The Role of Transplant in Myelofibrosis

Myelofibrosis is a condition that affects the bone marrow’s ability to produce new blood cells due to scar tissue occupying the bone marrow. There are multiple causes of this condition; some are primary, meaning that the issue originates internally from mutations in the bone marrow cells, and some are secondary, which occurs when there is an external cause like chemotherapy, other cancers, or lesions that affect and damage bone marrow cells.
Myelofibrosis is generally considered an incurable disease. The only possibility of a cure is undergoing a bone marrow transplant, and not all patients can receive this treatment due to different causes, such as advanced age or health conditions like heart, lung, or kidney disease. However, the ways to treat this condition beyond stem cell transplant are continuously expanding.
Bone Marrow Transplant for Myelofibrosis: Who is Eligible?
When it comes to deciding who should receive a transplant, several factors need to be taken into consideration. A doctor must assess three main factors: patient factors, transplant factors, and disease-specific factors. Since every patient is unique, there may be some exceptions to the rules if it means that the patient will have a better outcome. For example, it might be offered to patients with poor survival based on prognostic scores like IPSS or DIPSS to increase their chances of getting better.
Additionally, the risk of developing leukemia and the risk of not responding well to chemotherapy can influence the decision to transplant. This risk is assessed by the genetic mutations analyzed in a bone marrow biopsy, the blood cell counts, and the symptoms that a patient is experiencing.
Bone marrow transplant is a powerful treatment for myelofibrosis, but it's also a complex procedure with potential risks, some of them listed in the picture below. Carefully weighing the potential benefits of a cure against the risks of transplantation is crucial. If a patient doesn’t have the opportunity to receive a transplant, enrolling in a clinical trial or receiving pharmacological therapy, for example, JAK inhibitors, can also result in significant disease control and health improvement.
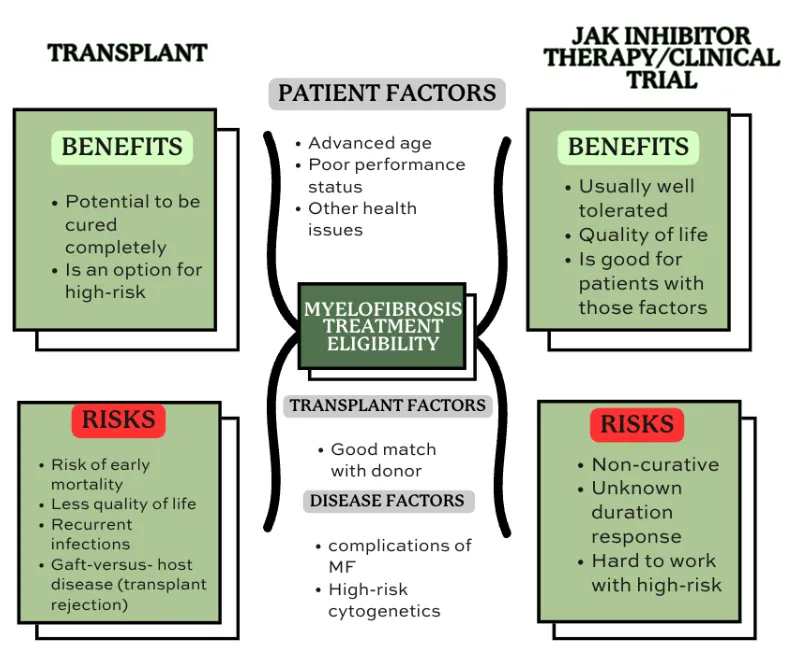
Figure adapted from: Devlin, R., & Gupta, V. (2016). Myelofibrosis: to transplant or not to transplant? Hematology, 2016(1), 543–551.
How a Transplant Can Cure Myelofibrosis?
The goal of treating myelofibrosis is to make the bone marrow functional again since scar tissue impedes bone marrow cells from forming blood cells. The highest odds of achieving this are undergoing a stem cell transplantation. This process is challenging for patients and the medical team, who have to monitor them closely.
The process consists of destroying the compromised bone marrow with high doses of chemotherapy injected intravenously for a short period. This process is called conditioning and creates a clean canvas to place the new healthy stem cells. Then, a donor, who needs to be genetically similar to the patient receiving the transplant, will give stem cells, which are immature cells inside the bone marrow that have the ability to produce blood cells. Once the patient’s bone marrow is “empty,” healthy stem cells will be introduced by intravenous infusion, traveling from the bloodstream to the bone marrow.
When the new cells are obtained from a different individual, this is called allogeneic stem cell transplantation. When treating other blood cancers, this process can be done with the patient’s stem cells, and then it’s called autologous stem cell transplantation.
Recovering from an allogeneic stem cell transplant is a long process that can take months of close monitoring. Usually, patients will stay in the hospital for 3 to 4 weeks until the new bone marrow starts producing new blood cells again. During this time, it’s common to receive transfusions when needed until the healthy stem cells settle in the new body. During this period, the immune system will be weaker, and the medical team will act to prevent all sorts of risks of infections.
How Do I Know If I Can Benefit From A Transplant?
When your oncologist assesses your overall health, they evaluate whether you may be a candidate for transplant by looking for all the conditions and personal aspects that can complicate the healing process. These can range from your age, cardiovascular conditions, metabolic issues, or a low platelet count to high-risk genetic features.
If any of these conditions apply to you, don’t get discouraged. The only ones who can tell you if you qualify are the doctors on your team. They complete a 360-assessment of your health profile and give you the best option. Remember that each patient is different and that many alternatives beyond transplant can be a better fit for you.
A great option to consider is to find a transplant expert to assess your situation fully; some excluding factors mentioned may not apply to you as the treatment needs to be adjusted individually and considering every patient’s specific needs. Receiving a second opinion from a transplant expert is beneficial to understanding all your options and how to achieve the best possible response.
In conclusion, understanding myelofibrosis is crucial for patients and their healthcare teams. Whether exploring treatment options like stem cell transplants or managing symptoms and disease progression, each patient's journey is unique. Remember, qualified medical professionals are best equipped to assess individual eligibility and provide tailored guidance.
If you want to continue reading about myelofibrosis, you can check our 101 articles, like:
Myelofibrosis is a condition that affects the bone marrow’s ability to produce new blood cells due to scar tissue occupying the bone marrow. There are multiple causes of this condition; some are primary, meaning that the issue originates internally from mutations in the bone marrow cells, and some are secondary, which occurs when there is an external cause like chemotherapy, other cancers, or lesions that affect and damage bone marrow cells.
Myelofibrosis is generally considered an incurable disease. The only possibility of a cure is undergoing a bone marrow transplant, and not all patients can receive this treatment due to different causes, such as advanced age or health conditions like heart, lung, or kidney disease. However, the ways to treat this condition beyond stem cell transplant are continuously expanding.
Bone Marrow Transplant for Myelofibrosis: Who is Eligible?
When it comes to deciding who should receive a transplant, several factors need to be taken into consideration. A doctor must assess three main factors: patient factors, transplant factors, and disease-specific factors. Since every patient is unique, there may be some exceptions to the rules if it means that the patient will have a better outcome. For example, it might be offered to patients with poor survival based on prognostic scores like IPSS or DIPSS to increase their chances of getting better.
Additionally, the risk of developing leukemia and the risk of not responding well to chemotherapy can influence the decision to transplant. This risk is assessed by the genetic mutations analyzed in a bone marrow biopsy, the blood cell counts, and the symptoms that a patient is experiencing.
Bone marrow transplant is a powerful treatment for myelofibrosis, but it's also a complex procedure with potential risks, some of them listed in the picture below. Carefully weighing the potential benefits of a cure against the risks of transplantation is crucial. If a patient doesn’t have the opportunity to receive a transplant, enrolling in a clinical trial or receiving pharmacological therapy, for example, JAK inhibitors, can also result in significant disease control and health improvement.
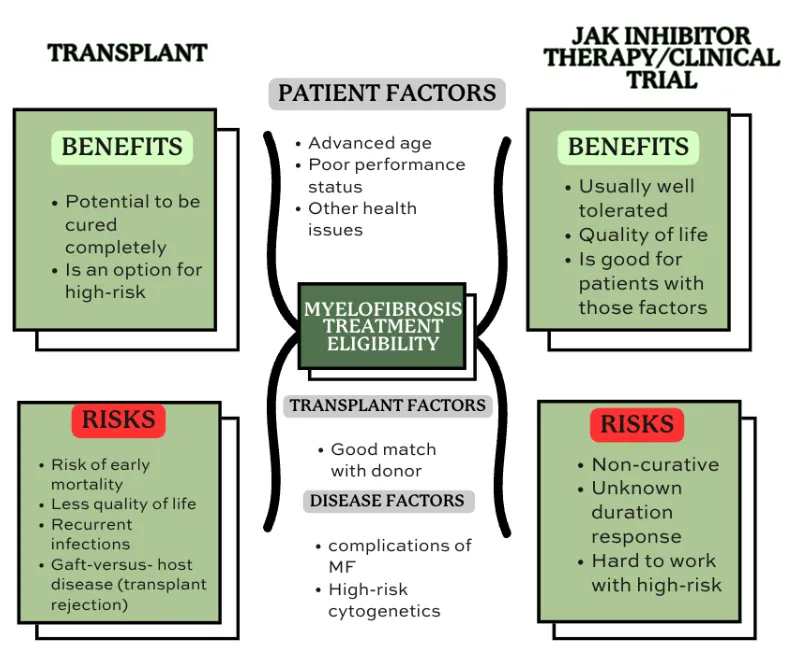
Figure adapted from: Devlin, R., & Gupta, V. (2016). Myelofibrosis: to transplant or not to transplant? Hematology, 2016(1), 543–551.
How a Transplant Can Cure Myelofibrosis?
The goal of treating myelofibrosis is to make the bone marrow functional again since scar tissue impedes bone marrow cells from forming blood cells. The highest odds of achieving this are undergoing a stem cell transplantation. This process is challenging for patients and the medical team, who have to monitor them closely.
The process consists of destroying the compromised bone marrow with high doses of chemotherapy injected intravenously for a short period. This process is called conditioning and creates a clean canvas to place the new healthy stem cells. Then, a donor, who needs to be genetically similar to the patient receiving the transplant, will give stem cells, which are immature cells inside the bone marrow that have the ability to produce blood cells. Once the patient’s bone marrow is “empty,” healthy stem cells will be introduced by intravenous infusion, traveling from the bloodstream to the bone marrow.
When the new cells are obtained from a different individual, this is called allogeneic stem cell transplantation. When treating other blood cancers, this process can be done with the patient’s stem cells, and then it’s called autologous stem cell transplantation.
Recovering from an allogeneic stem cell transplant is a long process that can take months of close monitoring. Usually, patients will stay in the hospital for 3 to 4 weeks until the new bone marrow starts producing new blood cells again. During this time, it’s common to receive transfusions when needed until the healthy stem cells settle in the new body. During this period, the immune system will be weaker, and the medical team will act to prevent all sorts of risks of infections.
How Do I Know If I Can Benefit From A Transplant?
When your oncologist assesses your overall health, they evaluate whether you may be a candidate for transplant by looking for all the conditions and personal aspects that can complicate the healing process. These can range from your age, cardiovascular conditions, metabolic issues, or a low platelet count to high-risk genetic features.
If any of these conditions apply to you, don’t get discouraged. The only ones who can tell you if you qualify are the doctors on your team. They complete a 360-assessment of your health profile and give you the best option. Remember that each patient is different and that many alternatives beyond transplant can be a better fit for you.
A great option to consider is to find a transplant expert to assess your situation fully; some excluding factors mentioned may not apply to you as the treatment needs to be adjusted individually and considering every patient’s specific needs. Receiving a second opinion from a transplant expert is beneficial to understanding all your options and how to achieve the best possible response.
In conclusion, understanding myelofibrosis is crucial for patients and their healthcare teams. Whether exploring treatment options like stem cell transplants or managing symptoms and disease progression, each patient's journey is unique. Remember, qualified medical professionals are best equipped to assess individual eligibility and provide tailored guidance.
If you want to continue reading about myelofibrosis, you can check our 101 articles, like:

about the author
Jimena Vicencio
Jimena is an International Medical Graduate and a member of the HealthTree Writing team. She has a passion for languages and is currently learning Japanese. In her free time, she loves playing with her cats. Jimena is also pursuing a bachelor's degree in journalism.
More on Core Education
Trending Articles
Get the Latest Myelofibrosis Updates, Delivered to You.
By subscribing to the HealthTree newsletter, you'll receive the latest research, treatment updates, and expert insights to help you navigate your health.
Together we care.
Together we cure.