Updates in Treatment Options for TP53-Mutant AML and MDS
Understanding the TP53 Mutation in AML and MDS
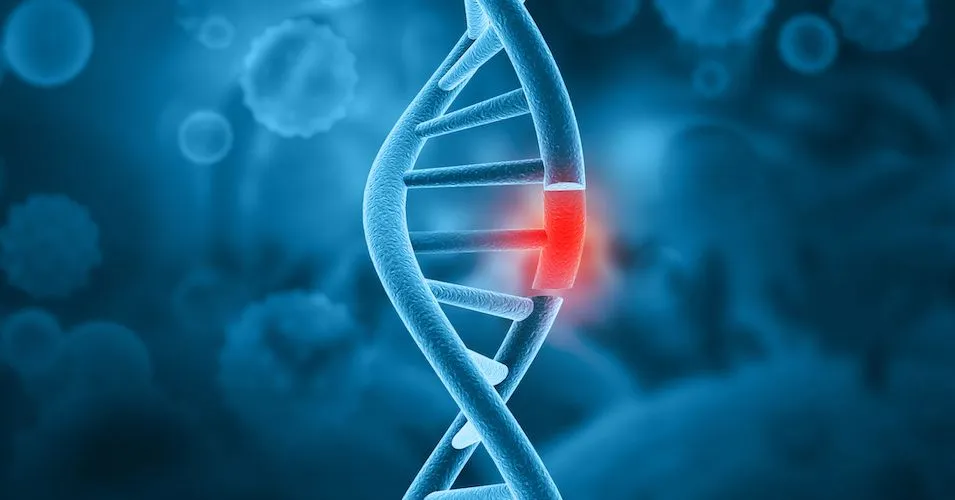
People with acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS) may hear about different gene mutations that occur in cancer. These differences make up the types of AML and MDS.
Knowing your AML/MDS type is important because it can influence which treatment may be more effective for you and help you understand how the cancer may behave.
Your AML specialist can run tests like next-generation DNA sequencing to find gene mutations. If they suspect part of a gene to be deleted rather than mutated, tests like fluorescence in situ hybridization (FISH) can help.
One of these mutations in AML and MDS cells is the TP53 gene mutation. In cells, the TP53 gene codes for the protein p53. If the gene is altered, the protein doesn’t work as it should in repairing the cell’s DNA, suppressing tumors, and telling cells beyond repair to die.
TP53 gene mutations or deletions [referred to as del(17p)] cause higher-risk forms of cancer, including in AML and MDS.
How Many MDS and AML Patients Have the TP53 Mutation?
It’s important to note that the genetic makeup of your MDS or AML can evolve over time, especially after receiving treatment. You and your doctor should monitor your genetic makeup at each relapse or treatment change.
If you have not received treatment before, the TP53 gene mutation is found in up to 10% of AML and MDS patients.
If you have received treatment before, the percentage of AML and MDS patients who have the TP53 gene mutation increases to 40%.
Which Treatments Work and Don’t Work for TP53 Mutated AML and MDS?
Cancer cells with the TP53 gene mutation do not respond to chemotherapy. Because chemotherapy is one of the standards of AML care, what other treatments should be used for patients with TP53?
Read on to learn what research in this area has not been successful and what has promise.
What Isn’t Working
To try and reactivate the p53 protein, researchers used a medicine called eprenetapopt in combination with other AML treatments like venetoclax and azacitidine.
Although early findings were promising, later phase III clinical trial results did not show this treatment to help TP53-mutant AML and MDS patients have meaningful outcomes.
Another treatment of an anti-CD47 antibody called magrolimab was tried and did not work for TP53-mutant AML or MDS.
What May Work
AML specialists are trying treatments that don’t depend on the cell’s signaling system that tells it to self-destruct (apoptosis), as this involves p53 use.
If you have TP53-mutant AML or MDS, ask your specialist about clinical trials that involve cellular therapies. These include treatments like anti-CD123 antibodies or CAR therapies from donors, also referred to as “off-the-shelf” cellular treatments.
Off-the-shelf CAR therapies may improve the chances of AML and MDS patients achieving remission as the donor T-cells or natural killer (NK) cells are not exhausted, as seen in a patient’s own T cells and NK cells.
Click the following link to learn more: Off-the-Shelf CAR NK Cell Therapy for Relapsed/Refractory AML and MDS
Conclusion
In summary, AML and MDS patients who have the TP53 gene mutation are encouraged to find and/or meet with their specialist to discuss receiving cellular therapies through clinical trials.
Some of these cellular therapies include an anti-CD123 antibody or off-the-self CAR treatments, which use donor immune system cells to kill cancer cells. These new treatments may help overcome the treatment resistance TP53-mutant AML and MDS cells have to chemotherapy.
Track Cancer Genetics for Free
If you haven’t already, click the button below and gain the benefits of a free HealthTree Cure Hub Registry account. Doing so will provide access to features like tracking cancer genetics and labs, all in one place.
Source:
Understanding the TP53 Mutation in AML and MDS
People with acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS) may hear about different gene mutations that occur in cancer. These differences make up the types of AML and MDS.
Knowing your AML/MDS type is important because it can influence which treatment may be more effective for you and help you understand how the cancer may behave.
Your AML specialist can run tests like next-generation DNA sequencing to find gene mutations. If they suspect part of a gene to be deleted rather than mutated, tests like fluorescence in situ hybridization (FISH) can help.
One of these mutations in AML and MDS cells is the TP53 gene mutation. In cells, the TP53 gene codes for the protein p53. If the gene is altered, the protein doesn’t work as it should in repairing the cell’s DNA, suppressing tumors, and telling cells beyond repair to die.
TP53 gene mutations or deletions [referred to as del(17p)] cause higher-risk forms of cancer, including in AML and MDS.
How Many MDS and AML Patients Have the TP53 Mutation?
It’s important to note that the genetic makeup of your MDS or AML can evolve over time, especially after receiving treatment. You and your doctor should monitor your genetic makeup at each relapse or treatment change.
If you have not received treatment before, the TP53 gene mutation is found in up to 10% of AML and MDS patients.
If you have received treatment before, the percentage of AML and MDS patients who have the TP53 gene mutation increases to 40%.
Which Treatments Work and Don’t Work for TP53 Mutated AML and MDS?
Cancer cells with the TP53 gene mutation do not respond to chemotherapy. Because chemotherapy is one of the standards of AML care, what other treatments should be used for patients with TP53?
Read on to learn what research in this area has not been successful and what has promise.
What Isn’t Working
To try and reactivate the p53 protein, researchers used a medicine called eprenetapopt in combination with other AML treatments like venetoclax and azacitidine.
Although early findings were promising, later phase III clinical trial results did not show this treatment to help TP53-mutant AML and MDS patients have meaningful outcomes.
Another treatment of an anti-CD47 antibody called magrolimab was tried and did not work for TP53-mutant AML or MDS.
What May Work
AML specialists are trying treatments that don’t depend on the cell’s signaling system that tells it to self-destruct (apoptosis), as this involves p53 use.
If you have TP53-mutant AML or MDS, ask your specialist about clinical trials that involve cellular therapies. These include treatments like anti-CD123 antibodies or CAR therapies from donors, also referred to as “off-the-shelf” cellular treatments.
Off-the-shelf CAR therapies may improve the chances of AML and MDS patients achieving remission as the donor T-cells or natural killer (NK) cells are not exhausted, as seen in a patient’s own T cells and NK cells.
Click the following link to learn more: Off-the-Shelf CAR NK Cell Therapy for Relapsed/Refractory AML and MDS
Conclusion
In summary, AML and MDS patients who have the TP53 gene mutation are encouraged to find and/or meet with their specialist to discuss receiving cellular therapies through clinical trials.
Some of these cellular therapies include an anti-CD123 antibody or off-the-self CAR treatments, which use donor immune system cells to kill cancer cells. These new treatments may help overcome the treatment resistance TP53-mutant AML and MDS cells have to chemotherapy.
Track Cancer Genetics for Free
If you haven’t already, click the button below and gain the benefits of a free HealthTree Cure Hub Registry account. Doing so will provide access to features like tracking cancer genetics and labs, all in one place.
Source:

about the author
Megan Heaps
Megan joined HealthTree in 2022. She enjoys helping patients and their care partners understand the various aspects of the cancer. This understanding enables them to better advocate for themselves and improve their treatment outcomes.
More on Treatment Advances
Get the Latest Leukemia Updates, Delivered to You.
By subscribing to the HealthTree newsletter, you'll receive the latest research, treatment updates, and expert insights to help you navigate your health.
Thanks to our HealthTree Community for Leukemia Sponsors: