Beyond Symptom Management: Modifying the Disease Course in Myelofibrosis

Disease-modifying therapies go beyond symptom management to slow disease progression and increase the likelihood of patient survival. They treat underlying causes rather than only manifestations or symptoms.
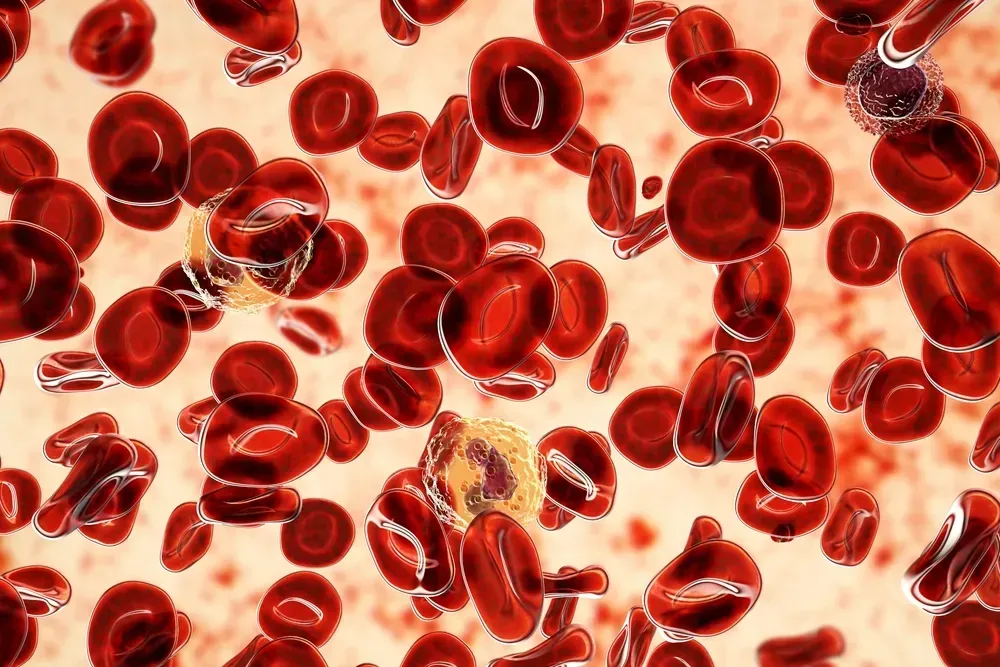
Janus kinase (JAK) inhibitors, the standard of care in patients with myelofibrosis (MF) for over a decade, help some key disease symptoms, such as enlarged spleen and fatigue − but they do not provide direct survival benefits. JAK inhibitors are primarily anti-inflammatory and have limited disease-modifying effects. Since they were the last great innovation for patients with MF, the medical community’s response to the disease has necessarily focused on symptom relief.
Unmet Need in Myelofibrosis: Disease-Modifying Treatment
However, research is advancing again, with the discovery of new therapeutic targets (such as nuclear factor–κB and the B-cell lymphoma-2 pathway) resulting in many novel agents under investigation. These include pelabresib, navitoclax, imetelstat, and navtemadlin. Clinical trials are assessing these medicines as monotherapy or in combination with ruxolitinib in patients with poor response to a JAK inhibitor or without any prior JAK inhibitor exposure.
These agents have potential disease-modifying effects. With this expanded horizon, investigators are able to employ new study endpoints, the most important of which are “progression-free survival” and “overall survival.” Simultaneously − and it is an exciting problem to have − a definition of disease modification in myelofibrosis must be determined.
Consensus is needed within the medical community to facilitate new responses to the disease and updated trial designs. For example, reductions in bone marrow fibrosis have been reported with both ruxolitinib and novel agents. Still, without evident increases in progression-free survival or overall survival, the importance of these reductions is uncertain.
Robust discussion is underway, and the definition will continue to evolve until a formal consensus is reached. One proposed definition states that:
Disease modification in myelofibrosis is a therapy that exerts a meaningful impact on survival outcomes and/or restoration of normal blood-cell production in conjunction with improvement in bone marrow fibrosis.
JAK Inhibition Will Continue to Play a Role
Despite the limited disease-modifying activity of JAK inhibitors, the JAK2 mutation is the most common in people with myelofibrosis. Therefore, the JAK pathway remains a pivotal feature of MF pathology, and JAK inhibition will not be disregarded moving forward. Combination therapies involving a novel agent plus a JAK inhibitor are expected. In fact, ruxolitinib−novel agent combinations have already shown improved benefits for patients in two international phase 3 clinical trials.
The JAK inhibitor ruxolitinib was the first FDA-approved medicine for treating myelofibrosis (in 2011), followed by fedratinib, pacritinib, and recently momelotinib. Ruxolitinib is still the preferred first-line treatment in appropriate patients, with the other JAK inhibitors serving as options if the response is suboptimal. In clinical trials, treatment with ruxolitinib was associated with spleen response and improvement of symptoms. However, approximately 50% of patients with myelofibrosis discontinue ruxolitinib due to reduced response or intolerance after about 3 years.
Within Approximately a Year ….
The possibility of disease modification for patients with myelofibrosis may transform clinical practice and treatment decision-making. More importantly, it could mean improved survival for patients. The pharmaceutical company behind pelabresib intends to submit the investigational medicine for approval in the US and Europe by the end of 2024. Change is coming … soon.
People who are educated about their care live longer, better lives. Sign up to receive our newsletter on myelofibrosis and stay up-to-date with the latest treatment advances:
Subscribe to the Myelofibrosis Newsletter
Sources:
- Myelofibrosis: Current unmet needs, emerging treatments, and future perspectives (2024)
- First-Line Ruxolitinib Combinations Boost Benefit Over Single Agent in Myelofibrosis (2023)
- Defining disease modification in myelofibrosis in the era of targeted therapy (2022)
- Disease Modification in Myelofibrosis: An Elusive Goal? (2022)
Disease-modifying therapies go beyond symptom management to slow disease progression and increase the likelihood of patient survival. They treat underlying causes rather than only manifestations or symptoms.
Janus kinase (JAK) inhibitors, the standard of care in patients with myelofibrosis (MF) for over a decade, help some key disease symptoms, such as enlarged spleen and fatigue − but they do not provide direct survival benefits. JAK inhibitors are primarily anti-inflammatory and have limited disease-modifying effects. Since they were the last great innovation for patients with MF, the medical community’s response to the disease has necessarily focused on symptom relief.
Unmet Need in Myelofibrosis: Disease-Modifying Treatment
However, research is advancing again, with the discovery of new therapeutic targets (such as nuclear factor–κB and the B-cell lymphoma-2 pathway) resulting in many novel agents under investigation. These include pelabresib, navitoclax, imetelstat, and navtemadlin. Clinical trials are assessing these medicines as monotherapy or in combination with ruxolitinib in patients with poor response to a JAK inhibitor or without any prior JAK inhibitor exposure.
These agents have potential disease-modifying effects. With this expanded horizon, investigators are able to employ new study endpoints, the most important of which are “progression-free survival” and “overall survival.” Simultaneously − and it is an exciting problem to have − a definition of disease modification in myelofibrosis must be determined.
Consensus is needed within the medical community to facilitate new responses to the disease and updated trial designs. For example, reductions in bone marrow fibrosis have been reported with both ruxolitinib and novel agents. Still, without evident increases in progression-free survival or overall survival, the importance of these reductions is uncertain.
Robust discussion is underway, and the definition will continue to evolve until a formal consensus is reached. One proposed definition states that:
Disease modification in myelofibrosis is a therapy that exerts a meaningful impact on survival outcomes and/or restoration of normal blood-cell production in conjunction with improvement in bone marrow fibrosis.
JAK Inhibition Will Continue to Play a Role
Despite the limited disease-modifying activity of JAK inhibitors, the JAK2 mutation is the most common in people with myelofibrosis. Therefore, the JAK pathway remains a pivotal feature of MF pathology, and JAK inhibition will not be disregarded moving forward. Combination therapies involving a novel agent plus a JAK inhibitor are expected. In fact, ruxolitinib−novel agent combinations have already shown improved benefits for patients in two international phase 3 clinical trials.
The JAK inhibitor ruxolitinib was the first FDA-approved medicine for treating myelofibrosis (in 2011), followed by fedratinib, pacritinib, and recently momelotinib. Ruxolitinib is still the preferred first-line treatment in appropriate patients, with the other JAK inhibitors serving as options if the response is suboptimal. In clinical trials, treatment with ruxolitinib was associated with spleen response and improvement of symptoms. However, approximately 50% of patients with myelofibrosis discontinue ruxolitinib due to reduced response or intolerance after about 3 years.
Within Approximately a Year ….
The possibility of disease modification for patients with myelofibrosis may transform clinical practice and treatment decision-making. More importantly, it could mean improved survival for patients. The pharmaceutical company behind pelabresib intends to submit the investigational medicine for approval in the US and Europe by the end of 2024. Change is coming … soon.
People who are educated about their care live longer, better lives. Sign up to receive our newsletter on myelofibrosis and stay up-to-date with the latest treatment advances:
Subscribe to the Myelofibrosis Newsletter
Sources:
- Myelofibrosis: Current unmet needs, emerging treatments, and future perspectives (2024)
- First-Line Ruxolitinib Combinations Boost Benefit Over Single Agent in Myelofibrosis (2023)
- Defining disease modification in myelofibrosis in the era of targeted therapy (2022)
- Disease Modification in Myelofibrosis: An Elusive Goal? (2022)
about the author
Jacqueline M. Mahon, MA
Jacqueline is delighted to be writing for HealthTree Foundation. She has extensive experience working in blood cancers as well as other oncologic and therapeutic areas. When not writing, she may be gardening, hiking, or playing with her rescue cat, Merlin.
More on Core Education
Trending Articles
Get the Latest Myeloproliferative Neoplasm Updates, Delivered to You.
By subscribing to the HealthTree newsletter, you'll receive the latest research, treatment updates, and expert insights to help you navigate your health.
Together we care.
Together we cure.