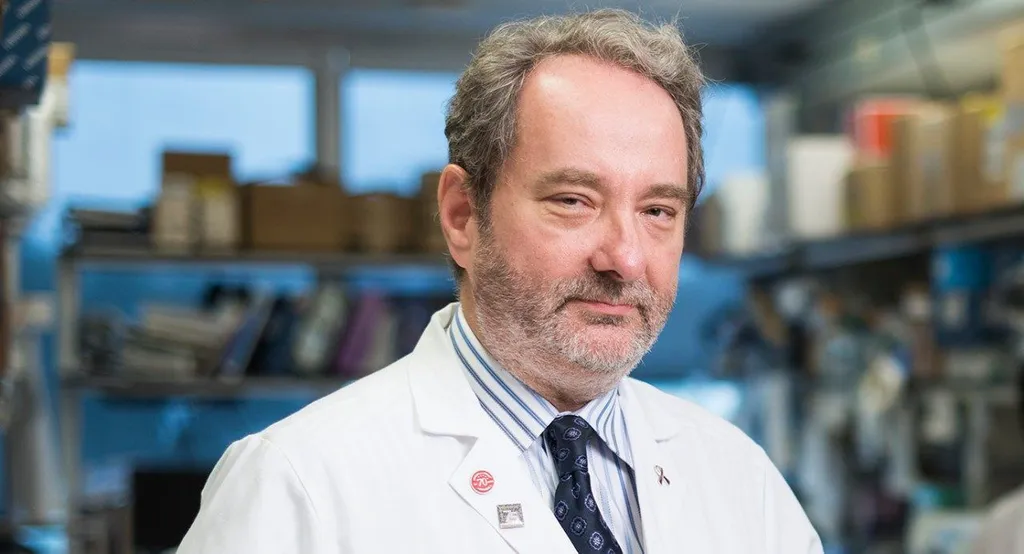
Looking Forward into 2022 in Multiple Myeloma With Robert Orlowski, MD, PHD, MD Anderson Cancer Center
Episode Summary
Robert Orlowski, MD, PhD
MD Anderson Cancer Center
Interview Date: February 7, 2022
Where is myeloma headed in 2022? Dr. Robert Orlowski of MD Anderson Cancer Center shares myeloma treatment trends and insights for the coming year. Learn more about how precursor conditions like MGUS and smoldering myeloma are being treated with newer therapies like daratumumab and isatuximab, how newly diagnosed myeloma is being considered in a more personalized way and what you could consider for treatment as a relapsed/refractory patient.
Thanks to our episode sponsor

Full Transcript
Jenny: Welcome to today’s episode of Myeloma Crowd Radio, a show that connects patients with myeloma researchers. I’m your host, Jenny Ahlstrom. We’d like to thank our episode sponsor, Bristol Myers Squibb, for their support of this Myeloma Crowd Radio show program.
Now before we get started with today's show, I just want to mention that if you are looking for help with your myeloma, we have over 150 (now 170) experienced and trained myeloma patients and caregivers who are myeloma coaches, and are willing to help you on a one-on-one basis. You can go to either healthtree.org and click on the Myeloma Section, or you can go to myelomacoach.org. and search for the type of coach you want and request a coach. They can work with you temporarily or on a long-term basis. You get to pick the coach you work with. We have coaches with specialty experience, as well as specific therapies, financial issues or other topics. If that's something that would be helpful to you, please connect with a myeloma coach today.
Now onto our show. This is one of my very favorite shows that we host every year to learn what we have to look forward to in 2022. With so much going on, it's very helpful to get an expert's bird's eye perspective of the most interesting progress being made. Unlike other shows where we discuss one topic in depth for the hour, this show will discuss many topics. It might be pretty fast-paced, although Dr. Orlowski is a pro in making complex topics easier to understand. Just know that we'll be doing a full transcript of the show that you'll be able to reference at a later time.
Dr. Orlowski, thank you so much. Welcome to the program. I love doing this show with you every year.
Dr. Orlowski: My pleasure. Thank you for inviting me every year.
Jenny: Let me just give a brief introduction for you before we get started. Dr. Orlowski is Chairman and Director of The Myeloma and Professor of Medicine in the Departments of Lymphoma/Myeloma and Experimental Therapeutics, Division of Cancer Medicine at MD Anderson Cancer Center. He serves as the chair of the Southwest Oncology Group, which is called SWOG, that is a clinical trial development group, nationally, and is a member of the NCI Steering Committee, the Multiple Myeloma Tissue Bank Steering Committee, the Computerized Provider Order Entry Steering Committee, BMT Committee, and American Society for Biochemistry and Molecular Biology.
Dr. Orlowski is on the editorial board of Hematology and the Journal of Clinical Oncology. He has received many awards over a number of years, including the Leukemia and Lymphoma Society’s Scholar in Clinical Research, the LLS Man of the Year Award, the Emil Frei III Award for Excellence in Translational Research from MD Anderson, and is a recipient of an ongoing SPORE grant from the NIH. He also has a myeloma daily paper that I suggest you subscribe to, called Myeloma Daily, and you can find that at paper.li or find him on Twitter at @myeloma_doc.
Dr. Orlowski, we have a lot to talk about. Maybe we just go in order of type of disease, start with the most important findings for maybe MGUS and smoldering myeloma patients.
Dr. Orlowski: Thanks very much. I did also want to take the opportunity, I hope it's not too late in the year, but to wish everybody a wonderful 2022, and also to hope that this will be the worst year ever for myeloma cells with not just billions and billions, as Carl Sagan would say, but trillions and trillions of them getting killed off by our better chemotherapy agents and immunotherapy agents. Hopefully, this will be the best year ever for myeloma patients.
Jenny: We hope so!
Dr. Orlowski: I think you wanted to start talking about MGUS and other precursor states and what we've learned, especially from ASH. I think that there's a couple of things that I would probably highlight, and a lot of them come from the so-called iStopMM study, which actually is a nice acronym for the Iceland Screens Treats or Prevents Multiple Myeloma. This is a screening, as well as treatment and prevention study, as the title suggests.
I think the couple of abstracts from that effort that came out, one in particular that will be interesting in terms of the, unfortunately, still ongoing COVID pandemic is that they found that patients with MGUS seemed not to have an increased risk for severity nor an increased susceptibility to COVID-19 infection. Although, unfortunately, sometimes, for more advanced myeloma, that did seem to be the case.
It seems also from other studies that have been published that MGUS patients have roughly equivalent responses to the vaccines against COVID, as do patients without MGUS. It still highlights the importance of everybody getting a COVID vaccine, but for those with MGUS, they probably need to worry a little bit less about the possibility that they will get really ill, if they do get COVID. Or at least their risk is no greater than the average patient.
Jenny: Okay, that's great.
Dr. Orlowski: One of the other abstracts that came out of the iStopMM study was looking at whether a certain frequency of follow-up was better than others, in terms of identifying patients with more disease severity. There were actually three different groups; one was just follow-up on an as-needed basis, one was a more regularly scheduled follow-up, and a third was more intensive even than that. As you might imagine, the people who were screened more frequently had more cases that were picked up.
I think people often think of MGUS as a benign condition, and one that doesn't need a lot of attention. I think it is still a benign condition for the most part, but it is important to follow patients closely because they can, unfortunately, sometimes, progress to myeloma. They also are at increased risk of other tumors. The notion that a benign disease can do well with neglect, I think is not correct. Even if you have MGUS, do keep seeing your doctor on a regular basis and make sure that he or she does the surveillance needed to make sure that you're safe.
Jenny: Great advice.
Dr. Orlowski: There also were some questions, I think, about new ways to hopefully reduce the risk of progression, and metformin is a compound that comes up pretty often. This is, of course, an oral drug that is used in many people with diabetes. There are suggestions, especially from other cancer types, that there may be a chemo prevention role for this drug. There are trials ongoing.
Some studies that looked at data from databases have suggested that metformin may be helpful, but interestingly, I tweeted last month about a laboratory-based study that showed that metformin actually increased the stickiness of myeloma cells to the bone marrow. Now, this was in a mouse model, not in people, but it also increased the burden of myeloma. Of course, mice and people are very far apart. Nonetheless, I think it does indicate the need for caution and that I wouldn't recommend using metformin, even though it's widely available, simply for the purpose of reducing the risk of progression because we just don't have enough information yet.
Jenny: Patients who might already be taking it who have myeloma, what do you suggest for that?
Dr. Orlowski: Well, definitely, if you're taking it because of diabetes, and especially if you have MGUS or smoldering myeloma, many people with those conditions will never progress. The diabetes may be a greater risk to their health, long-term, than is the plasma cell dyscrasia. I would definitely have no concern about taking the metformin if you have been prescribed it for diabetes purposes.
Jenny: Great.
Dr. Orlowski: There also have been efforts to look at whether other ways of observing myeloma cells, which include testing for circulating tumor cells or doing more detailed biopsies, could be of benefit. I think, in general, what we're finding is that some of these so-called liquid biopsies, which means essentially just studies that are done on the blood, as opposed to the bone marrow, they're getting better. The sensitivity of a blood test is still not as good as a bone marrow. The reason is that there are not many circulating abnormal cells in patients with myeloma or smoldering disease or MGUS. If you have fewer cells than, for example, if you do a bone marrow, you wind up having fewer numbers of cells to study, and you need a larger volume to take in order to do an accurate analysis.
There are studies that show that the circulating cells do increase as people go from MGUS to smoldering myeloma to full myeloma, and others that show that the molecular changes that can be found in the bone marrow are similar to those that can be found in the plasma cells in the circulation. I don't think this is quite ready for prime time, but I do hope that in the near future, we may be able to do away with the need for bone marrows, either completely or at least in the short run, maybe reduce the number of them and replace some of them with these blood assays. I'll turn it over to you, Jenny, to see where you want to go from here.
Jenny: I think that's great. I know patients are always hopeful about that, but just the reality of the number of cells, I don't know, maybe they'll get there in a few years. I appreciate what you said. I think it'd be interesting to understand, talk about progression. You mentioned this a little bit. When you're trying to risk-stratify patients with MGUS and smoldering myeloma, I know you're looking at genetics. We know that some of the smoldering myeloma genetics might be there already when they're diagnosed with smoldering that maybe not new ones are being acquired when they have active myeloma. What's the latest on smoldering myeloma? How do you best risk-stratify your patients, by genetics or tumor burden, or what other factors that you're looking at. Patients always are asking that question. When do I start treatment? Or what do I do and when do I do it?
Dr. Orlowski: Yes, great question. First of all, in terms of prognostic models, probably the one that is used most commonly these days is the International Myeloma Working Group or IMWG model. In the paper, there were actually three different versions; one where they used only three factors, a second one where they added the use of FISH data, which is a molecular test looking for chromosome abnormalities, and then a third model where they had a different number of factors.
I think that one of those IMWG models, which are also known by the 20-2-20 terminology because the initial three factors were more than 20% bone marrow involvement, a monoclonal protein of more than two grams, and an involved to uninvolved free light chain ratio of over 20; one of those three models is the best. They do provide a risk at two years of progression. Now, of course, this is an estimate. The fact that you are high risk doesn't mean that you will progress. Or if you come into the low-risk category, it doesn't mean that you won't progress. The groups do definitely have a different risk profile. There probably will be other versions of these prognostic systems as we get smarter, because right now, we still can't predict large groups versus individuals well.
We can tell you, if you have 500 people in a certain risk group, what percentage of them will progress, but we don't know whether Mr. Smith or Mrs. Jones are going to be the ones that progress. I do think that the technology is getting better. If you are in the high-risk smoldering category, then I think you definitely should think about either a clinical trial, or if one isn't available locally, talk to your myeloma specialist about whether some kind of treatment, this could be with lenalidomide alone, or it could be with lenalidomide and dexamethasone or with daratumumab, if that may be appropriate. If you're in the intermediate or low risk category, you're probably okay, and I don't think you urgently would need treatment.
It also depends on what's happening. Because if you do the risk just at diagnosis, what you are missing out on is the fact that myeloma can change over time, and I would repeat that risk calculation at each visit. There are some studies already that show that if you, for example, are intermediate risk, and you stay at intermediate risk on later visits, your risk of progression will be lower than if you are intermediate at the beginning but then at some point later on, you go to high risk, that suggests what we sometimes call myeloma in evolution. Your M protein is going up, or your free light chains are going up. Those are more concerning situations than if you have stable numbers.
Jenny: Yes, so interesting. That leads us to, when you talk about the ultra-high-risk patients or high-risk smoldering myeloma patients, there are a lot of different types of clinical trials that are out there for those types of patients. Some are like, let's give it all we’ve got, like Kyprolis and Revlimid-dex, plus a transplant, plus double maintenance or some other types of -- do you want to explain the different types of approaches and then what you suggest for patients who are in this category, what they consider?
Dr. Orlowski: Well, as you're pointing out, there are different approaches where some smoldering myeloma, the same as newly diagnosed symptomatic myeloma, and they want to throw, if you will, the proverbial kitchen sink at it. The rationale there is that if you're able to tolerate that therapy, maybe because you're getting it at a time when there is less myeloma to start, and your immune system may be healthier, that there could be an opportunity for cure. Other people look at it from the perspective that they don't feel that the chemotherapy will yet be curative. Rather than give people something very toxic that puts them at risk of complications and also may induce resistance later on, if they do progress, and then the remaining treatment options are going to be less attractive; their rationale is to do maybe less severe or intense treatment.
At MD Anderson, we have a pretty wide program with a number of clinical trials. Our focus has been on immune therapy, and part of that is with the rationale again, that if we utilize a stronger immune system, which people do have in smoldering versus active myeloma, that there is a greater chance of inducing a durable benefit. If we understand the immune mechanisms by which progression occurs, we'll be in a better situation on an individual patient basis to predict what treatment will be best for that one patient. That's what our program is looking to do.
Jenny: I want to just make a comment here, because I think it's really important for myeloma patients not only to see and consult with myeloma specialists, the fact that you have many studies, tens of dozens of studies running at your center for different types of patients. Sometimes that depends on the center’s expertise and the center’s size and the number of patients being treated for that particular type of cancer. It's very important that patients, especially high-risk smoldering myeloma patients are treated in a clinical trial. If that is the case, you need to be by a center or visit a center that has a clinical trial open. Those could be considered at every stage of your disease, from smoldering myeloma to newly diagnosed myeloma to relapsed myeloma. So, just be aware as you consider these treatment options and have these discussions with your doctor, that you consider clinical trials at every stage. I just think that's a really important concept.
Dr. Orlowski: Well, I think you made a great point. The other thing I would say is, don't be bashful about even getting not just a second, but potentially a third opinion, or more, because as you point out, different centers have different expertise. There may be a trial available at a third or fourth center that piques your interest more so than at the second. You would shop around if you were buying an appliance for your house, and this decision is a lot more important than that. Plus, in the smoldering category, you don't have to rush off and immediately begin therapy. You have a little bit of time to consider the options. I know that when people are diagnosed, of course, they're very anxious, and everybody wants to get started on something as quickly as possible. With smoldering disease, you typically have at least a few weeks or a couple of months to look around, do some thinking. This isn't something that just arose in the past six months. You've probably had this for a few years, so another couple of weeks or months to be comfortable that you're going down the right path is a very reasonable thing to do.
Jenny: Yes, I think it's great. You mentioned you have a vaccine study running, I know for smoldering. I'm sure you have others that you're talking about, using immunotherapies. I also thought it was interesting that some of the ASH papers were even thinking about using daratumumab for MGUS patients, or venetoclax, which is not really approved yet in myeloma, for smoldering myeloma patients with the 11;14 translocation. Do you have any comments about those types of approaches?
Dr. Orlowski: Well, I think they're certainly very interesting. We have data already about daratumumab in smoldering myeloma, both alone and in combination, and the data looked good. To me, for MGUS where you have an average risk of progression of 1% per year, and that means that if you're going to treat everybody with MGUS, you will have treated 99 people unnecessarily in order to potentially benefit one person, I think we have to get a little bit smarter to be able to figure out which one person out of those 100 is going to progress and treat that one. To me, I don't think I'm ready yet to say daratumumab for every MGUS patient, or venetoclax for every MGUS patient with t(11;14) because these are drugs that have fewer side effects than many of our older drugs like doxorubicin or cyclophosphamide, but fewer side effects doesn't mean no side effects. Until we know that they have an acceptable risk-benefit ratio, I don't think I'm ready to do it for MGUS.
Now, smoldering, I think, is another story. Remember, the MGUS patients, for example, with COVID, doing relatively well. If we start throwing dara and venetoclax and other things at them, they're going to start having, what I call immune toxicity, which means a weakening of the immune system. Even if you reduce the myeloma burden, which many of these treatments probably would do, if you wind up putting folks at risk for other things, you may not wind up doing them a favor in the long run.
Jenny: That makes a lot of sense. That's a good point. Thank you for pointing that out. Well, maybe we jump to newly diagnosed myeloma. I know there's a lot probably that we want to talk about. What do you consider to be the most promising? You have this induction therapy usually, and a lot of people will go to transplant. Are there other things that you think are promising to change up that protocol, basically, for newly diagnosed patients?
Dr. Orlowski: Well, I think there are a few really interesting things that are happening. Number one, I think that there's a greater awareness that we need to consider things like fitness and frailty in our decisions on treatment for myeloma. Now, frailty is one of those concepts that if you go back to the Potter Stewart comment where he was referring to obscenity, and this was a Supreme Court justice, he said famously at one point that he didn't know how to define it, but he knew it when he saw it. With frailty in patients, I think doctors feel the same way. They know when a patient is frail, but they don't know how to define it. The problem with that is that then different trials may include different numbers of patients with frailty. If I define it one way, and another doctor defines it another way, that's not good. There are now established algorithms that allow us to calculate this. There are still quite a few different ones, and we don't know which one is best.
One, for example, counts that if you're over 80, that automatically puts you into the frail category, which obviously isn't the case for every 80-year-old, so I do think that some refinements are important. We do know that frail patients have to be treated differently than folks that are fitter, and this is one good way that we'll be able to make sure that we're doing that correctly. There also is a greater, I think, understanding that high risk and especially so-called ultra-high-risk patients need to be treated probably more aggressively. One of the ways to define ultra-high-risk is that these are people who have at least two of the high-risk abnormalities in their myeloma cells. Unfortunately, two is worse outcome than one in most situations, and there are a number of approaches here which include trying to use more drugs, intensifying with transplant and using a better consolidation and maintenance therapy.
Actually, we just recently published results of one of those SWOG studies for high-risk patients, where we looked at incorporating an antibody. One thing that we did find is that using a proteasome inhibitor and an immunomodulatory drug as part of both the initial therapy, as well as in maintenance, gave us better outcomes than we would have ever expected in this group. Definitely, intensive therapy and continuing that as long as is feasible, while hopefully not harming the patient too much and maintaining their quality of life, is important for high risk. There also is an area where CAR T-cells and bispecifics are being looked at, because we know the greater the reduction in myeloma, the better will be the outcome for all, but especially for these high-risk folks.
Jenny: Yes, interesting. I saw a lot also at ASH about, like you mentioned the study that you were doing with the antibodies using isatuximab or daratumumab upfront. Instead of just giving like Revlimid-Velcade-dex, they're adding those to the first line of therapy, hoping to move things out. Do you want to comment on what they've seen so far in doing that?
Dr. Orlowski: Well, we do see good benefits in adding an anti-CD38 antibody, and the two that we have so far are daratumumab and isatuximab, as you mentioned. In the randomized studies that we have available in newly diagnosed patients, it does look like one or the other of those drugs is improving outcomes in standard as well as in high-risk disease. There's a little bit of controversy about the high-risk aspect. Part of the problem there is that high risk patients are a subpopulation. There are fewer of them, and when you have fewer patients, it's more difficult to be confident of your conclusion. To me, any drug that further reduces the amount of myeloma is going to be a benefit for high risk. I have switched to using a CD38 antibody in all of my newly diagnosed high risk patients because the further I can mash that myeloma down, the better.
Jenny: Yes, that makes a lot of sense. Well, let's talk about transplant also, maybe just approaches for transplant-eligible versus people who cannot have a transplant. Do you want to just discuss transplant for newly diagnosed patients? Is that something that you are going to say you should probably always do, or wait, or what do you think?
Dr. Orlowski: I think here a lot depends on your risk, again, we're getting back to the standard risk or high risk, and also how well you have done with your initial therapy. I'll tell you the way that I practice in patients that are off of trials. If you fall into the molecularly high-risk category, then I do think that a transplant is reasonable as part of the frontline therapy. In Europe, they would often say that even a tandem transplant or two transplants might be the better way to go. I don't think we need that because we have better upfront drugs available here, but it is something to keep in the back of your mind.
For standard risk patients, what I do is I tell them that if we can get you into a complete remission and MRD negativity, then I will give you the choice of collecting the stem cells and storing them for later and, in the meantime, go on maintenance; or if you just want to go ahead and get the transplant over with, then that's fine too. Many of them elect to just go on maintenance. Some of them, even 10 years out, I've not had to transplant. The good news is that even if you do need a transplant, your outcome from a delayed transplant is just as good. We know that from a number of modern studies that showed that delaying a transplant from the first line until the first relapse, maintains its efficacy. You're not losing anything there. The benefit also is the high dose melphalan which comes with transplant unfortunately does damage normal cell chromosomes sometimes, and can put the patient at risk of a second cancer. Often those second cancers can be more difficult to treat than the first.
Jenny: Yes, not fun for anyone. Let's go back to what you were talking about just now. You're talking about patients who get to be MRD negative after that first line of therapy, then you hold and say, okay, let's just check and see what you're going to do next, and that may take a long time to have happen. MRD testing or this minimal residual disease testing has become a really big thing, and trying to get also as maybe an endpoint for some of these clinical trials. Should newly diagnosed patients, after their first line of therapy, or I know sometimes you have to have a baseline. When does a newly diagnosed patient, when should they get MRD testing? Right before they get -- well, you have detectable disease, so I don't know if, as you’re diagnosed with an M protein of three or six or something is going to do that for them. How do you do MRD testing for these newly diagnosed patients?
Dr. Orlowski: Well, I'm glad you brought that up because it also depends a little bit on what assay, what tests you're going to use for MRD. There are two main ones. One is called Next Generation Flow cytometry or NGF. This is essentially a way to fingerprint the cells in the bone marrow, and it can tell the difference between a normal plasma cell and a myeloma plasma cell. That test, because you use the same antibodies every time that you use it to fingerprint, you can do that test anytime, even if you've never had an MRD test before.
The other one which is called Next Generation Sequencing or NGS, that you have to have a baseline sample where there are myeloma cells because they essentially sequence the gene from the myeloma cells that is making the abnormal protein. Then they monitor the level of expression of that gene, moving forward. On that assay, you really need a baseline sample or at least a bone marrow when you've got some myeloma around, because if you decide, after you've had five or six cycles of chemotherapy, hey, I want to know if I'm MRD negative by the Next Generation Sequencing, they may not be able to identify whether there is an abnormal sequence or not. A little bit depends on that. I think, for me, if you can get the Next Generation Sequencing done, it seems to be one that could be a little bit more sensitive, and that's usually the way that I would go. If you haven't had a chance to have the MRD testing when you were diagnosed, then it makes sense to do the NGF or Next Generation Flow whenever you want to know the information.
Sometimes the doctors are a little hesitant to get it because we don't yet fully know what to do with the information. For example, if you're MRD negative or if you're slightly MRD positive, we don't yet know what to do in those situations. Minimally, for me, we know that if you're MRD negative, your outcome is going to be better than if you're MRD positive. From a patient perspective, I would want to know that because knowing what your prognosis is gives you more of an opportunity to say, maybe I want to change therapy, or maybe they'll be very happy and not want to change therapy. More information can always be helpful and better than less.
Jenny: Yes, I agree. Sometimes the science catches up with some of the test results that you get. If you don't do it at all, then you can't go back and look at anything, but if you do do it, that might be informative later. I don't know. I always think testing is pretty simple, but sometimes I think, like for patients, I was just talking to another patient today. She was diagnosed in a community oncology setting, and she never even had anything done, no genetic testing and that kind of thing. Sometimes, as a patient, you need to ask about these things and just say, can you do an MRD test? What kind of test is it? Just to ask some of those questions
Dr. Orlowski: Definitely. Fortunately, we see less and less patients referred without that kind of testing being done, so I think the awareness of the need to do the testing is increasing. It still does sometimes show up on records that people have had just a plain bone marrow and no cytogenetics, no FISH, no MRD testing. Sometimes we then have to be in the situation of saying, well, maybe we need to redo the bone marrow and get those pieces of information before we make a decision. For me, if somebody comes in and they have all that done, then I can spare them another bone marrow.
Jenny: Yes, right. Well, those are never fun but sometimes informative. I always ask for conscious sedation.
Dr. Orlowski: Oh, yeah, definitely. There are some people who tolerate them very well, but if I had to have a bone marrow, I would also ask for conscious sedation. Just make sure that you have someone to drive you home from that, in case some of the medication hasn't completely worn off.
Jenny: Yes totally worth it, in my opinion. Okay, let me ask this about the 1q gain in newly diagnosed myeloma. I saw a little bit of information about that at ASH. This 1q gain is just like an extra copy of Chromosome 1, or maybe I'm not saying it right. In other tests like from the CoMMpass study and things, they found, if you had three copies, it wasn't necessarily high risk, but if you have four copies, it was. Maybe there was something else that was discovered that you heard at the last ASH, about this 1q gain feature. Because it's found in quite a few number of patients, right?
Dr. Orlowski: Well, the 1q, you’re right, depending on what tests you do, it can be found in, anywhere from 40 to 60, maybe even 60 is probably a little bit high, but nonetheless, anywhere from 40 to 60% of patients may have this. You can have either an amplification of 1q where you have the same number of chromosomes, but that particular region can be having extra copies, or there can be gain where you've got more than two copies of Chromosome 1. You're right that there are some studies that suggest that four or more copies in particular, can be ultra-high-risk or high-risk, whereas maybe three copies is intermediate risk. It also depends on whether there are any other abnormalities present because 1q often isn't there by itself, but may be present with other abnormalities.
Actually, one of the scientists here at MD Anderson, Simona Colla, she and her team were able to show that one of the genes that can be amplified in the 1q21 region, so meaning that there are extra copies, can actually help to promote repair of DNA damage. While that sounds like a good thing for normal cells, which it is, unfortunately, in myeloma cells, if you're doing, for example, a stem cell transplant where you're using a DNA-damaging drug, by having more DNA damage repair proteins, those myeloma cells have a mechanism of resistance. She and her team are looking at ways to specifically down-regulate that gene.
I think a lot of what has been done now in high-risk disease is really generic therapy. What I mean by that is not that it shouldn't be done, but that it's not really specific for each of the subtypes of high risk. What we probably need to get to and what we're working on here are, understand the biology of each of the subtypes, for example, deletion 17p, 4;14, 14;16, with the notion that a different therapy will be best for each of the individual subtypes. I think that's probably the way to go in the future, along with the immunotherapy approaches which hopefully will work against all of them.
Jenny: Yes, it's hard to think about this targeting idea, but I think that understanding of the biology is so important because then you can group people into different buckets. Do you want to explain any clinical trials that are being run, either at MD Anderson or other places, for newly diagnosed myeloma that patients might want to just have a heads up about?
Dr. Orlowski: Well, definitely, I think that there are a number of studies, which we briefly mentioned earlier, looking at addition of CD38 antibodies. Also, for high risk patients, there are some studies that are taking already CAR T-cells into earlier lines of therapy, and others that are using bispecific antibodies, which we'll probably get to in the next segment. I think the nice part about these trials is that many of them are building onto what we already consider a standard of care. It's not that you're getting some new thing that they've just dusted off the shelf and are giving it to you, you're getting the standard therapy plus something that we think makes it work better. The good news about that is that most of these agents, by the time they're given in the newly diagnosed setting, has already been shown to be very active in relapsed/refractory myeloma. If something works that late in treatment, it usually works even better in the earlier lines of therapy. Many people just want the tried-and-true therapy, and I can certainly understand that. On the other hand, getting your ice cream with some sprinkles on it that makes it taste better is always a good thing. I would say upgrade to first class from coach and go on a trial.
Jenny: I agree because everyone always tells you, your first therapy is your most important and your most durable and longest remission. I don't know. In my opinion, you should just do some homework. That's tough to do as a newly diagnosed myeloma patient because you've been hit with this diagnosis, this disease you probably never heard of before. All of a sudden, you're supposed to make a decision and consider a clinical trial. It's an extra complicated time of your life and making these decisions, but truly, I think it does matter for your outcome, to consider that.
Dr. Orlowski: I just want to say really briefly, the other thing to keep in mind is that some trials in the newly diagnosed setting, do allow you to have one cycle of treatment somewhere else and then to go on the trial because they realize that sometimes people present with kidney problems or high calcium. They need to get treated right away, and they can't wait for a consult, two weeks down the road. Many of the trials will allow you to get one cycle of therapy, usually three or four weeks, and then still go onto the trial later on and benefit from the novel drug that's being used.
Jenny: Oh, I didn't know that. That's great information and additional options for newly diagnosed patients. Okay, wonderful. Well, let's talk about relapsed/refractory myeloma. You had mentioned CAR T being used in newly diagnosed myeloma. Would you like to give an update of that? I know we're all anticipating this other update in the month of February, but maybe just give us a status report of where CAR T is at. I know it's been a challenge to get this therapy into patients.
Dr. Orlowski: Well, we do have one approved CAR T for myeloma which is the anti-BCMA or B cell maturation antigen-targeted therapy called ide-cel. That's the way to abbreviate it. We hope, soon, even in this month, to have a second BCMA-targeted CAR T which will be called cilta-cel. There haven't been head-to-head studies comparing them. They both look really good. Cilta-cel, which is the one that hopefully will be approved this month, may look a little bit better, but again, until you do a randomized study comparing them head-to-head, it's tough to know.
One of the limitations that has come up is that, of course, at least the way these cells are made now, you need actually viral vectors because viruses are used to get the gene into the T cell that expresses the CAR or chimeric antigen receptor. Some of these require quite a lot of virus, and there have been some limitations on production, so that has slowed the roll-out. Of course, we've got COVID problems. That hasn't helped. I, tongue in cheek, say, there's not enough virus of one kind and too much virus of another. Hopefully, in ‘22, as the pandemic hopefully wanes and doesn't come back and more manufacturing capacity comes online, I think more people will be able to benefit from the currently available CAR Ts.
There are other CAR Ts that are being studied as well, including others that also target BCMA. There also are studies against other targets. Because sometimes what can happen is that when you use one therapy against this protein called BCMA, you can get a myeloma relapsing that doesn't express BCMA. It kind of turns into a stealth myeloma cell. It becomes invisible to another therapy against that same target. Fortunately, there are other targets that look really attractive. Probably the best examples are GPRC5D which is another protein that, like BCMA, is expressed a lot on myeloma cells. There's also a target called FcRL5. There are others that are being explored, including a couple that we're looking at, at MD Anderson.
The hope is that if you get a BCMA-targeted therapy, if you relapse, what we would do is we would study your myeloma cells. If they still make BCMA, then we could maybe give you the same thing again or a slightly different BCMA-targeted therapy. Whereas, if you relapse and you don't have BCMA, hopefully your myeloma cells would have one of these other protein targets, and we could come back with a slightly modified CAR T or a modified bispecific therapy.
Jenny: Yes, okay, interesting, lots of different approaches. That ide-cel is also called Abecma, for people who might know that name and not the other one. Let’s talk about bispecific antibodies because there seems to be so many being developed in the myeloma space, both for BCMA and other targets. Do you want to do a review of those?
Dr. Orlowski: Sure. Well, with a CAR T-cell, the way most of the products now, not all, but the way most of them are made is that your T cells are taken out, they're infected with this virus that brings in the receptor gene into the cell, the T cells are expanded, and then they are sent back and infused into you. That process can take four to maybe five or even six weeks. In the meantime, you're waiting. Sometimes you need what's called Bridging therapy, which means treatment to knock the myeloma down a little bit while you're waiting for the CAR T. Also, each patient's cells can only be used for them and not somebody else.
The idea behind a bispecific is this is an antibody, so it's sort of like daratumumab or isatuximab, except that you have two arms, if you will. That's why it's called a bispecific. One arm binds, in this case, to myeloma, or you can make it to a different tumor; and the other arm binds to your own T-cell in your body. It activates the T-cell, brings it next to the myeloma cell, and the T-cell attacks. This is what we call an off-the-shelf therapy because the same drug is used for multiple people. You take one vial and give it to Mrs. Smith and another one goes to Mr. Jones, so you don't have that four to six-week wait period. The efficacy of these seems to be good. As you mentioned, there's many of them that are being trialed. They have response rates, usually 60 to 70, or even 80% range.
The only downside is that right now, the treatment is given on a regular basis. With the CAR T, you get one infusion of these cells and then, for right now, at least, you don't get any more therapy. With the bispecifics, typically, you get either an infusion or injection. Some of them start weekly, some of them start a little bit more frequently, some of them start less frequently, but it is an ongoing therapy. Again, it's more like daratumumab where, once you start, you tend to continue; same thing with lenalidomide, for example. There are pros and cons to both approaches. I think if you're in the relapsed or refractory setting, just talk to your myeloma specialist about which of those may be best for you.
Jenny: Yes, and those are all in clinical trials right now. Again, a reason to get up-to-date on what's happening in clinical trials because these might be options. Okay, we still have more to cover, but I also want to leave time for caller questions. Do you want to give us an update on using other drugs like selinexor and Blenrep and then newer things that are not approved yet in the relapsed/refractory setting?
Dr. Orlowski: Definitely. Well, just really quickly so we have a few minutes for questions. We have a new generation of what are called cereblon-binding drugs that are coming, or CELMoDs. These are similar in some ways to lenalidomide and pomalidomide, but they seem to work even in patients whose myeloma no longer responds to len or pom. Some of those are hopefully getting close to approval. The data that have been presented look good. You mentioned selinexor which is a selective inhibitor of nuclear export, which either alone or preferably with dexamethasone, or even with other drugs like bortezomib, or Carfilzomib or Dara, can be very helpful and if given once a week at the right dose and with supportive care can be very good.
You mentioned belantamab mafodotin, and I'm using the generic name because that's what we're trained to do in academia, which is an antibody drug conjugate to BCMA. Especially with some of the newer dosing regimens where it's given maybe once every month or even once every six weeks, you can have very good activity, both alone and in combination. This is one of those things that also is off the shelf, so you don't have to worry about waiting for weeks and weeks to get your treatment. I think those are some of the things that are coming.
We also have other CD38 antibodies. There's one that I thought was interesting from the ASH meeting, which was TAK-573. It doesn't yet have an official name, but this was a CD38 antibody with an attached interferon molecule. Some of you who've been around myeloma for a long time, may remember that interferon used to be used in myeloma. I think the interesting thing about this drug is that even though it goes after CD38, it showed activity even in people whose myeloma was progressing on daratumumab. There may be, I think, good applicability of that drug if the data continue to look as attractive.
The bottom line is there's lots of things available. There's even other therapies that are going to be available if people need them, so really make sure that you get the best treatment upfront. I think part of the rationale for many years has been that, well, don't use everything that we have because then when you relapse, there's going to be nothing left. I can guarantee you that as active as the field is, even if you use up everything that's FDA-approved now, by the time you get to that point, there will be other therapies available. The sooner you use something, the better is the benefit.
Jenny: I think that's great advice. Okay, that's amazing. You went through a lot of information, but I do want to go to caller questions, so thank you so much. If you have a question for Dr. Orlowski, you can call 347-637-2631 and then press “1” on your keypad. We'll start with caller one. Go ahead with your question.
Caller: Hi, Jenny. It’s Jack. Hello, Dr. Orlowski. I always enjoy your show.
Jenny: Hi, Jack.
Dr. Orlowski: Hey, Jack.
Caller: Hi there. I enjoyed your discussion on MRD testing. We have patients though that, as Jenny mentioned, for example, never got or don't have available a bone marrow sample from their initial diagnosis. Is it reasonable, if you want NGS sequencing testing, to start a new basis, whenever you relapse, if you don't have that initial basis?
Dr. Orlowski: First of all, sometimes when you have your initial bone marrow, pathologists may have extra slides or what they call coverslips, that haven't yet been used or stained. Sometimes you can extract enough DNA from those that you can get the sequencing done from the baseline. Yes, if you relapse and you have measurable myeloma now, you can get the NGS as a baseline at that time, even if you didn't have it done at the time of initial diagnosis.
The only time that doesn't work is if you didn't have it at baseline, you get treated with something, and you're in complete remission, and you want to know if you're MRD negative. You may not be able to tell that from the sequencing because there's not enough myeloma cells to evaluate, which in some ways is a good thing because if you've got a lot of myeloma cells left, then that's not good result. Yeah, you can definitely do it at the time of relapse if you haven't had one at baseline.
Caller: Thank you.
Jenny: Yes, great question.
Dr. Orlowski: Thank you.
Jenny: Thanks, Jack. I think a lot of patients wonder about that. Okay, next caller, go ahead with your question.
Caller: Hi, Dr. Orlowski. Thanks for your time today. I've learned a lot. This has been really informative. I had a specific question. You mentioned deletion 17p. I'm wondering, can you give us an update on your work on that, as I understand that you're doing specific work on that mutation?
Dr. Orlowski: Yes, thank you for asking that. We, hopefully, will be publishing this soon. We've presented at ASH, data about one specific drug which is a BCMA antibody drug conjugate. It turns out that when you have deletion 17p, although p53 is the gene whose loss is probably most impactful in terms of poor prognosis, there is a very nearby gene called POLR2A which is also lost. The only good thing about that is that it makes the cells super sensitive to a drug called amanitin, which is a poison from mushrooms, but if we attach that drug to an antibody, we can get it safely into myeloma cells, at least in mice, which of course, we've been able to cure mice for a while with myeloma. That's not new, but we do see very good responses.
We're about to start a trial of that in relapsed/refractory myeloma patients of that antibody. I think the data are, at least in the laboratory, really exciting. If we could get similar results in patients, fingers crossed, we would have a therapy that would work well for all myeloma patients, but would work especially well for deletion 17p. Unfortunately, right now, it's the opposite. Things do work in deletion 17p, but usually the benefit is shorter. Here, what we have is, hopefully, something where the benefit will be longer.
Jenny: Yes, well, these patients need extra help. Great question, and I'm so glad you're working on this. Okay, next caller, go ahead with your question.
Caller: Hello. I appreciate your speaking with us today. It has been very interesting.
Dr. Orlowski: My pleasure.
Caller: My interest in particular is you had some clinical trials with people with myeloma or with pancreatic cancer and trying to deal with the NRAS, KRAS mutation. Could you perhaps update us on the status of that effort?
Dr. Orlwoski: You're bringing up a good point, which is that about maybe 20% of myeloma patients will have an NRAS mutation, and about another 20% of patients will have a KRAS mutation. Usually, you have one or the other, not both. Some of the positions of the mutation in the gene where they occur in myeloma are a little bit different than the ones that occur in pancreatic cancer. We know that in myeloma, when you have this mutation, it activates one particular pathway called the p44/42 MAPK, and there are drugs that have been tried in patients with those mutations that block that pathway that seemed to show good activity. There are some molecularly targeted therapies of trials where you can access those drugs, and some of them are also FDA-approved. I would definitely look into that. Although it seems that those patients also respond well to immunotherapies, but you're right that we do need more trials targeting that particular group of patients.
Caller: Excellent, excellent. Who would I contact at MD Anderson to learn more about specific treatments available?
Dr. Orlowski: Actually, I usually give out my email address on this call, so now is as good a time as any to do that. It’s rorlowski@mdanderson.org. I'll do the best I can to send you a reply within about 24 hours. It depends on how much digging I have to do to get the answer.
Caller: Oh, that's wonderful. That's great news.
Jenny: Okay, great. Yeah, great question, and thanks for your answer. Okay, we'll have one more caller question. Go ahead with your question.
Caller: Yes. Dr. Orlowski, my husband right now has unquantifiable, whatever that means. Now, at what point could he have another bone marrow? If the M protein is at 0.2 or 0.5 or higher?
Dr. Orlowski: Now when you say another bone marrow, are you referring to a biopsy or to a stem cell transplant?
Caller: Oh, a biopsy so that he could have full genetics or whatever you all do to get that done.
Dr. Orlowski: Well, anytime there is a measurable protein in the blood suggests that there is also myeloma in the bone marrow. The more protein, in general, the more myeloma cells, and the more myeloma cells, the easier it is to do the genetic testing. Many places will now take the bone marrow aspirate and do a purification step to concentrate the myeloma cells. I would say that if his numbers are creeping up, I wouldn't wait until it hits a predetermined level. I would just go ahead and get an evaluation and try to do the bone marrow and figure out what's going on. Because myeloma sometimes, when it relapses, will creep along slowly, and you've got time; but every now and then, it creeps along for a while, and then all of a sudden, something happens and it takes off very rapidly. We wouldn't want him to have a bad outcome because of that. I would say the sooner you can get evaluated, the better. Don't wait for a particular number.
Caller: Okay, he has an M protein that's unquantifiable. Can he have one done now that would be significant?
Dr. Orlowski: I'm sorry. Thank you for reminding me about that. The unquantifiable usually means that the protein is visible on what's called the immunofixation but not on the electrophoresis. That doesn't mean that it would be at a low level. Do you have any information from the baseline testing about the type of myeloma that he had?
Caller: Well, he has light chain.
Dr. Orlowski: Okay. Yeah, I think if you have just proteins visible by the immunofixation, what I would definitely do is talk to your doctor there who will be doing the bone marrow and find out if they will be purifying the myeloma cells before testing them for any chromosome changes. Because if they're not purifying and concentrating the cells, there may not be enough of them when he's in this very low disease state to get a good reading on the chromosomes. The problem is that you can be kind of fooled because if there's only a few myeloma cells in there, you may get back a negative result. You may think, oh, that's good because he doesn't have high risk features, but it may turn out that that's true only because there weren't enough myeloma cells to test.
Caller: I would be going back to your facility.
Dr. Orlowski: Oh, well, no problem then.
Jenny: Great. Thank you so much.
Caller: By the way --
Jenny: Sorry, just one second. Let me bring her back on. Go ahead. Sorry.
Caller: I was born in Poland and was a refugee during WWII.
Dr. Orlowski: Oh, (answers in Polish). A little Polish story, everybody.
Caller: Okay, thank you. Dr. Orlowski, thank you so much. What an informative show. We had so much to cover, and I just think you're the best at doing this. I just appreciate what you're doing and the research you're providing for patients, and the excellent care. Thank you so much for participating once again on this annual show. We just appreciate you.
Dr. Orlowski: Thank you everybody. Bye-bye.
Jenny: Okay, thank you so much. Thank you for listening to Myeloma Crowd Radio. We invite you to join us next time to learn about what's happening in myeloma research and what it means for you.
Trending Articles
Upcoming Events
Have Any Questions?
Thank you for your interest in the event. If you have any questions, we would love to help!
Feel free to give us a call or send us a message below.

Get In Touch With Us
1-800-709-1113
Support@healthtree.org
More Podcast Episodes
Get the Latest Multiple Myeloma Updates, Delivered to You.
By subscribing to the HealthTree newsletter, you'll receive the latest research, treatment updates, and expert insights to help you navigate your health.
Together we care.
Together we cure.