of a fried chicken meal, so this was an odd food thought. I told Natalie to order me the smallest amount they had, which turned out to be eight. I expected to eat one or two. When we arrived at the apartment, I took my wings in and Natalie went to check the mail. After getting the mail, she eagerly asked, “How many wings did you eat?” I said, “all EIGHT!”
Surviving the first 100 days after a transplant is the big challenge. Thankfully, the medical teams work very hard to keep patients alive and the care doesn’t stop upon discharge from the hospital. Stem cell transplant patients must live near the hospital after discharge. Like all transplant patients, I went to the clinic daily after leaving the hospital. An Advanced Practice Nurse checked my vitals, reviewed my lab work and started an IV that lasted about three hours. Magnesium was the primary part of the IV, which could also provide needed general fluids. There was always the possibility of needing a blood transfusion. My APN, Cindy, was terrific. She served as a nurse, life coach and friend. After a couple weeks, she started giving us a day off and over time we were given two days a week off. I wasn’t expected to stay in the apartment all the time but was encouraged to avoid crowds when out, so Natalie and I would go to restaurants in the middle of the afternoon. I was instructed to not eat anything uncooked. Cindy said, “Send it back if it has garnish on it.”
In times of trouble, God provides angels to help. They don’t have wings and cannot fly, but they appear as friends and family. A business colleague, Becky, allowed us to use her apartment on some of our two to four-day trips in the summer of 2012. We’ve made many trips to Houston for checkups the last 5 ½ years. Checkup visits for cancer patients are somewhat similar to playing Russian Roulette; everything can be fine and then a bad test/scan result can change everything.
We were discharged to go home on February 8, 2013, which was day +98.
About the Author
Cancer entered Kenny's life at age 28 when his first wife was diagnosed with breast cancer. Later, he lost my dad to cancer. In 2012, he was diagnosed with leukemia and survived a stem cell transplant. In January 2018, he was diagnosed with prostate cancer and had surgery in March. He's known Jesus as his Lord and Savior since he was in the 5th grade. Sports has always been a huge part of his life since he was 8 in 1964, when the Arkansas Razorbacks took his heart. Kenny started a blog in 2018 to write short stories about specific issues from his life path. You can read additional posts written by him by visiting www.cancersportsfaith.wordpress.com.
There are places we visit during our lives that become part of us. We think of them fondly and run to them for comfort in times of trouble. Galveston Beach is such a place for me. As a young child I vacationed there with my family and the Galveston Jack Tarr Resort was the location of my high school senior trip. As a young adult, one of my first adult vacation sights was Galveston; on the beach during the day and in the Astrodome at night watching my Cardinals play the Astros.
I’ve realized that I most definitely use places for comfort. Regardless of where our place of comfort is, when we are there we are taken back to a place in time that we remember fondly and would love to return. When you are a few days from entering the hospital for a stem cell transplant and wondering about your odds of surviving, visiting a place of comfort is a way to relax. Natalie (my wife) and I went to Galveston on the weekend before my transplant. As the waves churned against the sandy shore on a breezy and mild late October day in 2012, I recalled the happy times with my family, my high school classmates and my adult vacations there.
Discussing the treatment plan following my MDS diagnosis in April 2012, my oncologist in Little Rock described how it’s necessary to put the disease into remission before a stem cell transplant can be done. Putting cancer into remission sounded like a great thing. But to accomplish it, they would put me in isolation, with no bathroom, and give me high dose chemotherapy. I thought, no thank you, let’s just keep the MDS in check with tolerable chemotherapy. But after barely two months of treatment, I had a 58% blast count (percentage of abnormal blood cells my bone marrow was producing) and the dire diagnosis was acute myeloid leukemia (AML).
At this point, thoughts about how long I might live, a funeral, leaving my family and all the life things I’d miss, began to occur, but they were not foreboding. My faith really became so real and meaningful at this point. I found myself becoming quite peaceful. Most of the negative emotions I’ve experienced first appeared about a year to a year and half after the transplant. I’ve always been good in a fight, it’s when the fight is over that I become emotional. It was probably close to three years after the transplant that I finally listened to Natalie and agreed to take some medication. My oncologist said I probably had agitated depression. When I saw my family physician in mid-July (2018), he said he’d been scoring my emotional state and it had improved from 16 a year or so ago, to a five currently. My faith sustained me through the medical care in Houston. I was at peace, trusting the will of God and the skill of my medical team. MD Anderson trains their staff to display confidence and it is powerful. There’s no, “Oh, we hope we can help,” it’s all, “This is what we do.” And the plan is stated in a way that you know, 1) they’ve done it many times before and 2) if it doesn’t work, they have more options. This environment made it easy to forget I was dealing with a terminal and not curable disease. Even today, I feel peaceful and at home in Houston.
Be the Match, is a wonderful program that takes mouth swabs of volunteers and enters them into an American and global registry with the goal of matching stem cell donors to patients who will likely die without a successful stem cell transplant. As my business colleagues discussed hosting a swab/registering event for me, I was amused by multiple calls from friends and colleagues who said, “I went to sign up with Be the Match but learned I’m too old!” Fortunately, the initial search for a donor to help me produced over 250 potential matches. This list was reduced to about a dozen that scored a perfect 10 out of 10 in the matching process. These were then evaluated on an additional four measures and one that scored 13 out of 14 was chosen. I’m just glad a young man who lived near Fargo, North Dakota decided to sign up. Ironically, he was flown to Minneapolis on Election Day 2012, where his miraculous stem cells were removed, flown to Houston and put into my body the very next day—November 7, 2012.
Please register with Be the Match or some other similar registry, you never know whose life you might save.
When I arrived on the isolation floor at MD Anderson Hospital for the high dose chemo, I was sent immediately to a shower room. There I showered and put on a sterile gown and was rushed into my room. Once there, I discovered a bedside commode, aka, potty chair and I was told to bag everything that came out of my body; I’ll just leave this part to your imagination. There was also a sink, where I was instructed on how to bathe and a wise nurse encouraged me to develop a daily routine. So, my years in the country playing alone, prepared me perfectly for 27 days in isolation.
There was a small room adjacent to mine where Natalie and visitors could see me through a window and we communicated by phone. I was just fine being alone and followed a daily routine of eating some breakfast, they cooked perfect bacon, taking my “bird bath,” as I named the sink bath and then, after a week or two, I felt like watching about five years of 24 on my computer. But, I could not read any of the six books I took. My sister brought my mom and kids down for Labor Day weekend. I’ve never seen as beautiful sight as my family in that window.
Natalie spent about 12 hours a day in the little room outside my window. As the days went on, she asked, then debated and finally begged, every nurse or doctor that entered my room to let her come in too. But they would not even consider it. Eventually, I suggested she get a job cleaning floors and once a day she could come in my room. It’s probably good I made that suggestion out of her reach!
On my last day of isolation, NASA flew the Space Shuttle right by my window. In the early 1960s, my dad got me up before daylight to watch history happen right before my eyes. Although I never saw a launch, my dedication to watching the space program makes it a source of comfort for me. So, I was thrilled to see the Space Shuttle on top of a 747 as it flew around Houston on its way to a museum in Los Angeles moments before I left the hospital.
After leaving the hospital, I mentally freaked out in a grocery store because: 1) I had choices I didn’t know what to do with and 2) the people had germs, which I might not be able to fight off. So, I went to the car. Praise the Lord, the high dose chemo worked, and my leukemia was in remission!
We went home the day after my discharge from isolation. We returned to Houston a couple weeks later for another round of chemo that was given outpatient. I was able to carry the chemo in a bag, which allowed us to get out of the hotel. I dubbed the chemo bag, my “European shoulder bag.” Then we were home another couple weeks before returning to Houston for the stem cell transplant.
What do you do with your time, knowing the transplant is coming up? I went to work every day while contemplating the possibility I was living my last days. A day or so before we left for Houston and the transplant, I left the office and drove to Mayflower, but my mom wasn’t home. So, I drove out west of town, where I used to hunt and fish with my dad, uncle and cousin. Then I went north into Conway, where I drove around the University of Central Arkansas campus I attended in the 70s and remembered my college days there. I also visited other places in town where my family and I went many times as I grew up. Front street in Conway had the Sterling’s store where I bought my baseball cards and the dance studio on the corner was where my sister took lessons.
We arrived in Houston for the transplant just before my 57th birthday. I was scanned, x-rayed and tested in about as many ways as you can imagine. Then, on my birthday, they needed to insert a port into a main blood vessel under my collarbone. This procedure created some debate: 1) do I take some medicine to calm me down and potentially not be able to enjoy a birthday dinner, which might be my last, or, 2) just do it. The nurse and I concluded I was fine without the meds. The doctor was behind schedule when she arrived. As she started the procedure, I jokingly said, “I hear you haven’t had much to do today!” I didn’t consider the fact that she had a scalpel and was cutting near the neck area of my body or that my face was covered, and she couldn’t see my smile. Fortunately, the line was successfully installed, and Natalie and I went to Outback where I enjoyed my favorite meal—steak and lobster.
We visited the transplant doctor on a Friday, before I was scheduled to enter the hospital on Wednesday, which just happened to be Halloween. After some discussion the doctor paused, likely to allow me to ask questions. I didn’t see any benefit in asking questions that had no certain answers or no answers that would help in any way. After a moment of my silence, she made two dramatic statements: 1) “We’ve refined the donor matching process so well, almost everyone’s transplant engrafts,” and 2) “We get almost everyone through the process alive.” Months later, a business acquaintance told me his father was told, before his transplant, that the survival rate was about 2/3rds. At this point I mistakenly said, “Wow, I was thinking I had about a 50/50 chance to survive.” She responded, “Well, there’s actually a 50% chance the disease will return after the transplant.” About a year after the transplant I was brave enough to ask if the 50% chance of the disease returning ever reduced and was told the odds reduce about 10% per year. This made surviving five years very meaningful. The challenging answer to my comment about survival confirmed it was best to not ask many questions. So, despite thinking, “Aren’t you dead when your blood counts are zero?” I said nothing when I was told the chemotherapy before the transplant would kill my immune system and take my blood counts to zero!
The day you enter the hospital for a stem cell transplant is called Day -7, I thought it should be called T-minus 7, after all, we were in Houston! The transplant procedure starts with hydration, then chemotherapy is given. The transplant is done on Day 0, or as the nurses call it, your rebirthday. I never liked that phrase because I consider myself reborn already by the blood of Jesus Christ.
The transplant is done using a modified version of isolation, and, this time I had a bathroom! Everyone that came in my room had to wear a mask, gloves and gown, except for Natalie who hardly left the room. This meant I could only see the eyes of my visitors. The isolation protocol required me to wear a mask, gown and gloves when I left the room. No physical contact was allowed anytime, so I couldn’t hug anyone.
The nurses refer to the first two weeks after the transplant as the “ditch,” and I was in it quickly. Just hours after the transplant, I developed a 104 degree fever that lasted over 12 hours. After a few hours break, the 104 degree fever returned for another 12 hours. I got another few hours of a break, then the 104 degree fever came back for eight more hours before it, thankfully, ended. I didn’t know what was happening—likely a very dangerous virus that I was fortunate to survive—and I didn’t ask. During the long periods of fever, I had a half dozen ice packs on my body and I dreamed of driving my boat across a smooth Greers Ferry Lake.
I was advised to gargle regularly. Before I got out of the ditch, I found out why. The chemotherapy caused my throat to feel like knives every time I swallowed. When the nurses found me spitting instead of swallowing, they brought me a suction device. This was a pretty miserable few days. I was in the hospital at Thanksgiving, which was after the fever, but the throat issues were still ongoing when the kids came to town. The kids’ presence helped a lot. I thought a lot about the annual family Thanksgiving meals I took for granted. Although I didn’t want to eat anything, I did think about my favorite Thanksgiving feast foods. I could almost taste my Aunt Nay’s meat beans.
Prior to entering the hospital, we attended a class for patients and caregivers to learn about the transplant process. One of the interesting comments to caregivers was to not be concerned when their loved one/patient did not eat. I may have eaten a little early in the month-long hospitalization, but after that I ate almost nothing. My pre-diagnosis weight dropped from 208 to under 160. My blood counts were approaching a safe level the week after Thanksgiving. But, the day I thought I would be released the doctor decided to keep me in the hospital. The next day when it appeared she was going to keep me another night I said, “If the only reason you’re keeping me is I’m malnourished, then the best thing you could do is let me out.” The doctor agreed, and we headed to our apartment.
On the way to the apartment, Natalie asked me what I’d like to eat, and I said, “chicken wings.” I’m not sure I’d ever eaten chicken wings, other than part of a fried chicken meal, so this was an odd food thought. I told Natalie to order me the smallest amount they had, which turned out to be eight. I expected to eat one or two. When we arrived at the apartment, I took my wings in and Natalie went to check the mail. After getting the mail, she eagerly asked, “How many wings did you eat?” I said, “all EIGHT!”
Surviving the first 100 days after a transplant is the big challenge. Thankfully, the medical teams work very hard to keep patients alive and the care doesn’t stop upon discharge from the hospital. Stem cell transplant patients must live near the hospital after discharge. Like all transplant patients, I went to the clinic daily after leaving the hospital. An Advanced Practice Nurse checked my vitals, reviewed my lab work and started an IV that lasted about three hours. Magnesium was the primary part of the IV, which could also provide needed general fluids. There was always the possibility of needing a blood transfusion. My APN, Cindy, was terrific. She served as a nurse, life coach and friend. After a couple weeks, she started giving us a day off and over time we were given two days a week off. I wasn’t expected to stay in the apartment all the time but was encouraged to avoid crowds when out, so Natalie and I would go to restaurants in the middle of the afternoon. I was instructed to not eat anything uncooked. Cindy said, “Send it back if it has garnish on it.”
In times of trouble, God provides angels to help. They don’t have wings and cannot fly, but they appear as friends and family. A business colleague, Becky, allowed us to use her apartment on some of our two to four-day trips in the summer of 2012. We’ve made many trips to Houston for checkups the last 5 ½ years. Checkup visits for cancer patients are somewhat similar to playing Russian Roulette; everything can be fine and then a bad test/scan result can change everything.
We were discharged to go home on February 8, 2013, which was day +98.
About the Author
Cancer entered Kenny's life at age 28 when his first wife was diagnosed with breast cancer. Later, he lost my dad to cancer. In 2012, he was diagnosed with leukemia and survived a stem cell transplant. In January 2018, he was diagnosed with prostate cancer and had surgery in March. He's known Jesus as his Lord and Savior since he was in the 5th grade. Sports has always been a huge part of his life since he was 8 in 1964, when the Arkansas Razorbacks took his heart. Kenny started a blog in 2018 to write short stories about specific issues from his life path. You can read additional posts written by him by visiting www.cancersportsfaith.wordpress.com.

about the author
Katie Braswell
Katie joined HealthTree as the Community Director for AML in 2021 and became HealthTree's Director of Education in 2023. Katie is a registered dietitian who is passionate about health literacy and patient empowerment. She loves to cook, travel and spend time with her newborn son, husband and dog.
More on Patient Stories
Trending Articles

Get the Latest Acute Myeloid Leukemia Updates, Delivered to You.
By subscribing to the HealthTree newsletter, you'll receive the latest research, treatment updates, and expert insights to help you navigate your health.