CLL Affects B-Cells, So What Is a B-Cell?

Understanding B-Cells
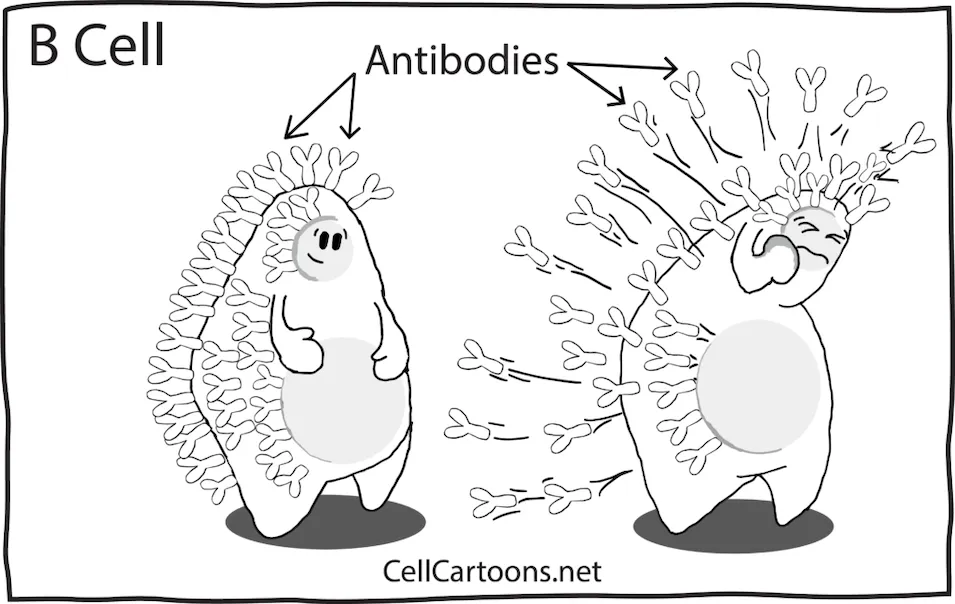
B-cells are part of the body’s immune system and protect against pathogens like harmful bacteria or viruses. They are created mainly in the bone marrow (some also in the lymph system) and circulate the body’s fluids (bloodstream and lymph fluid).
If a B-cell comes across a pathogen and its receptor matches the pathogen’s antigen binding site, the B-cell will lock onto the pathogen, ensuring it does not replicate and won’t infect other cells. Binding to the pathogen also signals other immune system cells to target the invader.
To check if copies of the same pathogen are in other areas of the body, the B-cell will create and send antibodies throughout the body’s fluid to attach to the replications of the original pathogen, immobilizing them and tagging them for pickup.
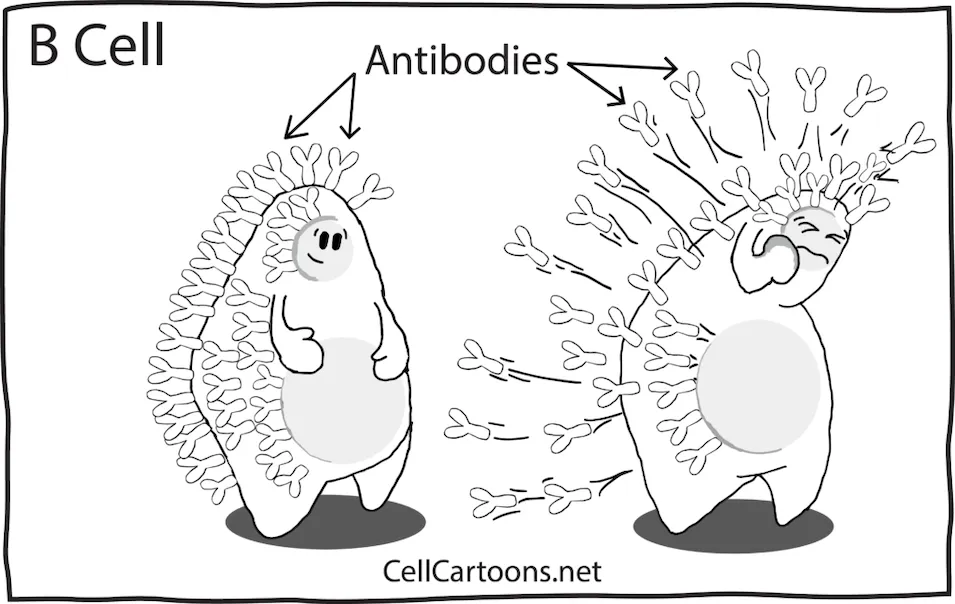
(Image source: CellCartoons)
How Are CLL Cells Different from Normal B-Cells?
Chronic lymphocytic leukemia (CLL) cells differ from normal B-cells because part of the cell’s DNA is deleted or changed, which may cause the cell to be unable to work well and avoid cell death. This allows the ineffective cell to keep multiplying. In most CLL cases, the replication of the mutated B-cell happens slowly.
How Did My B-Cells' DNA Become Damaged?
Reasons the B-cells' genetic instructions became damaged to turn into CLL are believed to be from either:
- A pathogen, such as a virus, and the body's immune system was too weak to remove the infected B-cell, allowing it to multiply
- From excess and chronic oxidative stress
- The patient may have inherited damaged DNA
What Can Be Done to Remove the Dysfunctional B-Cells (CLL)?
Thanks to recent medical advances, modern targeted therapies are designed to remove or limit the progression of CLL cells while leaving most of the body’s healthy cells alone. Although these are not yet a cure for CLL, for many patients, they help control the cancer for long periods of time.
The body also naturally produces cancer-killing immune system cells like T-cells. In diseases like CLL, the immune system cells may become exhausted and not work effectively to kill the cancer. Learn about immune system exhaustion here.
Summary
B-cells are important immune system cells that protect the body by identifying and tagging harmful invaders like viruses and bacteria. In chronic lymphocytic leukemia (CLL), B-cells become damaged, multiply abnormally, and stop working properly. Modern targeted therapies can help patients control cancer progression.
Sources:
Understanding B-Cells
B-cells are part of the body’s immune system and protect against pathogens like harmful bacteria or viruses. They are created mainly in the bone marrow (some also in the lymph system) and circulate the body’s fluids (bloodstream and lymph fluid).
If a B-cell comes across a pathogen and its receptor matches the pathogen’s antigen binding site, the B-cell will lock onto the pathogen, ensuring it does not replicate and won’t infect other cells. Binding to the pathogen also signals other immune system cells to target the invader.
To check if copies of the same pathogen are in other areas of the body, the B-cell will create and send antibodies throughout the body’s fluid to attach to the replications of the original pathogen, immobilizing them and tagging them for pickup.
(Image source: CellCartoons)
How Are CLL Cells Different from Normal B-Cells?
Chronic lymphocytic leukemia (CLL) cells differ from normal B-cells because part of the cell’s DNA is deleted or changed, which may cause the cell to be unable to work well and avoid cell death. This allows the ineffective cell to keep multiplying. In most CLL cases, the replication of the mutated B-cell happens slowly.
How Did My B-Cells' DNA Become Damaged?
Reasons the B-cells' genetic instructions became damaged to turn into CLL are believed to be from either:
- A pathogen, such as a virus, and the body's immune system was too weak to remove the infected B-cell, allowing it to multiply
- From excess and chronic oxidative stress
- The patient may have inherited damaged DNA
What Can Be Done to Remove the Dysfunctional B-Cells (CLL)?
Thanks to recent medical advances, modern targeted therapies are designed to remove or limit the progression of CLL cells while leaving most of the body’s healthy cells alone. Although these are not yet a cure for CLL, for many patients, they help control the cancer for long periods of time.
The body also naturally produces cancer-killing immune system cells like T-cells. In diseases like CLL, the immune system cells may become exhausted and not work effectively to kill the cancer. Learn about immune system exhaustion here.
Summary
B-cells are important immune system cells that protect the body by identifying and tagging harmful invaders like viruses and bacteria. In chronic lymphocytic leukemia (CLL), B-cells become damaged, multiply abnormally, and stop working properly. Modern targeted therapies can help patients control cancer progression.
Sources:

about the author
Megan Heaps
Megan joined HealthTree in 2022. She enjoys helping patients and their care partners understand the various aspects of the cancer. This understanding enables them to better advocate for themselves and improve their treatment outcomes.
More on Core Education
Trending Articles
Get the Latest Chronic Lymphocytic Leukemia Updates, Delivered to You.
By subscribing to the HealthTree newsletter, you'll receive the latest research, treatment updates, and expert insights to help you navigate your health.
Together we care.
Together we cure.