Why Do I Have Myelofibrosis?
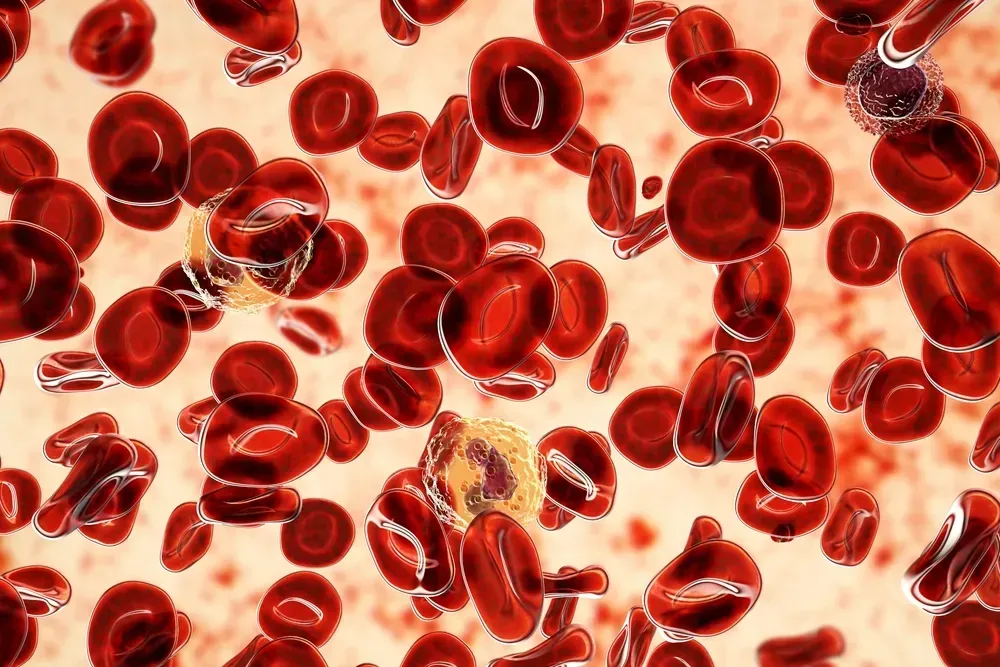
Myelofibrosis is a rare blood cancer and stem-cell disorder that causes scarring of the bone marrow. “Myelo” means bone, and “fibrosis” refers to the development of fibrous scar tissue.
Bone marrow is the inner, spongy part of the bone that makes blood cells. The stem cells in the bone marrow are the foundational elements for the specialized cells that compose blood. In myelofibrosis, these stem cells become mutated, although it is not known how these genetic mutations happen.
As the mutated stem cells replicate and divide into the specialized cells − white blood cells, red blood cells, or platelets − they pass on the mutation, and disorder results. Production of red blood cells declines, while white blood cells are overproduced. This disordered process causes a buildup of scar tissue and inflammation in the bone marrow.
In Myelofibrosis, the Blood Cell Production Is Disordered
In an example of homeostasis (maintenance of stability), the liver and spleen begin making more blood cells to compensate. However, these organs are not ideally suited for this purpose, and the shortage of red blood cells is not solved. In addition, the spleen has its own job, fighting infection, and when it undertakes double duty, it becomes enlarged.
This splenomegaly (enlarged spleen, pronounced “spleh-no-meh-guh-lee”), which is characteristic of myelofibrosis, can cause pain or discomfort in your abdomen or below your left ribs. You also may feel full even when you have barely eaten. Approximately 90% of people living with myelofibrosis have an enlarged spleen when they’re diagnosed.
Anemia, a condition that develops when there are not enough red blood cells to carry oxygen throughout the body, is a cardinal feature of myelofibrosis. Almost 40% of people with myelofibrosis have anemia at diagnosis, and anemia will eventually develop in all patients with this condition.
Myelofibrosis Can Progress to Leukemia
About 20% of people with myelofibrosis progress to acute myeloid leukemia (AML), a different type of blood cancer. In AML, mutated stem cells in the bone marrow overproduce monocytes and granulocytes, which are other specialized cells in the blood. Monocytes and granulocytes are not fully developed and, therefore, cannot work normally. An excess of monocytes and granulocytes is detrimental.
When AML arises from myelofibrosis, it can progress quickly (“acute”) and be difficult to treat. Over 15% of all people with AML will survive for 5 years or more after being diagnosed. Younger people diagnosed with AML tend to live longer than older people.
There is no staging system for the progression of myelofibrosis to AML because how it happens is not fully described. Many different genetic mutations appear to be involved, and the process differs according to which mutations first occur.
Researchers are Working to Determine the Causes of Myelofibrosis
No one knows what triggers the start of myelofibrosis. However, researchers have determined that it is not inherited genetically, so it does not run in families. People with myelofibrosis are usually older than 40, but the disease can occur at any age.
Risk factors associated with myelofibrosis include:
- Age over 65 years (average age of diagnosis is 65 years)
- Exposure to certain chemicals, such as toluene and benzene
- Exposure to very high levels of radiation
- Mutation of the Janus kinase 2 (JAK2) gene (50% to 60% of people with myelofibrosis)
- Mutation of the calreticulin (CALR) gene
- Mutation of the myeloproliferative leukemia protein (MPL) gene
However, some people with myelofibrosis don't have any identifiable gene mutations. Note, too, that stress does not cause myelofibrosis − but certainly, living and coping with a chronic disease can cause stress. It is important to learn strategies for managing fatigue, insomnia, pain, and emotional upset often associated with a diagnosis like this. (See sources below.)
The probable disease course or prognosis differs for each person with myelofibrosis. Some can live for many years without major symptoms developing, while for others, the disease progresses more quickly. The average survival rate is 6 years.
Learn more about myelofibrosis prognosis and survival with our 101 articles here: Myelofibrosis 101.
If you want to stay up-to-date with the latest treatment advances in myelofibrosis, sign up for our newsletter and join the HealthTree for Myelofibrosis community:
Sources:
Myelofibrosis is a rare blood cancer and stem-cell disorder that causes scarring of the bone marrow. “Myelo” means bone, and “fibrosis” refers to the development of fibrous scar tissue.
Bone marrow is the inner, spongy part of the bone that makes blood cells. The stem cells in the bone marrow are the foundational elements for the specialized cells that compose blood. In myelofibrosis, these stem cells become mutated, although it is not known how these genetic mutations happen.
As the mutated stem cells replicate and divide into the specialized cells − white blood cells, red blood cells, or platelets − they pass on the mutation, and disorder results. Production of red blood cells declines, while white blood cells are overproduced. This disordered process causes a buildup of scar tissue and inflammation in the bone marrow.
In Myelofibrosis, the Blood Cell Production Is Disordered
In an example of homeostasis (maintenance of stability), the liver and spleen begin making more blood cells to compensate. However, these organs are not ideally suited for this purpose, and the shortage of red blood cells is not solved. In addition, the spleen has its own job, fighting infection, and when it undertakes double duty, it becomes enlarged.
This splenomegaly (enlarged spleen, pronounced “spleh-no-meh-guh-lee”), which is characteristic of myelofibrosis, can cause pain or discomfort in your abdomen or below your left ribs. You also may feel full even when you have barely eaten. Approximately 90% of people living with myelofibrosis have an enlarged spleen when they’re diagnosed.
Anemia, a condition that develops when there are not enough red blood cells to carry oxygen throughout the body, is a cardinal feature of myelofibrosis. Almost 40% of people with myelofibrosis have anemia at diagnosis, and anemia will eventually develop in all patients with this condition.
Myelofibrosis Can Progress to Leukemia
About 20% of people with myelofibrosis progress to acute myeloid leukemia (AML), a different type of blood cancer. In AML, mutated stem cells in the bone marrow overproduce monocytes and granulocytes, which are other specialized cells in the blood. Monocytes and granulocytes are not fully developed and, therefore, cannot work normally. An excess of monocytes and granulocytes is detrimental.
When AML arises from myelofibrosis, it can progress quickly (“acute”) and be difficult to treat. Over 15% of all people with AML will survive for 5 years or more after being diagnosed. Younger people diagnosed with AML tend to live longer than older people.
There is no staging system for the progression of myelofibrosis to AML because how it happens is not fully described. Many different genetic mutations appear to be involved, and the process differs according to which mutations first occur.
Researchers are Working to Determine the Causes of Myelofibrosis
No one knows what triggers the start of myelofibrosis. However, researchers have determined that it is not inherited genetically, so it does not run in families. People with myelofibrosis are usually older than 40, but the disease can occur at any age.
Risk factors associated with myelofibrosis include:
- Age over 65 years (average age of diagnosis is 65 years)
- Exposure to certain chemicals, such as toluene and benzene
- Exposure to very high levels of radiation
- Mutation of the Janus kinase 2 (JAK2) gene (50% to 60% of people with myelofibrosis)
- Mutation of the calreticulin (CALR) gene
- Mutation of the myeloproliferative leukemia protein (MPL) gene
However, some people with myelofibrosis don't have any identifiable gene mutations. Note, too, that stress does not cause myelofibrosis − but certainly, living and coping with a chronic disease can cause stress. It is important to learn strategies for managing fatigue, insomnia, pain, and emotional upset often associated with a diagnosis like this. (See sources below.)
The probable disease course or prognosis differs for each person with myelofibrosis. Some can live for many years without major symptoms developing, while for others, the disease progresses more quickly. The average survival rate is 6 years.
Learn more about myelofibrosis prognosis and survival with our 101 articles here: Myelofibrosis 101.
If you want to stay up-to-date with the latest treatment advances in myelofibrosis, sign up for our newsletter and join the HealthTree for Myelofibrosis community:
Sources:
about the author
Jacqueline M. Mahon, MA
Jacqueline is delighted to be writing for HealthTree Foundation. She has extensive experience working in blood cancers as well as other oncologic and therapeutic areas. When not writing, she may be gardening, hiking, or playing with her rescue cat, Merlin.
More on Core Education
Trending Articles
Get the Latest Myelofibrosis Updates, Delivered to You.
By subscribing to the HealthTree newsletter, you'll receive the latest research, treatment updates, and expert insights to help you navigate your health.
Together we care.
Together we cure.