What is Early Primary Myelofibrosis?

Myelofibrosis is a type of cancer that affects the bone marrow's ability to generate new blood cells caused by scar tissue within the marrow. This condition is due to various reasons, with primary causes due to mutations within bone marrow cells.
As a result of bone marrow scarring, common symptoms arise including low blood cell counts like anemia (low red blood cell counts), enlarged spleen or enlarged liver which can reduce life expectancy in myelofibrosis patients.
Other symptoms that can negatively impact myelofibrosis patients’ quality of life include fatigue, stomach discomfort, night sweats, bone pain, and itching.
What is “Early” Myelofibrosis?
The concept of “early” or prefibrotic primary myelofibrosis comes from changes in the bone marrow that precede fibrosis but have not fully changed to fibrosis.
The WHO classification includes a distinct category for early/prefibrotic primary myelofibrosis (a diagnosis made only after analyzing a biopsy sample).
Patients with myelofibrosis are risk-stratified, often into low, intermediate-1 (int-1), int-2, or high-risk disease.
“Early Myelofibrosis” is a concept that can be defined in two general ways:
- Risk of death (this risk is determinedwith genetics and baseline health at diagnosis)
- Disease duration (how long have these changes taken place in the bone marrow)
How is Early Myelofibrosis Treated?
Since early myelofibrosis refers to changes in the bone marrow that have the potential to progress to bone marrow fibrosis but are not fibrotic yet, the recommendations are to treat them as soon as possible.
Multiple studies have shown that treating myelofibrosis as soon as possible after diagnosis can be beneficial to patients. This results in more effectiveness and lower toxicity compared with treating it later in the disease course.
What are the Treatments for Early/Prefibrotic Primary Myelofibrosis?
Ruxolitinib has shown promising results in patients who start an early treatment when a prefibrotic process in their bone marrow is detected. Some of the findings are very interesting:
- Ruxolitinib can improve patients’ overall survival rate
- Ruxolitinib reduced symptom severity after 4 weeks of treatment, improving quality of life in patients
- After 6 months of treatment, patients had a reduction in the previously enlarged spleen
- Patients experienced better blood cell counts (improved anemia and platelet counts)
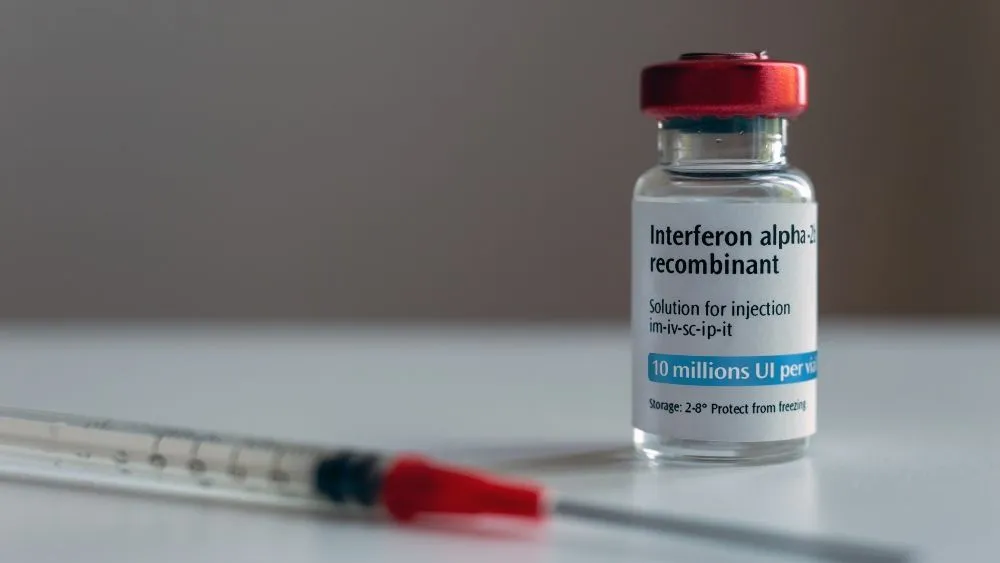
Therapy with Interferon alfa-2a can also be used for myelofibrosis, mainly in patients without enlarged spleen or symptoms, and can reduce bone marrow fibrosis and improve treatment response in patients without high-risk mutations.
Combination treatment with ruxolitinib and interferon alfa-2a is also an option for certain patients with myelofibrosis. The phase 1/2 Ruxopeg study showed that this combination is well tolerated and helped reduce the spleen size and reduce mutational changes.
Myelofibrosis is considered a chronic condition, with the only curative option being a hematopoietic stem cell transplant. Several therapies have been developed and are available to extend the overall survival of myelofibrosis patients, like ruxolitinib, which can also improve symptoms caused by myelofibrosis and extend life expectancy.
Expanding treatment options for all patients and discovering the best time to start treatment is possible thanks to research. This is why it is very important to continue active research on early myelofibrosis patients so that their progression can be prevented one day.
If You Want to Stay Updated With Myelofibrosis Treatment Advances, Join Our Newsletter!
NEWSLETTER
Sources:
- What Is Prefibrotic Myelofibrosis?
- Primary myelofibrosis: 2023 update on diagnosis, risk-stratification, and management
- Management of Patients with Early Myelofibrosis: A Discussion of Best Practices
- Primary Myelofibrosis
Myelofibrosis is a type of cancer that affects the bone marrow's ability to generate new blood cells caused by scar tissue within the marrow. This condition is due to various reasons, with primary causes due to mutations within bone marrow cells.
As a result of bone marrow scarring, common symptoms arise including low blood cell counts like anemia (low red blood cell counts), enlarged spleen or enlarged liver which can reduce life expectancy in myelofibrosis patients.
Other symptoms that can negatively impact myelofibrosis patients’ quality of life include fatigue, stomach discomfort, night sweats, bone pain, and itching.
What is “Early” Myelofibrosis?
The concept of “early” or prefibrotic primary myelofibrosis comes from changes in the bone marrow that precede fibrosis but have not fully changed to fibrosis.
The WHO classification includes a distinct category for early/prefibrotic primary myelofibrosis (a diagnosis made only after analyzing a biopsy sample).
Patients with myelofibrosis are risk-stratified, often into low, intermediate-1 (int-1), int-2, or high-risk disease.
“Early Myelofibrosis” is a concept that can be defined in two general ways:
- Risk of death (this risk is determinedwith genetics and baseline health at diagnosis)
- Disease duration (how long have these changes taken place in the bone marrow)
How is Early Myelofibrosis Treated?
Since early myelofibrosis refers to changes in the bone marrow that have the potential to progress to bone marrow fibrosis but are not fibrotic yet, the recommendations are to treat them as soon as possible.
Multiple studies have shown that treating myelofibrosis as soon as possible after diagnosis can be beneficial to patients. This results in more effectiveness and lower toxicity compared with treating it later in the disease course.
What are the Treatments for Early/Prefibrotic Primary Myelofibrosis?
Ruxolitinib has shown promising results in patients who start an early treatment when a prefibrotic process in their bone marrow is detected. Some of the findings are very interesting:
- Ruxolitinib can improve patients’ overall survival rate
- Ruxolitinib reduced symptom severity after 4 weeks of treatment, improving quality of life in patients
- After 6 months of treatment, patients had a reduction in the previously enlarged spleen
- Patients experienced better blood cell counts (improved anemia and platelet counts)
Therapy with Interferon alfa-2a can also be used for myelofibrosis, mainly in patients without enlarged spleen or symptoms, and can reduce bone marrow fibrosis and improve treatment response in patients without high-risk mutations.
Combination treatment with ruxolitinib and interferon alfa-2a is also an option for certain patients with myelofibrosis. The phase 1/2 Ruxopeg study showed that this combination is well tolerated and helped reduce the spleen size and reduce mutational changes.
Myelofibrosis is considered a chronic condition, with the only curative option being a hematopoietic stem cell transplant. Several therapies have been developed and are available to extend the overall survival of myelofibrosis patients, like ruxolitinib, which can also improve symptoms caused by myelofibrosis and extend life expectancy.
Expanding treatment options for all patients and discovering the best time to start treatment is possible thanks to research. This is why it is very important to continue active research on early myelofibrosis patients so that their progression can be prevented one day.
If You Want to Stay Updated With Myelofibrosis Treatment Advances, Join Our Newsletter!
NEWSLETTER
Sources:
- What Is Prefibrotic Myelofibrosis?
- Primary myelofibrosis: 2023 update on diagnosis, risk-stratification, and management
- Management of Patients with Early Myelofibrosis: A Discussion of Best Practices
- Primary Myelofibrosis

about the author
Jimena Vicencio
Jimena is an International Medical Graduate and a member of the HealthTree Writing team. She has a passion for languages and is currently learning Japanese. In her free time, she loves playing with her cats. Jimena is also pursuing a bachelor's degree in journalism.
More on Treatment Advances
Get the Latest Myeloproliferative Neoplasm Updates, Delivered to You.
By subscribing to the HealthTree newsletter, you'll receive the latest research, treatment updates, and expert insights to help you navigate your health.