What are Bispecific Antibodies for Follicular Lymphoma?
What are bispecific antibodies, and when are they used to treat follicular lymphoma? Learn answers to these questions and more below!
What are Bispecific Antibodies?
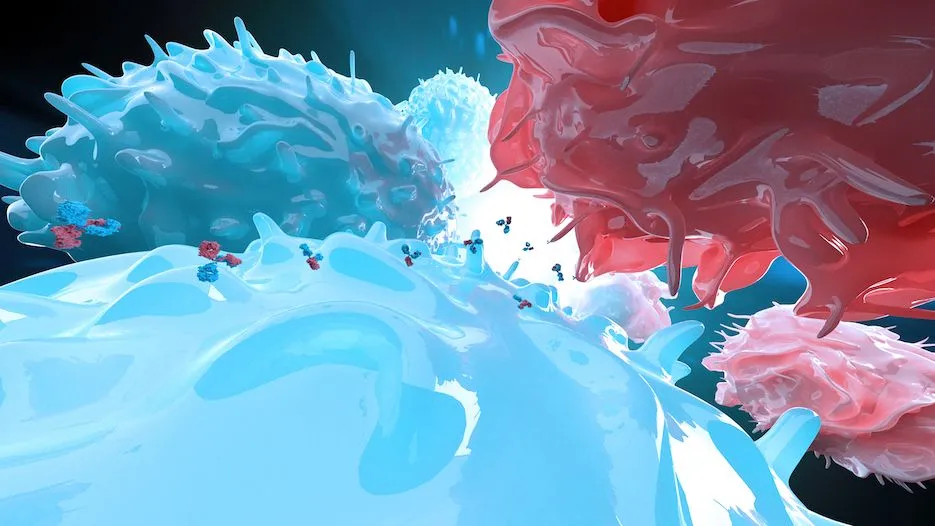
You may be familiar with monoclonal antibodies used in follicular lymphoma treatment, such as rituximab (Rituxan, Genentech) and obinutuzumab (Gazyva, Genentech). Monoclonal antibodies target one protein on the surface of cancerous B-cells like follicular lymphoma, called CD20. Binding to this surface protein signals the immune system to target and destroy the cancer cells.
Bispecific antibodies attach to two targets: the CD20 surface protein on follicular lymphoma cells and the surface protein on cancer-killing T-cells. By binding to both targets, the bispecific antibodies act as a bridge, connecting the T-cells to the cancer cell.
This mechanism of action is helpful as T-cells often have difficulty finding and killing follicular lymphoma cells on their own.
What are the FDA-Approved Bispecific Antibodies for Follicular Lymphoma?
The FDA-approved bispecific antibodies for follicular lymphoma include epcoritamab (Epkinly, Genmab and AbbVie) and mosunetuzumab (Lunsumio, Genentech). People with follicular lymphoma qualify to receive these treatments as a third-line therapy.
Third-line therapy is available to people who have already tried two previous follicular lymphoma treatments. Click here to learn more about follicular lymphoma therapies.
The main differences between epcoritamab and mosunetuzumab are how they are administered and for how long.
- Epcoritamab
- Administered by subcutaneous injection (shot under the skin).
- Continuous-duration therapy; meaning the medicine is given indefinitely until follicular lymphoma cells stop responding to treatment.
- 82% of patients show a reduction of signs/symptoms of follicular lymphoma.
- Remission lasts an average of 15.4 months.
- Mosunetuzumab
- Administered by either intravenous infusion (IV) or, as of December 2025, a new version is available as a subcutaneous injection.
- Fixed-duration therapy: it is administered for up to 17 months. However, patients can stop at eight months if they experience reduced signs and symptoms of their follicular lymphoma.
- 80% of patients achieve reduced signs/symptoms of follicular lymphoma.
- Remission lasts an average of 23 months.
What are the Side Effects of Bispecific Antibodies?
Bispecific antibodies have fewer side effects than CAR T-cell therapies. The primary concern with bispecific antibodies is cytokine release syndrome (CRS), which occurs when the activated T-cells release a high level of inflammatory molecules called cytokines during the treatment process.
CRS typically presents with symptoms like fever, which can escalate to more severe conditions such as low blood pressure and high heart rate. Despite its potential severity, CRS can often be managed with prescribed steroids as initial treatments. However, hospital admission is recommended for more severe or persistent symptoms.
People who receive bispecific antibodies may also experience brain-related side effects like headaches and confusion. These occur less often than with CAR T-cell therapy, affecting fewer than 10% of patients.
Other risks include infections and prolonged low counts of various blood cells (cytopenias), which are generally less frequent but require careful monitoring.
Encouragingly, recent studies and clinical trials indicate that even patients with significant comorbidities can tolerate bispecific antibodies well, with no deaths attributed to CRS reported in these studies. As such, while bispecific antibodies share some toxicities with other cancer therapies, their rapid availability and ease of administration over extended periods make them an important option in treating follicular lymphoma.
Conclusion
People with follicular lymphoma may be able to receive an FDA-approved bispecific antibody, such as epcoritamab or mosunetuzumab, as their third-line therapy. These treatments have manageable side effects and help the majority of patients achieve remission for an extended period of time.
Stay updated with the latest news on research and treatment of follicular lymphoma with HealthTree. Subscribe to our newsletter today!
FOLLICULAR LYMPHOMA NEWSLETTER
Sources:
- Lunsumio
- Epkinly
- Epcoritamab SC Monotherapy Leads to Deep and Durable Responses in Patients with Relapsed or Refractory Follicular Lymphoma: First Data Disclosure from the Epcore NHL-1 Follicular Lymphoma Dose-Expansion Cohort
- FDA approves Roche’s Lunsumio VELO™ for subcutaneous use in relapsed or refractory follicular lymphoma
What are bispecific antibodies, and when are they used to treat follicular lymphoma? Learn answers to these questions and more below!
What are Bispecific Antibodies?
You may be familiar with monoclonal antibodies used in follicular lymphoma treatment, such as rituximab (Rituxan, Genentech) and obinutuzumab (Gazyva, Genentech). Monoclonal antibodies target one protein on the surface of cancerous B-cells like follicular lymphoma, called CD20. Binding to this surface protein signals the immune system to target and destroy the cancer cells.
Bispecific antibodies attach to two targets: the CD20 surface protein on follicular lymphoma cells and the surface protein on cancer-killing T-cells. By binding to both targets, the bispecific antibodies act as a bridge, connecting the T-cells to the cancer cell.
This mechanism of action is helpful as T-cells often have difficulty finding and killing follicular lymphoma cells on their own.
What are the FDA-Approved Bispecific Antibodies for Follicular Lymphoma?
The FDA-approved bispecific antibodies for follicular lymphoma include epcoritamab (Epkinly, Genmab and AbbVie) and mosunetuzumab (Lunsumio, Genentech). People with follicular lymphoma qualify to receive these treatments as a third-line therapy.
Third-line therapy is available to people who have already tried two previous follicular lymphoma treatments. Click here to learn more about follicular lymphoma therapies.
The main differences between epcoritamab and mosunetuzumab are how they are administered and for how long.
- Epcoritamab
- Administered by subcutaneous injection (shot under the skin).
- Continuous-duration therapy; meaning the medicine is given indefinitely until follicular lymphoma cells stop responding to treatment.
- 82% of patients show a reduction of signs/symptoms of follicular lymphoma.
- Remission lasts an average of 15.4 months.
- Mosunetuzumab
- Administered by either intravenous infusion (IV) or, as of December 2025, a new version is available as a subcutaneous injection.
- Fixed-duration therapy: it is administered for up to 17 months. However, patients can stop at eight months if they experience reduced signs and symptoms of their follicular lymphoma.
- 80% of patients achieve reduced signs/symptoms of follicular lymphoma.
- Remission lasts an average of 23 months.
What are the Side Effects of Bispecific Antibodies?
Bispecific antibodies have fewer side effects than CAR T-cell therapies. The primary concern with bispecific antibodies is cytokine release syndrome (CRS), which occurs when the activated T-cells release a high level of inflammatory molecules called cytokines during the treatment process.
CRS typically presents with symptoms like fever, which can escalate to more severe conditions such as low blood pressure and high heart rate. Despite its potential severity, CRS can often be managed with prescribed steroids as initial treatments. However, hospital admission is recommended for more severe or persistent symptoms.
People who receive bispecific antibodies may also experience brain-related side effects like headaches and confusion. These occur less often than with CAR T-cell therapy, affecting fewer than 10% of patients.
Other risks include infections and prolonged low counts of various blood cells (cytopenias), which are generally less frequent but require careful monitoring.
Encouragingly, recent studies and clinical trials indicate that even patients with significant comorbidities can tolerate bispecific antibodies well, with no deaths attributed to CRS reported in these studies. As such, while bispecific antibodies share some toxicities with other cancer therapies, their rapid availability and ease of administration over extended periods make them an important option in treating follicular lymphoma.
Conclusion
People with follicular lymphoma may be able to receive an FDA-approved bispecific antibody, such as epcoritamab or mosunetuzumab, as their third-line therapy. These treatments have manageable side effects and help the majority of patients achieve remission for an extended period of time.
Stay updated with the latest news on research and treatment of follicular lymphoma with HealthTree. Subscribe to our newsletter today!
FOLLICULAR LYMPHOMA NEWSLETTER
Sources:
- Lunsumio
- Epkinly
- Epcoritamab SC Monotherapy Leads to Deep and Durable Responses in Patients with Relapsed or Refractory Follicular Lymphoma: First Data Disclosure from the Epcore NHL-1 Follicular Lymphoma Dose-Expansion Cohort
- FDA approves Roche’s Lunsumio VELO™ for subcutaneous use in relapsed or refractory follicular lymphoma

about the author
Megan Heaps
Megan joined HealthTree in 2022. She enjoys helping patients and their care partners understand the various aspects of the cancer. This understanding enables them to better advocate for themselves and improve their treatment outcomes.
More on Core Education
Trending Articles
Get the Latest Non-Hodgkin Lymphoma Updates, Delivered to You.
By subscribing to the HealthTree newsletter, you'll receive the latest research, treatment updates, and expert insights to help you navigate your health.
Together we care.
Together we cure.