Allogeneic Transplant and Precursor Myeloma Cells with William Matsui, MD, Johns Hopkins
Episode Summary
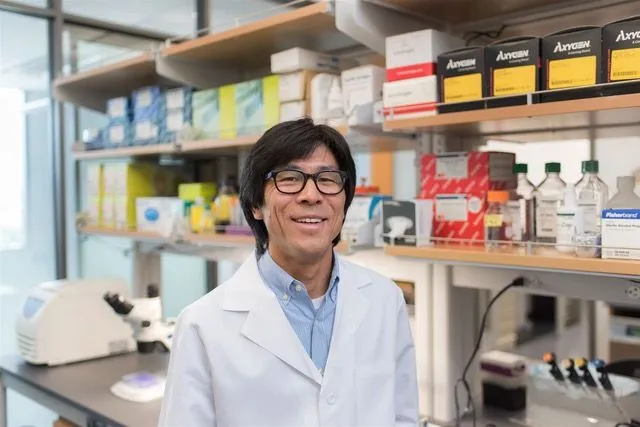
Dr. William Matsui, MD
Johns Hopkins University
Interview Date: February 16, 2018
Allogeneic (or donor) stem cell transplant has become much safer over the last 20 years. For those who have high risk myeloma features, it should be considered as a potential option. Dr. William Matsui, MD of Johns Hopkins University (and soon to be leading a myeloma practice in Austin, TX) shares his experience with allo transplant for all patients, regardless of their age. He notes that a younger donor may be better than a closer match, which makes it less difficult to find family donors. The paradigm has shifted for this treatment option that could be potentially curative for patients. His current study is to learn to how enhance and extend remissions for allo patients using an antibody called MEDI-551. Dr. Matsui also describes potential study for early or precursor B-cell targets which could help eliminate all myeloma and precursor myeloma cells.
Thanks to our episode sponsor, Takeda Oncology
Full Transcript
Jenny: Welcome to today’s episode of Myeloma Crowd Radio, a show that connects patients with myeloma researchers. I’m your host, Jenny Ahlstrom. And we’d like to thank our episode sponsor, Takeda Oncology, for their support of Myeloma Crowd Radio. Our show today is about allogeneic or donor stem cell transplants, and how to use this type of transplant which is actually the very first immunotherapy ever used in myeloma.
Dr. William Matsui from Johns Hopkins has made significant progress making this type of transplant safer, and is working on making it more effective, and his research also focuses on the early precursor cell, so we’ll be covering that as well.
I just want to note before we get started, if you’d like to meet Dr. Matsui in person, we welcome you to join us at the upcoming Myeloma Crowd Radio Roundtable on Saturday, March 24th, where Dr. Matsui and several other myeloma experts will be joining us to talk about the latest research for relapse myeloma, high-risk myeloma, and myeloma innovation. You can join this and three other roundtables this spring. So you can check out our website at myelomacrowd.org to find one near you.
So Dr. Matsui, welcome to the show.
Dr. Matsui: Thank you so much for having me.
Jenny: Okay. We’re so happy you’re here. Let me introduce you before we get going into our questions.
William Matsui is the Head of the Myeloma program at Johns Hopkins University. He’s also a Professor of Oncology at the Sidney Kimmel Comprehensive Cancer Center, and is a Member of the Department of Oncology, and a Member of the Graduate Program in Pathobiology and Cellular and Molecular Medicine.
He’s on the editorial and review boards of Haematologica, Immunology, and Immunogenetic Insights, is a SPORE recipient award researcher in lymphoma, and has won multiple teaching awards in the Johns Hopkins Department of Medicine and Oncology. He’s received the Kimmel Foundation Scholar, Sidney Kimmel Foundation for Cancer Research Award, as well as the LLS Scholar in Clinical Research Award. Presently and for the past six years, Dr. Matsui has served on the NCI Investigational Drug Steering Committee, and is the co-chair for the Cancer Stem Cell Task Force.
Just as I mentioned, Dr. Matsui is moving west in the next few months, and will be in Austin, Texas in June at the Livestrong Cancer Institute, a brand new school, part of the Dell Medical School at the University of Texas in Austin. I know patients that are little further west will be very, very excited to hear about that. And again, welcome to show.
Dr. Matsui: Thank you.
Jenny: Well, Dr. Matsui, why don’t we start by talking about allogeneic transplant as an immunotherapy? Because right now we hear about all these different immunotherapies coming out, and that was really the original.
Dr. Matsui: Yes. So allo transplantation was actually, like all transplantation, was never originally meant to be an immunotherapy. All transplantation, including autologous transplantation is the best example of this, using stem cells from yourself, or someone else, was really meant to be a way of overcoming the bone marrow toxic effects of high-dose chemotherapy. When people were doing this way back when, the thought was that they wanted to use blood or bone marrow from somebody other than the patient. The point was is that that person had no leukemia or cancer and so you weren’t transferring that back into the person.
As a side effect of that, people would get to have these immune reactions where the immune system of the donor would start to attack them. What people later figured out was those effects were actually beneficial in terms of controlling cancer. There’s been sort of a lot of questions about well, how does the immune system really play a part in controlling cancer? How does it do that? How does it work? I think that in the case of allogeneic transplant and myeloma, the best example that that is immunotherapy is that if you have a transplant and then you take more immune cells from the donor, if the patient has unfortunately relapsed after the transplant, you can give them those immune cells, and you can see the tumors go away actually.
So that’s really, in part, the evidence that it is an immunotherapy. Since we’ve been doing bone marrow transplants for almost easily four to five decades now, it’s probably the oldest established form of immunotherapy. It’s been used in all different heme malignancies and it has had a checkered past in myeloma. I think that at this point in time, maybe there’ve been enough advancements that we can actually go back and take another look at whether or not it might be a useful thing to add to the armamentarium things we do for myeloma patients.
Jenny: Well, let’s talk about that. So why allo in myeloma, and why not allogeneic transplant in myeloma? What would your take be on that?
Dr. Matsui: The reason why I think that allogeneic transplantation should be considered is that if you look at long-term studies, and these have been studies where people have been followed for over a decade, for sure, there are people who have undergone transplants and have no evidence of their disease coming back.
That, coupled with this idea that it’s immunotherapy, I think makes people believe that some portion of patients, for sure not every patient, but some portion of a group of patients is potentially cured by this approach. That’s the same in leukemia, and it’s the same in lymphoma. We use allo transplant in those diseases because we want to cure the patient. So that’s, for sure, the good part about it, right? Potentially curing someone is definitely a good thing.
The downside has been the side effects of it is number one. And then the other thing I would say is, is that in this day and age where you have many, many different therapies for myeloma, and patients obviously are living longer, is it better to just keep treating with a bunch of different things versus undergoing something like a transplant in general?
I think that on the side effects side, it got a very bad rep in the ‘90s, and people started doing allogeneic transplants sort of in a very concerted fashion in the mid early ‘90s. When I was doing my medical training, I went to medical school at UCSF but I did my internship and my residency at the University of Washington in Seattle, and that’s where the Fred Hutch is.
They were doing a lot of transplants specifically for myeloma at that point in time because myeloma is a very common disease compared to a lot of other heme malignancies. The problem was that at that time, there was almost a 50-50 chance that you would potentially die from the procedure. So that is super high. That is, for sure, unacceptably high especially for some disease that can be a chronic disease like myeloma. You don’t want to provide a 50-50 chance of not making it six months.
Jenny: Through the procedure, right.
Dr. Matsui: Yes, exactly. So that’s why it was very much sort of downplayed. One thing to think about is, is that well, why was it that myeloma patients became so sick from that procedure, and are those things that you could fix over time? So really, there are two major issues in myeloma patients. One is, is that if you give patients, for whatever reason, high-dose chemotherapy in the context of an allotransplant, and this is probably a little more chemotherapy, intensity wise, than you would get with melphalan, just giving two days of melphalan.
With that, it was difficult. There was a lot of organ damage that was done. People had a lot of pneumonia. There were some renal problems giving those higher dose of chemotherapy to people. And then the second issue is, is that even if you survived the chemotherapy part, then you have this immune system, and the question is, is that can the immune system tell the difference between you and your myeloma?
Because if it can go after the myeloma then that’s all good. If it now starts to attack you, that’s something called graft versus host disease (GVHD). You never see that in an autologous transplant because the immune system that you’re getting back in an autologous is your own so you’re not going to recognize yourself as being foreign. But if you’re bringing in a new immune system, it can start to attack your organs, and the most common ones are your skin and your liver and your gut. If there’s a very profound or intense reaction, then you can die from that immune reaction itself.
Back in the day, we were straddled with this conundrum of patients. We could potentially cure some of them, but we were probably hurting more people than we are helping at that point in time. I think there have been some major advancements in the last 30 years that have now allowed us to make the allo transplant much, much safer.
I think that if you get rid of this crazy nature of having every other person not make it through the transplant, then I think that now you can go back and consider it. But if you talk to most people who are myeloma folks, they have, at one point or another, tried allotransplantation, and it is more technically complex than doing an auto transplant, and there are many more complications from doing allotransplantation. So most people don’t like doing them.
I’m a bone marrow transplanter, and I transplant all diseases, including myeloma, and so those things that we see in allotransplantation for sure are more than an auto but those are complications you see for every disease, and so I think that that, to me, is not as big a deal.
I think that when you bring up the question of allo with most myeloma experts, I think that, like I said, it’s interesting to hear the spectrum of sort of comments you get back like it’s too dangerous.
Jenny: I get a very wide variety.
Dr. Matsui: Some people are still for them or still willing to try them. Other people say, “That is so dangerous, and half the people die, and then the other half get graft versus host disease.” Like I said, I think those are individuals who don’t necessarily do allogeneic transplantation. If they’re really only taking care of myeloma patients, they’re probably only doing autos.
There have been these incredible, I think, changes over time. There are two major ones. One is, is that instead of using high doses of chemotherapy, which is what we used to do, we used to give eight days of high-dose chemotherapy or four days of chemotherapy and four days of radiation. You can actually get by with very low doses of chemotherapy, and it’s very similar to the chemotherapy that you might get before you get CAR T-cells.
So that chemotherapy is really not designed to kill the myeloma. Its job is to try to sort of trim back at the normal immune system so that like in the case of CAR T-cells, you’re making space so that the CAR T-cells you’ve constructed can go in to your body and now have room to expand. For us in allo transplantation, we want to make the patient’s immune system as stupid as possible so that what we can do is put someone else’s bone marrow and immune system in there and it won’t get automatically rejected.
And those medications, there are two in particular. One is cyclophosphamide or Cytoxan, that’s used sometimes in myeloma. The other’s called fludarabine which is never used in myeloma. But those two together are very potent immunosuppressants. They’re not necessarily things that completely kill your bone marrow but they’re really designed to modulate the immune system and get rid of the immune system and the host.
So once you to do that then it becomes pretty easy to put another person’s marrow in. The big advancement about two decades ago was that you could use low doses of chemo rather than high doses of chemo. With that, over time, it’s become gentle enough that when I started doing transplants the upper age limit to have an allotransplant was usually in your mid-50s, and now, it’s well-tolerated enough that here at Hopkins we have no upper age limit actually.
Jenny: Wow. That’s incredible.
Dr. Matsui: Yes, and the other thing is, is that it used to be when you did a bone marrow transplant, you would be in the hospital for easily about seven or eight weeks, right? For us now here at Hopkins, we do 90% of them as outpatients. The vast majority of people never end up being an inpatient. So it’s mild enough that people are able to get up, walk around, go back and forth. And so we have a clinic, and they come back and forth to that outpatient clinic every day while they’re getting their transplant, but it doesn’t mean that they need to be cooped up in a hospital for 40 days and 40 nights anymore. It has gotten much, much better that way.
And then the second thing is, is this issue of graft versus host disease because that, by itself, is a major side effect. Like I said, you never see that with an autologous transplant but it can be severe. And there’s been a lot of efforts over the years to actually decrease the amount of graft versus host disease that you can get. Here at Hopkins, we have a specific way of doing it where we use cyclophosphamide again but we do it after you get your transplant. If we do that, we can take let’s say in the past, there used to be a serious graft versus host disease rates of about 50%. And now, we’ve reduced those to easily less than 10% and probably more like 5%.
If we can make it safer then, I think, it now opens up the possibility to see whether or not how curative is it, and are there strategies actually that you can try to think about to make it more effective over time? But I think that if you think about it, it’s hard to make things a whole lot safer and make them a whole lot more effective at the same time. It’s almost the opposite effect. If you make it more safe, it doesn’t work as well. But I think that since we’ve vastly improved the safety, now it’s time to really work on the efficacy.
So a lot of the trials that we do here at Hopkins have been really focused on well, how do we make sure that people don’t relapse as quickly or relapse following the allo transplant? Having a new immune system, I think provides a very good platform to now do a lot of things including trying to harness that donated immune system against myeloma.
Jenny: Well, that’s just totally incredible. I didn’t know that the low-dose chemo was what you’re using to do the actual transplant. Do you lose your hair and things like that if it’s such a low dose? You’re still taking Cytoxan during chemo.
Dr. Matsui: Yeah, so it’s a little bit different. I think that if you’ve experienced an autologous transplant, with melphalan, you’d probably lose your hair, you can have issues with nausea, you can have issues with mucositis where you get mouth sores so that it makes it difficult to eat and drink. So mucositis we almost never see with an allo transplant. Whenever you get chemo I think that there is some risk of nausea. I personally don’t think it’s as bad as -- from the chemo part, with the lower doses of chemo that we give compared to melphalan.
There are medicines, there are immunosuppressants that you get after the transplant to make sure you don’t get graft versus host disease right away and that you don’t reject the marrow you just got, those can cause some nausea but I think those are oral and so those are usually pretty manageable. I think with the low doses, the chance that you’re going to lose your hair completely is pretty low. I think it’s very low. I think you can get hair thinning.
Jenny: That’s incredible.
Dr. Matsui: But like I said, it’s amazing that, for me, having done this for about 20 years where when I started, the only people we were transplanting were very young individuals who got very sick from the procedure to now having people who are more advanced in age, you totally find, is an incredibly amazing difference. Like it’s night and day.
Jenny: That is incredible. I don’t think that word’s gotten out.
Dr. Matsui: Like I said, I think that if you go to a myeloma person and you say, “Look, I’m doing allo transplants,” you’ll get a checkered opinion about the procedure, and it is largely because I think most people have this memory of how horrible it was. I think that for me and for us at Hopkins, having improved the safety, I think that now if you have something that’s potentially curative, I don’t think you can really turn your back on that.
I think you got to at least figure out, just like with all treatments, who does it work best in? What is the best situation to do it in? What are the things that can help you along the way? What do you look out for? I think all of those things are now trying to foster that in myeloma. But like I said, unfortunately or fortunately, if you ask people about an allo, you get a very mixed bag.
Jenny: I believe that. With the graft versus host, there’s chronic versus acute GvHDs. So do you want to talk about the differences between those two? And what you’re talking about when you say it used to be 50% and now it’s less than 10%, that’s probably the acute, not the chronic, right?
Dr. Matsui: So it’s actually with both. So both used to be about 50%. Most people who get chronic graft versus host disease had acute graft versus host disease. Acute graft versus host disease is really sort of defined by timing. So it happens within the first probably three to six months right after the transplant. It is weird because the immune system that one receives really only attacks three organs in your body.
It attacks your skin so you can get a rash. It can attack your liver so you can become jaundiced or it can attack your gut so you can have nausea and diarrhea. After six months, chronic graft versus host disease can come up, and it can come up sort of at any time, and it can affect any organ in your body. Common places that it affects, it can affect your skin, again, where you get sort of tightening of the skin, something called scleroderma. You can get the attack of your tear glands, your lacrimal glands, and so your eyes are dry all the time. The same thing can happen for your salivary glands so you have a dry mouth all the time. It can affect things like your gut. It can attack your joints like arthritis. You name it, it can happen.
When I tell people about chronic graft versus host disease is that that is, as the name suggests, a longer-term issue. Many times, it’s controllable. You give people immunosuppression but if you need to give them immunosuppression for a long, long period of time then what happens is, is that they become very susceptible to infections unfortunately, so that’s the trade-off.
So what I tell people is that getting chronic graft versus host disease is really a trade-off from your myeloma. It’s like getting a different disease. You don’t want necessarily to have this huge burden of chronic graft versus disease. I think that that’s really a long-term issue. The acute part I think is an issue but it’s more of an immediate term issue, and I think it contributes, certainly, to the danger of the transplant but, like I said, it’s not like this chronic issue that you have to live with day to day to day to day for years after the transplant.
I think that there’s like a little bit of a philosophical difference in approach to acute versus chronic but, like I said, if you have really bad chronic GvH, it potentially is fully a trade-off from having myeloma.
Jenny: Right, and I know there are other different types of allogeneic transplants, so when you talk about you’re using the low-dose chemo and you’re reducing the graft versus host, do all of the types of allo transplant do that? The half-low, or the mini, or you know --
Dr. Matsui: Right, so using low-doses of a chemo is that’s what a mini transplant is. So a full transplant is where we’re going to give you eight days of chemo. For us, a mini is five days of chemo but it’s not super high doses, and one day of low-dose radiation. So it’s six days of treatment but it’s at a much lower dose than the full transplant. So mini transplant is using these lower amounts of chemo.
There are differences in terms of what the graft is that you get. The most common one that people believe is important is if you are having HLA, what’s called a fully-matched donor, so this is typically a sibling. If you think about it, these HLAs, there are like ten of them, so if your ten copies are the same as your donor’s ten copies that means your immune systems are somewhat in sync. So that should lower the amount of graft versus host disease. It should lower the chance that your immune system rejects the donor’s bone marrow.
In the past, for many, many, many years, the ideal donor is someone who has a perfect match. When they say perfect match, it’s an HLA match. So the issue is, is that that is fine if you are a ten-year-old with leukemia because you probably have a sibling who is young but if you are 70 and you have a sibling, then it’s unlikely that that sibling is going to be 20. So one question is, is that is there a difference with regards to the age of the donor? And so there certainly are.
One of the other ways to do it instead of having a fully-matched transplant -- if you get half of your genes from your mom, half of your genes from your dad, that means with each parent, you share half of their, what’s called, genotype. The other is, is that it means that your kids share half of your phenotype. In that way, if you said, “Well, okay. Instead of doing everyone fully-matched, maybe what we should do is think about using half-matched individuals.” Well, that would allow people who are older who probably have teenaged or adult-sized kids, maybe you could use their kids as a donor.
Normally, in the United States now, if we wanted to do an allogeneic transplant, it’s something like 40% of people will have a related sibling who’s fully-matched, that’s sort of the number. If you say now, what I want to do is I don’t care about them being fully matched. I just need people to be half-matched, well, that means that your parents could donate for you, it means your kids could donate for you, it means that your grandparents may be able to donate for you or your grandchildren may be able to donate for you. It means that your cousins may be able to donate for you, your aunts, your uncle.
So it ends up being that if you look at half matching, it’s something like 95% of people will have a match. It takes that matching issue or finding an equation a little -- or finding a donor somewhat out of the equation.
So the major issue using half-matched transplant is that in the past, they’ve been associated with tremendous rates of graft versus host disease, and that makes sense because half of it they recognize and then the other half they think it’s totally foreign. So there’s a really high risk of GvH.
The way that we’ve developed our transplants here at Hopkins is that by using this Cytoxan after the transplant, we found that if you have a half-matched individual versus a fully-matched individual, the graft versus host disease rate is exactly the same. So there’s no difference anymore.
And so now that allows you to sort of say, “Look, if I compare older pairs of siblings who get transplant versus patients and their kids who get transplanted, how did they do?” So it seems like the younger your donor is, the better patients do actually - across all diseases - and it’s this weird thing. It makes sense. You get a younger, more vibrant immune system, and that is probably better than getting immune cells and bone marrow cells that have been in a person for decades or more.
Jenny: That makes sense.
Dr. Matsui: So for us now, just about all of our myeloma transplants, if the patient is, let’s say, around 50 or older and they have a child who’s a teenager or older, I would use a kid who’s half matched over a sibling who’s fully matched but is 50 or older. So that changes the equation a little bit because there are many, many more people who can get transplanted. I think you’re doing better because you’re using younger donors.
Jenny: I just read an article from researchers that were in Australia about different types of cancers. And they said that it could be you know, how we’re setting all these genetic mutations? It could just be the status of the immune system which is allowing the cancer to grow. So maybe more study needs to happen on that and maybe we need to balance things out a little bit on this immune system status. So that makes a lot of sense that the stronger your immune system, the better impact you’re going to have.
Dr. Matsui: We, as humans, are probably optimal around the age 20 or something, and then it’s all downhill from there. I think that the closer you are to that, the GvH rates are better, the relapse rates are lower, there’s less complications with the transplant. Almost every parameter is better if you use a younger donor. So we have moved away from are you fully matched versus not. That is the major parameter at most cancer centers.
For us it’s really, what is the age of donors who are available to you? Like I said, we’ve used cousins, we’ve used grandkids if we have to. It’s been amazing also in that way where instead of now sort of you have a patient, you go and you get them typed to see what they have and what their relatives have, in the past many times you were like, “Well, unfortunately you don’t have a donor.” Now, you don’t even consider that that’s a possibility unless the person is adopted or something. I think it ends up being like that also is somewhat of a game changer.
Jenny: That’s amazing.
Dr. Matsui: Allowing more access to transplantation for older folks.
Jenny: Right, right. That’s amazing. You mentioned earlier now that you’ve been able to effect the safety and improve the safety now you’re thinking about how to make things better. I don’t know if you have any statistics about potential cure rates from allo or just even an idea of how effective it is but you’re using an antibody as well. So do you want to talk about that a little bit?
Dr. Matsui: We had actually looked at using sort of this method of controlling graft versus host disease. We had just published earlier, like at the end of last year, our experience looking at patients who had been transplanted using this approach, allo transplants, from 2003 to 2011. So what we wanted to do is make sure that we had enough follow-up for everybody. And in that analysis, it ended up being that the probability of being alive at ten years was about 50%, between 40% and 50%.
What we think as far as patients being in a sustained remission over a long period of time, it ends up being about 25% to 30%. In that analysis, nobody died from a complication of the transplant, and the graft versus host disease rates were, for acute, were 8% and for chronic, it was about 10%. When I talk to people I say, “It’s probably a one in three or a one in four chance that an allotransplant is curative in myeloma.” So one question is, is that how --
Jenny: Those are some pretty good odds when you start thinking about it like that.
Dr. Matsui: Yes. I think the question is, is if it’s safe, if you’re getting something out and you have less threat of something bad happening going in, then I think it becomes something that’s doable. If you said that it’s 25% of people are cured but you have a 50-50 shot of not making it six months, then it becomes a very different conversation and a very different equation.
And so right now, the issue is that how do we try to reduce the risk of relapse? What we found in other diseases is that if you use medicines and let’s say that they’re not really curative in the normal setting, and this is not a myeloma, this would be in this one leukemia called ALL or in this other leukemia called AML, what you can do is if you give medicines that are sort of effective at controlling the disease without a transplant and use those as sort of a maintenance after an allo, the patients do much, much, much, much better.
In this one disease, ALL, typically if you did a transplant in a specific type of ALL called Philadelphia chromosome-positive ALL, it’s about 30% of people are cured. If you give them tyrosine kinase inhibitor like Gleevec, afterwards it goes up to like 70%. So it can really improve things. I think part of that is that you have a totally known immune system now in place.
We’re trying to do that with myeloma. And other people have thought of this. There’s a national trial ongoing right now where people have an allo transplant. It’s a full transplant so it’s high-dose chemotherapy but what they get is they get ixazomib or Ninlaro after the transplant as maintenance. Then there have been some studies looking at using Revlimid as maintenance post-allo just like you would in the post-auto situation.
For us, we’ve been interested in this idea of cancer stem cells, and we think that those are more like B-cells rather than plasma cells. And so they have a different set of markers. One of the markers is CD19. One idea is that can you try to get rid of those cells because we think that those cells are responsible for the cancer growing back and for people relapsing.
Can we get rid of those using a strategy? One of the things that we identified was this antibody against CD19. CD19 is not expressed on the plasma cells, myeloma plasma cells generally. But can we give that medicine post-transplant to try and reduce the risk of relapse by getting rid of the cancer stem cells?
That’s one of the allogeneic transplant trials we have here at Hopkins. It’s a trial that’s specifically for myeloma patients. If you have leukemia, lymphoma, there are other trials but this is not the trial for you. It uses the same transplant we would do if we didn’t do the trial. And, really, the trial is only adding in this antibody you get at IV. You get it for about a year and then we see what happens.
The antibody itself has been used in a bunch of different diseases including -- there’s a study we did a number of years ago in myeloma. It’s pretty well-tolerated. There are not many side effects. We think that this would be potentially a strategy that is safe to try to reduce the risk of relapse.
Like I said, I think that there’s a lot of room to improve. One in four, one in three is better than zero but it is the majority of patients. I think that, for us, making it safer, we don’t have to study that anymore. What we should study now is how do we try to keep people in remissions and prevent them from relapsing. I think that when people ask, “Well, should I think about a transplant, an allo transplant? What are the specifics about it?” one thing I will say is, is that people tend to do better earlier on in their therapy or the course of their therapy rather than later on.
In the past, the other problem has been that many patients will come into an allo after they’ve failed everything else. I think that even there, you’re asking a lot for the allo to be affective. And so I think doing it earlier on -- there was just a report from the Hutch looking at allo transplants. Looked like patients who did it in the first line, after the first line of therapy, did much, much better than those who did it after a few lines of therapy.
And then the other is, is that I think that it’s important to try and have as little myeloma as possible when you start the allo transplant. The reason is, is that that the chemo we give you to prepare you for the transplant is not effective against myeloma so we’re not getting rid of more myeloma by doing that. If you think about it, we put in the other person’s marrow and the other person’s immune system, it takes some time for that immune system to grow and to start attacking the tumor. It’s probably three months.
And so if you have myeloma and you have a new immune system, then it’s a race, it’s a race between what is going to grow the fastest. If it’s your myeloma that grows the fastest then the immune system is not going to work. So you want to be in as good a remission as possible. It ends up being a little more difficult if you’ve been through multiple lines of therapy to get a full complete remission at that point in time.
So here, I’ve been recommending if we’re going to do it, I actually talk to people if they have -- the people I would consider are people who have higher risk disease based on their cytogenetics, and we tend to talk to more people who are younger versus older about it. But I have become more age-agnostic. If someone has high-risk disease based upon their cytogenetics, I will talk to them about doing an auto or an allo, and give them sort of multiple points of view or multiple choices.
Some people pick an auto or some people pick an allo. Most people I would say pick autos because that’s sort of the standard approach, and you don’t really know as well what you’re getting with an allo. Like I said, I don’t think it’s good to wait personally because I think that the ability for it to work, that opportunity you get for it to work I think really goes down if you’ve relapsed multiple times unfortunately.
Jenny: Yes, I agree. I think they say that about regular stem cell transplant too, doing it earlier upfront is a better approach before your disease has gotten more sophisticated. Well, let’s talk for a minute what you’ve mentioned before about targeting CD19 in these precursor stem cells or what you call the B-cells versus active myeloma cells. Can you explain that for patients who’ve never heard that before?
Dr. Matsui: Sure. So if you think about what plasma cells are, they are cells that their job is to be part of the immune system, and their job is to make immunoglobulins or antibodies. And so what we see as your M spike or what we see as your light chains, your lambda light chains or kappa light chains, those are part of antibodies or those are antibodies that are being made. And you normally need antibodies as part of protecting you from a bunch of different stuff in the world.
Those plasma cells, their normal counterpart, myeloma plasma cells are similar to normal plasma cells. And normal plasma cells, their job is to make antibodies. They’re like these little, tiny antibody-producing factories. Their job is actually not to make more themselves. If you want more plasma cells, it’s not plasma cells making more cells. It ends up being that they come from an earlier cell. So you have a more immature cell that now matures to become a plasma cell, and that cell is called a B-cell.
If in the normal system, B-cells are the things that are giving rise to plasma cells, then it may not be a crazy idea to think that in myeloma, that the same sort of system is set up where B-cells related to the myeloma are actually making myeloma plasma cells. So we sort of looked into this a number of years ago, and think that at least in some patients, the B-cells are pretty important.
The problem is that B-cells are really different to plasma cells. They are killed by different kinds of chemo. Things that work in myeloma generally don’t work so well in lymphoma for example, that are B-cells. So you have this dichotomy of the cells and what you can treat them with. And so that may be one of the reasons why many of the therapies we use are, unfortunately, not curative is because we’re doing a really great job getting rid of the plasma cells but those drugs that we’re using are not getting rid of the factory where these things are being made.
We have proposed this for many years because the allo transplantation thing to me is humorous because it’s a very controversial thing. So for me, this idea that B-cells were important was a tremendously controversial thing at the time. So now, when I talk to people about allos and they say, “Well, this is crazy,” blah, blah, blah, it doesn’t faze me as much because I think I went through the whole skepticism with B-cells way back when.
One question is, is that how do we know that B cells are important? And actually, it wasn’t my group or our investigators at Hopkins that provided evidence. There was actually a group at the University of Pennsylvania. What they did was they had these CAR T-cells. They were one of the first groups to generate CAR T-cells. So they had CAR T-cells but not against a myeloma protein. They were against B-cells. They were against CD19. So there are a couple of people up there, one is Carl June, the other is that Stadtmauer, and Dr. Garfall. They had a trial where they used those T-cells, the CD19 T-cells, in patients with myeloma.
In some of the patients, they saw pretty good effects of getting rid of tumor even though CD19 was not on the tumor cells. So that was a study that was published a couple of years ago. That, too, is highly controversial if you ask people but I think based upon that, one question is, is can we design CAR T-cell therapies that let’s say -- there are CAR T-cell therapies now that go after myeloma cells, those are against a target called BCMA. So one thought is can you combine a BCMA targeting T-cell to get rid of the myeloma with a CD19 targeting T-cell to try to get rid of the B-cells? That’s a study that people are thinking about doing in a couple of different places, one for sure is up at the University of Pennsylvania.
For me, I think that there’s potentially some utility in doing this. I think that in the post-allo transplantation, this is probably the best time to use any immunotherapy whether it be CAR T-cells, whether it be antibodies because the immune system is just much, much better than the immune system in the patient was because that was hampered by myeloma. I think that doing this trial where we give this antibody against CD19, in my own mind, is sort of a value added thing where I don’t think there’s going to be side effects from it.
Of course, we have to do it under a clinical trial to figure out whether there are but given that it’s been pretty safe in patients who haven’t had a transplant, I think that there’s hopefully some benefit to that in terms of preventing relapse without adding a whole lot in terms of side effects and toxicity. So that’s sort of the rationale for the trial we have right now.
Jenny: Well, that sounds great. I think it’ll be so fascinating to see. And what stage is it in, what phase of the trial is it in?
Dr. Matsui: It’s a phase 2 trial. It is one that is sponsored, in part, by the NIH and it’s, in part, sponsored by a company that makes the antibody, MedImmune which is AstraZeneca now. We just finished our first patient, and we have a couple more that we’re getting ready to do allos in, and then we’re signing them up for this trial.
I think it’s an ongoing effort. I think that it’s interesting. One thing that’s interesting to me is, is that, really, the push to do more allos here over the last, I would say, two years maybe. And in the beginning, there were really no patients that we would consider doing allos in but seeing that they’re relatively safe, if it doesn’t work you can still go on to other therapies. So over the last I would say probably a year, a year and a half, I’ve gotten a lot of referrals specifically for allos. I think it’s nice to see that some people are interested in at least finding out whether or not that might be an approach that they could think of.
Jenny: That’s wonderful and I think it’s a great option for people.
Dr. Matsui: Like I said, I think having a conversation with someone about it, it doesn’t mean that you go and you talk to someone about it, that that’s what you’re going to get. I think you have to go into the details and figure out is it for you or not, are you the right person to do it in? If you have low-risk disease I would say, “Look, there are better things out there. And we may not even need allo transplantation. We may have curative things in ten years. And if you have low-risk disease, you’d probably make it that long.” So I think it really is a pretty involved conversation that’s very, very specific to an individual patient.
Jenny: I want to ask one more question before I open it up for caller questions. When you talked about using drugs that were for the B-cells like the CD19 target or other types of B-cell cancers, have a lot of different myeloma specialists tried to combine kind of the standard care therapy in myeloma with something like that besides this antibody that you’re using to see if that can even work?
Dr. Matsui: Yes, so we had done a trial using a different antibody called Rituximab which is very commonly used for lymphoma, and we did that almost a decade ago probably, and we didn’t really see anything. I think that we understood some reasons over the years why we think that that’s the case. I think that this antibody is better than that antibody. It’s a controversial enough thing.
The other thing is that most myeloma people are not like lymphoma people. Most myeloma people are pretty specialized. I think that the ideas -- I think many of the diseases, like I said, the therapies are the same. We know how to Velcade. We know how to use IMiDs. When other people try to use them in other diseases, it’s a bit of a head-scratcher for them.
I think that the comfort with combining those types of strategies I think, for sure, number one has to be done on a clinical trial, and number two, I don’t know if that really hit the radar of a lot of people. Like I said, we have our data, and it is super controversial still but that’s what science is for, is to sort of figure out and answer these things.
Jenny: And try things out.
Dr. Matsui: Well, yes, and figure out what is really going on. But I think that that’s sort of what I would say is that I think some people are pretty open-minded and other people just say, “Look, forget it. That is completely made up and false. Let’s not even think about that.” Like I said, it’s science. I think if you do things under the right conditions like doing them in a clinical trial, you don’t just make them up on your own, and you explain what is going on to the people who are enrolled on the trial, then I think that’s probably the best situation to try and figure, actually, these things out.
Jenny: Wonderful. Well, let me open it up for caller questions. I still have more questions but I don’t know how much more time you have. So let’s just go ahead with caller questions.
If you’d like to ask Dr. Matsui a question, you can call 347-637-2631, and push 1 on your keypad. And we’ll start with our first caller, go ahead.
Caller: Hi. Good afternoon, Jenny and Dr. Matsui. Thanks so much for this interview today. The information that you’re sharing today is just so fascinating. Just to clarify, is this trial that you’re speaking of, the allo trial, the CD19 targeted antibody, is it for newly diagnosed high-risk patients or is it for relapsed and refractory patients?
Dr. Matsui: So it’s actually for both. For newly diagnosed high-risk patients, it’s based upon either your cytogenetics or your gene expression profiling if that’s something that’s still done. For newly diagnosed patients, that’s the thing. And people, like I said, need to go into a good remission with their initial chemotherapy. As far as relapsed patients go, it is open for relapsed individuals. The population we had initially been focusing on were patients who’ve relapsed pretty quickly after an auto.
I think that if there’s relapse that occurs within 18 months of having the auto, historically, that’s been a tough group of patients to treat long-term, and so we focused on those. But like I said, I think over the last year and half, I think the important lessons that we’ve learned is that you really need to be in a very good remission if a CR is possible going into the transplant because you really got to give that new immune system a fighting chance and time to grow.
Caller: So an allo transplant at initial diagnosis is actually a practical consideration based upon this trial design?
Dr. Matsui: It is but, like I said, if you asked, I don’t know, 100 myeloma experts and you said, “Look, I have a young patient that has the worse of the worst. They have a 17P or something really bad, what would you do?” I think some people would consider an allo transplant at that point, but the vast majority would not. They would say to go on to an auto transplant and maintenance.
So patients are eligible, and like I said, try to have as balanced a conversations as possible. These are the standard approaches. This is what auto transplant entails. This is what you’d probably get out of an auto transplant. And this is the potential of an allo, and try to help the person think about it and make some decisions that way. People say, “Well, if I send them to you, you’re just going to do an allo transplant.” I say, “No, no, no, come on.” Part of talking to people is explaining what these different options are. It’s not like the vast majority of people who come to see me for a transplant --
Caller: I don’t think you’re going to slap the handcuffs on them and tell them, “You can’t leave until you get the allo.”
Dr. Matsui: Yes. The majority of people still vote to do an auto transplant and I think that that’s fine as long as they feel comfortable with that decision, as long as they feel they got the right information.
Caller: It’s obviously standard of care, and everybody pretty much leans towards what we know in standard of care. But I think at the back of my mind I always think, “Well, geez, standard of care is not curing anybody so why not take the --”
Dr. Matsui: I am totally with you. That’s sort of the approach we take. And like I said, I think that we’ve done a lot here to make transplantation safer. I think that that is one argument that in the past, was a very valid one. I think that that is actually not that valid an argument anymore that it is much, much more toxic than an auto.
Caller: I understand and respect the fact that studies need to be completed in order to validate these premises but I thank you for pushing the envelope because it just may end up being something that we will need in the myeloma community.
Dr. Matsui, I have a question though because it always tends to puzzle me, and I think I kind of fall back to the fact that this disease is so heterogeneously distributed throughout the marrow. Bone marrow bias is what I generally refer to it as. The sample and corresponding results are only as good as the sample procured.
If you’re going to kind of be considering whether you’re a high risk or standard risk, how does the bone marrow sample bias affect the determination of the actual cells, the disease phenotype, at any given point whether it’s a diagnosis, a relapse, using the MRD testing? Can you help me better understand that? Is there a way to overcome that?
Dr. Matsui: There is a lot of what’s called intratumoral heterogeneity. In each patient there are, like if you sort of said, “Look, this myeloma has this number of mutations or these specific mutations,” you could have other myeloma cells and have for sure, some shared mutations but variable other ones, and so that’s where the heterogeneity comes in. I think that the other thing you can see is that your genetics or cytogenetics changing over time. That’s probably an evidence of heterogeneity.
So this issue of sampling is a real issue. Nobody wants to get six different bone marrows to sample six different places. You got to go with what you have. We know that certain abnormalities are bad from doing a single marrow. So I think that part is okay. Typically, what I think about is if patients are not really responding well especially to their induction therapy, I like to re-marrow them just to make sure that there’s no -- something else that we didn’t catch the first time. Like I said, there’s no perfect strategy. Trying to deal with --
Caller: Yes, because that would make sense. If you found the high-risk markers initially, you’re kind of okay with the choice but when you don’t and you’re being told that you’re standard risk and you’re kind of going at standard of care approach, that’s a scary thought because --
Dr. Matsui: Yeah, and I think that if you’re a standard risk, then your myeloma should act in a standard way, right? And if it’s not acting in that way, I would actually go back and try to re-figure it out. There’s something weird, right?
Caller: Good approach.
Dr. Matsui: And so if there’s something weird, then I don’t think you can just sort of blindly say, “Look, this is low-risk disease, and so you got low-risk disease.” I think that low-risk disease responds well to chemo. And so I think that if you’re not seeing responses then perhaps rechecking would not be a bad idea.
Caller: Does the aspirate sample need to be the first pull for the MRD testing or any type of testing? And if yes, is there a consensus from center to center doing these types of tests?
Dr. Matsui: I think that for most tests, I don’t think that the first pull is always done. I think that there is issues depending on -- I think if you do two pulls, I think the second pull is probably as good as the first pull. I think that if you’re doing five pulls, I think the fifth pull is probably not very useful. But I think that at least a couple of pulls I think is okay. I think that there are pretty standard ways that we do it, the order in which we get marrow for tests and blood tests.
We send off first what samples we use for each tests. I think that’s very similar in many different centers. And so I think that as long as it’s uniformly done, I think that you can at least have confidence in that. But is it a perfect system? For sure, it’s not. It’s difficult. Everyone know it’s difficult doing marrows. Sometimes, it’s like cake and other times, it’s really difficult. There’s no explanation for it. I think in those ways, it is a little bit of a skittish way of doing things.
Caller: Well, thank you so very much for your time today. I wish you the best of luck and hoping that maybe someday the Livestrong Center will also open up a satellite on the East Coast again so that we can get you back on the East Coast as well. So good luck. And Jenny, thanks so much for taking my calls.
Dr. Matsui: Sure. Thank you.
Jenny: Thanks for your questions. Good questions. So we have another call, go ahead with your question.
Caller: Hi, Dr. Matsui. I don’t want to take a lot of your time. I know we’re just about done with the call but I just want to thank you for everything you’ve shared. It’s been so helpful. My question is regarding the different cancers you’ve worked with. It looks like you haven’t fully worked with myeloma but you’ve branched out to other cancers as well. So what I’m wondering is what lessons have you learned while working with myeloma in comparison to the other cancers you’ve worked with, and also, how might your experience with other cancers and working with these cancers impact myeloma?
Dr. Matsui: We’ve worked on leukemia and the other thing that we’ve worked on is pancreatic cancer. We’ve done the same sort of thing looking for cancer stem cells and all of those diseases. Really, people always ask, “Why are you doing this?” The reason why is because I train a lot of people, and if people have specific interests, I want them to follow those interests. I don’t want to force a leukemia person to become a myeloma person.
So that’s how they’ve sort of developed. I think that in some cancers, it’s really well-understood like leukemia where stem cells are, how they’re related to other cells. I think that that is enormously useful as a roadmap for us to study myeloma, and that work has been going on in leukemia for much longer than our work in myeloma.
I think in pancreatic cancer, the one thing is that it is, I would say, a little bit easier to study the environment. I think that we know the environment is important to myeloma but how do you study it because it’s inside of a bone? You pull it out and it’s a bunch of liquid. And so in solid tumors you get chunks of tumor and you can sort of see what cell is next to what and what are they doing.
I think that from pancreatic cancer, we’ve learned a tremendous amount of how do things in the environment regulate cancer stem cells in pancreatic cancer? I think that that is very helpful for us because now we started thinking about well, what are the things that really control these cells in myeloma?
Having different ways to get at a problem I think is incredibly helpful. It hopefully prevents you a little bit from getting tunnel vision and thinking that everything you do is right. I think that we’ve learned a lot from those other -- my lab has learned a lot from studying those other diseases. For me clinically though, I only see myeloma patients, I am a transplanter doing other diseases but all of my time in the clinic is seeing folks with myeloma and other plasma cell diseases. So it’s my first interest, the thing that I’m, for sure, most interested in but I think that the other thing are, like I said, very helpful.
Caller: Yes. That’s great. Thank you so much.
Dr. Matsui: Sure.
Jenny: Okay. Thank you so much. Well, Dr. Matsui, thank you so much for joining us. I think your work is really exciting, and I hope you stay open-minded.
Dr. Matsui: Oh, yes. I don’t think that that will be that difficult. Well, thank you so much for having me.
Jenny: Well, we’re just really appreciative for all you’re doing, and we encourage people to attend the roundtable so they’ll meet you in person and ask a few questions about their type of myeloma and other things like that that I know you’ll talk about there, and also to visit you in Austin when you get there. We’re very excited for you. We’re just thrilled that you’ll be leading that program.
Dr. Matsui: I’m excited for myself too.
Jenny: And you’ll like the weather a lot better probably.
Dr. Matsui: Yes. I think that that’ll be nice.
Jenny: Okay. Well, thank you so much again for joining us. We’d like to thank our listeners for listening to Myeloma Crowd Radio, and invite you to tune in next time to learn more about the latest in myeloma research and what it means for you.
Trending Articles
Upcoming Events
Have Any Questions?
Thank you for your interest in the event. If you have any questions, we would love to help!
Feel free to give us a call or send us a message below.

Get In Touch With Us
1-800-709-1113
Support@healthtree.org
More Podcast Episodes
Get the Latest Non-Hodgkin Lymphoma Updates, Delivered to You.
By subscribing to the HealthTree newsletter, you'll receive the latest research, treatment updates, and expert insights to help you navigate your health.
Together we care.
Together we cure.