What Factors Impact the Outcomes in Myelofibrosis Patients?

Myelofibrosis (MF) is a type of blood cancer that affects the bone marrow, leading to abnormal production of blood cells. Over time, scar tissue forms in the bone marrow, reducing its ability to make healthy blood cells. This can cause a wide range of symptoms, including fatigue, an enlarged spleen, and difficulty fighting infections. Myelofibrosis can develop on its own (primary MF) or as a progression from other conditions like polycythemia vera (PV) or essential thrombocythemia (ET).
While each case is unique, several important factors have been shown to impact how myelofibrosis develops and how patients respond to treatment.
If you've been diagnosed with myelofibrosis, you may have wondered what factors can potentially influence your health, disease progression, and outcomes. Understanding these factors can help you feel more informed and engaged in managing your health.
Recent Data for Myelofibrosis Risk Factors
A recent retrospective study published in the Annals of Hematology evaluated data from two sources:
-
The SEER database (2000-2021), 5,403 myelofibrosis patientsMontefiore Medical Center (2000-2023),, 84 cases.
The study examines how social and demographic factors impact survival in myelofibrosis, a rarely studied topic.
It shows that social and demographic factors, including sex, race, marital status, and income, are associated with survival in myelofibrosis. Addressing these social and demographic factors is key to improving overall health outcomes and providing fair care for all myelofibrosis patients.
What are the Main Findings from SEER Data?
The SEER database analysis (2000-2021) included 5,403 myelofibrosis patients, with a median age of 69 years. The majority (82%) were non-Hispanic White.
-
Survival Rates:
-
2-year survival: 69%
-
5-year survival: 42%
-
Factors Linked to Worse Survival:
-
Older age
-
Male sex
-
Diagnosis before 2011 (prior to ruxolitinib approval)
-
Predictors of Worse Overall Survival:
-
Non-Hispanic Black ethnicity
-
Unmarried status
-
Lower income
-
An Interesting Observation:
Married patients tended to have better treatment adherence, psychological support, and healthier eating habits, all of which contributed to improved outcomes.
What are the Main Findings from the Single-Center Analysis?
The analysis (2000-2023) included 84 myelofibrosis patients treated at Montefiore Medical Center.
-
Survival Rates:
-
2-year survival: 90%
-
5-year survival: 61%
-
Factors Linked to Survival:
-
Age was a significant predictor of worse survival.
-
Non-Hispanic Black patients had the lowest median survival, although the difference was not statistically significant.
-
Socioeconomic Observations:
Non-Hispanic Black and Hispanic patients resided in areas with higher socioeconomic stress compared to Non-Hispanic White patients.
What Influences Myelofibrosis Outcomes?
Several factors may affect how myelofibrosis progresses, along with your overall health, and the effectiveness of treatments. These include genetic mutations, age, blood counts, symptoms, and other underlying health conditions.
Genetic Mutations
Some patients have specific mutations linked to a more aggressive form of the disease. The most common mutations include:
-
JAK2 (Janus kinase 2) mutations, found in about 50-60% of patients.
-
CALR (calreticulin) mutations, found in about 20-30% of patients.
-
MPL (myeloproliferative leukemia protein) mutations, found in a smaller percentage of patients.
These mutations can influence how myelofibrosis progresses and how it responds to certain treatments.
Age
A patient’s age is a key factor for predicting how myelofibrosis will affect people and which treatment strategies will work best for them. For example, in myelofibrosis, older patients are prone to have more complications, and for younger patients, it may progress more slowly.
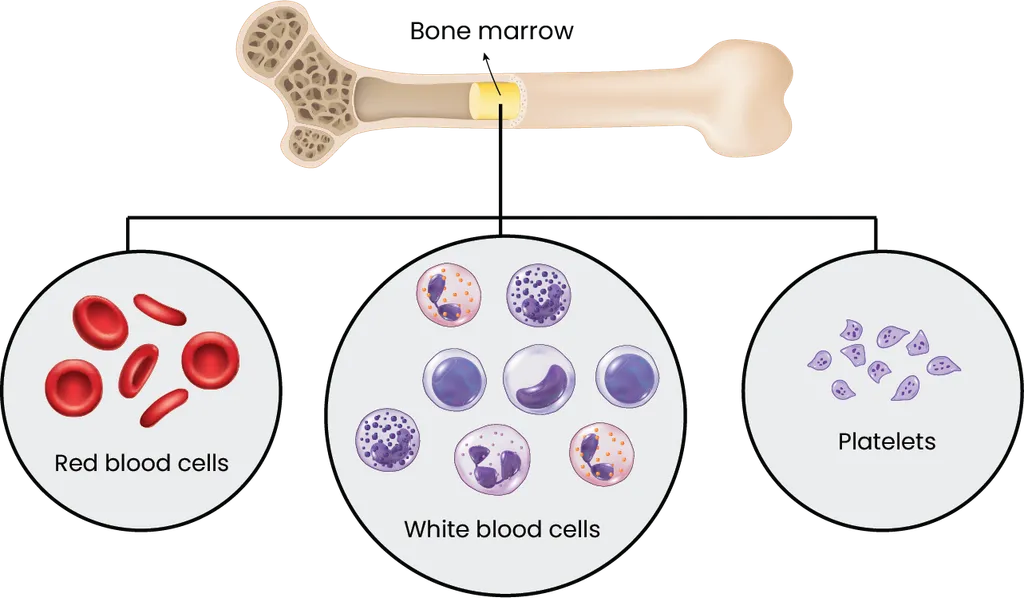
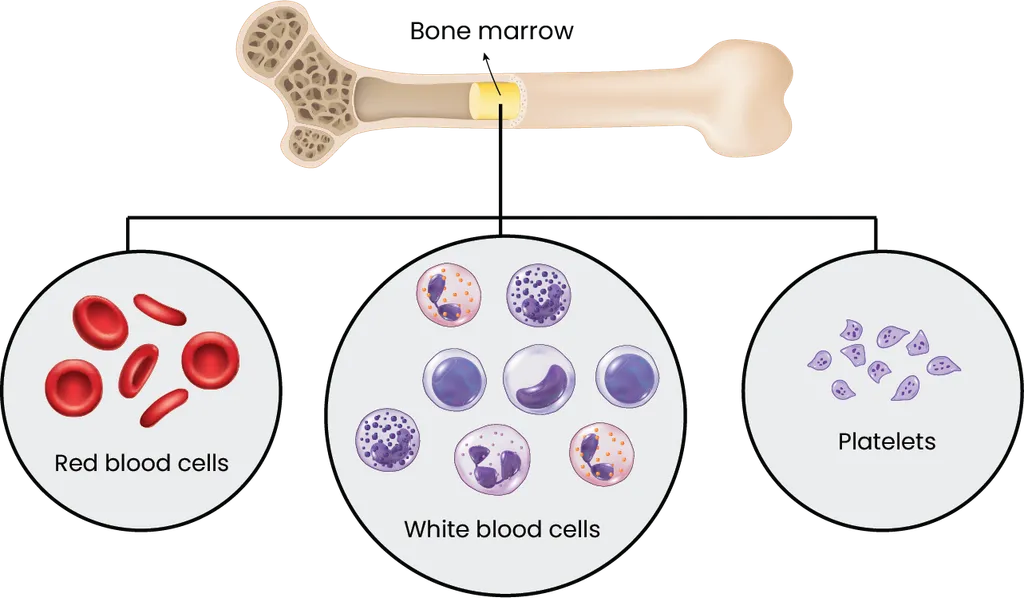
Blood Counts
Are essential for monitoring myelofibrosis progression and assessing prognosis.
-
Anemia (low red blood cell count) can be one of the first indicators of myelofibrosis and may be associated with a more aggressive form of the disease.
-
Leukocytosis (high white blood cell count) or leukopenia (low white blood cell count) can also affect outcomes because it interferes with the immune response.
-
Thrombocytopenia (low platelet count) may indicate a more advanced disease and can lead to complications like bleeding.
Spleen Size
Is increased in many myelofibrosis patients, known as splenomegaly, which can cause discomfort, early satiety, and a range of other symptoms. A larger spleen size often suggests a more advanced stage of your myelofibrosis. The size of your spleen can also impact treatment choices, as certain medications or procedures may be recommended to reduce spleen size.
Symptoms
Fatigue, night sweats, bone pain, and weight loss can provide insight into the evolution of myelofibrosis. Monitoring and managing these symptoms is key to improving one's quality of life.
Bone Marrow Fibrosis
The degree of scarring or fibrosis in the bone marrow is another factor that can affect outcomes. More advanced fibrosis is often associated with poorer survival rates. Regular monitoring through bone marrow biopsies may be needed to assess the extent of fibrosis.
Other Health Conditions
Such as heart disease, diabetes, or kidney problems, can also affect how well you respond to treatment. Patients with multiple health issues may have a more challenging time managing myelofibrosis and may experience more complications.
Cytogenetics
Chromosomal changes have been linked to more aggressive disease and worse outcomes. For example, patients with complex karyotypes, such as in ASXL1, SRSF2, EZH2, or IDH1/2 tend to have a higher risk of progression.
Prognostic Scoring Systems
Doctors use prognostic scoring systems to help predict outcomes and guide treatment decisions. One of the most widely used tools is the Dynamic International Prognostic Scoring System (DIPSS), which considers factors like age, hemoglobin levels, white blood cell counts, and the presence of symptoms. The DIPSS score places patients into different risk categories (low, intermediate, or high), helping doctors estimate survival and recommend appropriate therapies.
Another tool is the MIPSS70 (Mutation-Enhanced International Prognostic Scoring System), which evaluates genetic mutations like JAK2, CALR, and MPL. This system may provide a more detailed understanding of your disease risk based on genetic factors.
What Can Your Role Be in Managing Myelofibrosis?
While many factors influencing myelofibrosis outcomes are outside your control, there are ways you can take an active role in managing your health:
-
Regular checkups with your healthcare provider allow for early detection of changes in your condition and timely adjustments to your treatment plan.
-
Maintaining a healthy lifestyle with a balanced diet, regular exercise, and stress management can support your overall well-being and help you cope with the physical and emotional challenges of the disease.
-
Stay informed about new treatment options and clinical trials. Medical research is ongoing, and emerging therapies may offer new hope for patients with myelofibrosis.
How Can Treatments Affect Outcomes?
Various treatment options are available for myelofibrosis, and the treatment choice can impact your outcomes.
-
JAK inhibitors like ruxolitinib (Jakafi) are often used to manage symptoms and reduce spleen size. The study highlighted that the approval of ruxolitinib in 2011 significantly improved survival outcomes for myelofibrosis patients, highlighting the importance of access to new treatments.
-
Stem cell transplantation offers the potential for a cure but is usually only an option for younger, healthier patients due to its risks.
-
Supportive therapies such as blood transfusions or medications to address anemia, infection risk, and symptoms are commonly used to help manage myelofibrosis’s effects.
Final Thoughts
Understanding the factors that can affect your outcomes with myelofibrosis can help you make informed decisions about your treatment and care. While it’s natural to feel anxious about your diagnosis, staying informed, working closely with your healthcare team, and taking steps to manage your health can empower you to navigate your health. Always discuss your concerns and options with your doctor, who can help you choose the best path forward based on your unique situation.
Keep track of your health by creating a free HealthTree account!
If you want to keep track of your labs, even if they were at different facilities, you can look at them all in one place by securely connecting your records to HealthTree. Or create a free account to see personalized treatment options, find clinical trials, connect with other myelofibrosis patients, and so much more for free!
Source:
Myelofibrosis (MF) is a type of blood cancer that affects the bone marrow, leading to abnormal production of blood cells. Over time, scar tissue forms in the bone marrow, reducing its ability to make healthy blood cells. This can cause a wide range of symptoms, including fatigue, an enlarged spleen, and difficulty fighting infections. Myelofibrosis can develop on its own (primary MF) or as a progression from other conditions like polycythemia vera (PV) or essential thrombocythemia (ET).
While each case is unique, several important factors have been shown to impact how myelofibrosis develops and how patients respond to treatment.
If you've been diagnosed with myelofibrosis, you may have wondered what factors can potentially influence your health, disease progression, and outcomes. Understanding these factors can help you feel more informed and engaged in managing your health.
Recent Data for Myelofibrosis Risk Factors
A recent retrospective study published in the Annals of Hematology evaluated data from two sources:
-
The SEER database (2000-2021), 5,403 myelofibrosis patientsMontefiore Medical Center (2000-2023),, 84 cases.
The study examines how social and demographic factors impact survival in myelofibrosis, a rarely studied topic.
It shows that social and demographic factors, including sex, race, marital status, and income, are associated with survival in myelofibrosis. Addressing these social and demographic factors is key to improving overall health outcomes and providing fair care for all myelofibrosis patients.
What are the Main Findings from SEER Data?
The SEER database analysis (2000-2021) included 5,403 myelofibrosis patients, with a median age of 69 years. The majority (82%) were non-Hispanic White.
-
Survival Rates:
-
2-year survival: 69%
-
5-year survival: 42%
-
Factors Linked to Worse Survival:
-
Older age
-
Male sex
-
Diagnosis before 2011 (prior to ruxolitinib approval)
-
Predictors of Worse Overall Survival:
-
Non-Hispanic Black ethnicity
-
Unmarried status
-
Lower income
-
An Interesting Observation:
Married patients tended to have better treatment adherence, psychological support, and healthier eating habits, all of which contributed to improved outcomes.
What are the Main Findings from the Single-Center Analysis?
The analysis (2000-2023) included 84 myelofibrosis patients treated at Montefiore Medical Center.
-
Survival Rates:
-
2-year survival: 90%
-
5-year survival: 61%
-
Factors Linked to Survival:
-
Age was a significant predictor of worse survival.
-
Non-Hispanic Black patients had the lowest median survival, although the difference was not statistically significant.
-
Socioeconomic Observations:
Non-Hispanic Black and Hispanic patients resided in areas with higher socioeconomic stress compared to Non-Hispanic White patients.
What Influences Myelofibrosis Outcomes?
Several factors may affect how myelofibrosis progresses, along with your overall health, and the effectiveness of treatments. These include genetic mutations, age, blood counts, symptoms, and other underlying health conditions.
Genetic Mutations
Some patients have specific mutations linked to a more aggressive form of the disease. The most common mutations include:
-
JAK2 (Janus kinase 2) mutations, found in about 50-60% of patients.
-
CALR (calreticulin) mutations, found in about 20-30% of patients.
-
MPL (myeloproliferative leukemia protein) mutations, found in a smaller percentage of patients.
These mutations can influence how myelofibrosis progresses and how it responds to certain treatments.
Age
A patient’s age is a key factor for predicting how myelofibrosis will affect people and which treatment strategies will work best for them. For example, in myelofibrosis, older patients are prone to have more complications, and for younger patients, it may progress more slowly.
Blood Counts
Are essential for monitoring myelofibrosis progression and assessing prognosis.
-
Anemia (low red blood cell count) can be one of the first indicators of myelofibrosis and may be associated with a more aggressive form of the disease.
-
Leukocytosis (high white blood cell count) or leukopenia (low white blood cell count) can also affect outcomes because it interferes with the immune response.
-
Thrombocytopenia (low platelet count) may indicate a more advanced disease and can lead to complications like bleeding.
Spleen Size
Is increased in many myelofibrosis patients, known as splenomegaly, which can cause discomfort, early satiety, and a range of other symptoms. A larger spleen size often suggests a more advanced stage of your myelofibrosis. The size of your spleen can also impact treatment choices, as certain medications or procedures may be recommended to reduce spleen size.
Symptoms
Fatigue, night sweats, bone pain, and weight loss can provide insight into the evolution of myelofibrosis. Monitoring and managing these symptoms is key to improving one's quality of life.
Bone Marrow Fibrosis
The degree of scarring or fibrosis in the bone marrow is another factor that can affect outcomes. More advanced fibrosis is often associated with poorer survival rates. Regular monitoring through bone marrow biopsies may be needed to assess the extent of fibrosis.
Other Health Conditions
Such as heart disease, diabetes, or kidney problems, can also affect how well you respond to treatment. Patients with multiple health issues may have a more challenging time managing myelofibrosis and may experience more complications.
Cytogenetics
Chromosomal changes have been linked to more aggressive disease and worse outcomes. For example, patients with complex karyotypes, such as in ASXL1, SRSF2, EZH2, or IDH1/2 tend to have a higher risk of progression.
Prognostic Scoring Systems
Doctors use prognostic scoring systems to help predict outcomes and guide treatment decisions. One of the most widely used tools is the Dynamic International Prognostic Scoring System (DIPSS), which considers factors like age, hemoglobin levels, white blood cell counts, and the presence of symptoms. The DIPSS score places patients into different risk categories (low, intermediate, or high), helping doctors estimate survival and recommend appropriate therapies.
Another tool is the MIPSS70 (Mutation-Enhanced International Prognostic Scoring System), which evaluates genetic mutations like JAK2, CALR, and MPL. This system may provide a more detailed understanding of your disease risk based on genetic factors.
What Can Your Role Be in Managing Myelofibrosis?
While many factors influencing myelofibrosis outcomes are outside your control, there are ways you can take an active role in managing your health:
-
Regular checkups with your healthcare provider allow for early detection of changes in your condition and timely adjustments to your treatment plan.
-
Maintaining a healthy lifestyle with a balanced diet, regular exercise, and stress management can support your overall well-being and help you cope with the physical and emotional challenges of the disease.
-
Stay informed about new treatment options and clinical trials. Medical research is ongoing, and emerging therapies may offer new hope for patients with myelofibrosis.
How Can Treatments Affect Outcomes?
Various treatment options are available for myelofibrosis, and the treatment choice can impact your outcomes.
-
JAK inhibitors like ruxolitinib (Jakafi) are often used to manage symptoms and reduce spleen size. The study highlighted that the approval of ruxolitinib in 2011 significantly improved survival outcomes for myelofibrosis patients, highlighting the importance of access to new treatments.
-
Stem cell transplantation offers the potential for a cure but is usually only an option for younger, healthier patients due to its risks.
-
Supportive therapies such as blood transfusions or medications to address anemia, infection risk, and symptoms are commonly used to help manage myelofibrosis’s effects.
Final Thoughts
Understanding the factors that can affect your outcomes with myelofibrosis can help you make informed decisions about your treatment and care. While it’s natural to feel anxious about your diagnosis, staying informed, working closely with your healthcare team, and taking steps to manage your health can empower you to navigate your health. Always discuss your concerns and options with your doctor, who can help you choose the best path forward based on your unique situation.
Keep track of your health by creating a free HealthTree account!
If you want to keep track of your labs, even if they were at different facilities, you can look at them all in one place by securely connecting your records to HealthTree. Or create a free account to see personalized treatment options, find clinical trials, connect with other myelofibrosis patients, and so much more for free!
Source:

about the author
Jimena Vicencio
Jimena is an International Medical Graduate and a member of the HealthTree Writing team. She has a passion for languages and is currently learning Japanese. In her free time, she loves playing with her cats. Jimena is also pursuing a bachelor's degree in journalism.
More on Navigating Your Health
Trending Articles
Upcoming Events
Get the Latest Myeloproliferative Neoplasm Updates, Delivered to You.
By subscribing to the HealthTree newsletter, you'll receive the latest research, treatment updates, and expert insights to help you navigate your health.
Together we care.
Together we cure.
3x Faster.