Factors that Influence Blood Transfusion Needs for DLBCL Patients Receiving CAR T-Cell Therapy

Diffuse large B-cell lymphoma (DLBCL) patients who receive CAR T-cell therapy, a treatment that modifies a patient’s T-cells to more effectively kill cancer cells, may need blood transfusions before, during, and after treatment. Researchers conducted a study to evaluate if certain factors influence some patients to need more blood transfusions than others surrounding CAR T-cell therapy, as well as the impact transfusions had on patient survival.
What is a Blood Transfusion?
A blood transfusion is a medical procedure in which blood cells are transferred from one person (the donor) to another (the recipient). Recipients often need a transfusion if their blood counts are low. For example, when a patient has anemia, a condition associated with low red blood cells, or thrombocytopenia, a condition associated with low platelets.
Patients who require a blood transfusion will need to travel to their treatment facility. Receiving the transfusion can take up to 4 hours for red blood cells and up to 30 minutes for platelets.
Blood Transfusions Surrounding Bridging Therapy
Since the manufacturing process for CAR T-cell therapy can take up to several weeks, patients who are waiting often need chemotherapy to get them through this time period. This is called bridging therapy.
Chemotherapy can disrupt bone marrow function, which is the part of the body where new blood cells are created. The researchers found that the need for blood transfusions significantly increased during this bridging therapy period and peaked in the first month after CAR-T-cell therapy, where over half of the patients required at least one blood transfusion.
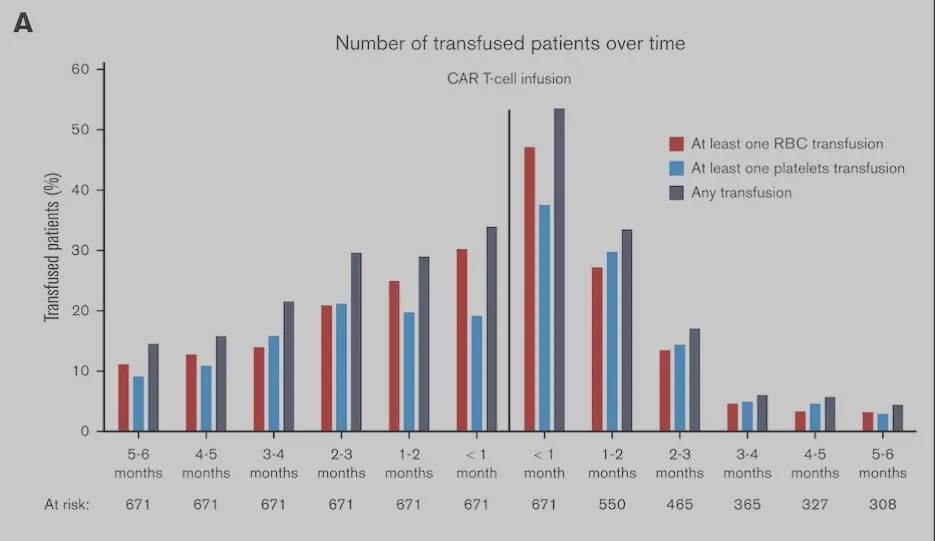
Figure adapted from: Vic, S., & Thibert, J. (2024). Transfusion needs after CAR T-cell therapy for large B-cell lymphoma: predictive factors and outcome (a DESCAR-T study) Blood Adv, 2024(6), 1573–1585.
What Increases My Risk For Needing Blood Transfusions After CAR T-Cell Therapy?
The researchers found that there were several risk factors that influenced whether patients needed blood infusions after their CAR T-cell therapy. They separated their findings into risk factors related to an early stage and a late stage following CAR T-cell therapy.
Risk factors for needing red blood cell and platelet transfusions in the early stages (0-30 days) after CAR T-cell therapy included:
- Over 60 years old
- Had difficulty taking care of themselves/frail (ECOG score of 2 or higher)
- Had been treated with the CAR T-cell therapy axi-cel (Yescarta) instead of tisa-cel (Kymriah)
- Had received at least 1 blood transfusion before CAR T-cell therapy
- Had high inflammation and low blood cell counts before CAR T-cell therapy
Risk factors for needing blood cell transfusions in the late stages (30 days to 6 months) after CAR T-cell therapy included:
- Received at least 1 blood transfusion before CAR T-cell therapy
- Had high inflammation and low blood cell counts before CAR T-cell therapy
- Patients with high brain inflammation (nervous system damage that may be caused by CAR T-cell therapy) have higher needs of red blood cell transfusions
- Patients who had been treated with tocilizumab (a steroid used to treat CAR T-cell therapy side effects) increased their need for platelet transfusions
Impact of Blood Transfusions on Relapse and Patient Survival Outcomes
The majority of patients (71.8%) achieved remission following CAR T-cell therapy (significantly reduced disease signs/symptoms). The researchers did not find that blood infusions impacted the response to the treatment.
The researchers did find, however, that blood transfusions impacted the average time to relapse (disease coming back after treatment) and overall survival following CAR T-cell therapy.
This study suggests that early red blood cell transfusions after CAR T-cell therapy may be linked to higher risk of relapse and lower overall survival rates. Conversely, patients who didn’t need early red blood cell transfusions, experienced longer relapse-free periods and improved overall survival. For platelet transfusions, the timing seems less critical, but overall, patients who did not require transfusions within the first month or up to 6 months after treatment had a better prognosis.
This study provides crucial insights that could lead to better management strategies for DLBCL patients undergoing CAR T-cell therapy. Understanding areas that increase the need for blood transfusions surrounding CAR T-cell therapy, may help healthcare providers better prepare for, manage, and reduce the need of blood transfusions for these patients, potentially improving their quality and length of life.
Join the HealthTree for DLBCL Newsletter to Learn More!
We invite you to join the HealthTree for DLBCL newsletter by clicking the button below to stay up to date on the latest advancements in diffuse large B-cell lymphoma.
Join the HealthTree for DLBCL Newsletter
Sources
Diffuse large B-cell lymphoma (DLBCL) patients who receive CAR T-cell therapy, a treatment that modifies a patient’s T-cells to more effectively kill cancer cells, may need blood transfusions before, during, and after treatment. Researchers conducted a study to evaluate if certain factors influence some patients to need more blood transfusions than others surrounding CAR T-cell therapy, as well as the impact transfusions had on patient survival.
What is a Blood Transfusion?
A blood transfusion is a medical procedure in which blood cells are transferred from one person (the donor) to another (the recipient). Recipients often need a transfusion if their blood counts are low. For example, when a patient has anemia, a condition associated with low red blood cells, or thrombocytopenia, a condition associated with low platelets.
Patients who require a blood transfusion will need to travel to their treatment facility. Receiving the transfusion can take up to 4 hours for red blood cells and up to 30 minutes for platelets.
Blood Transfusions Surrounding Bridging Therapy
Since the manufacturing process for CAR T-cell therapy can take up to several weeks, patients who are waiting often need chemotherapy to get them through this time period. This is called bridging therapy.
Chemotherapy can disrupt bone marrow function, which is the part of the body where new blood cells are created. The researchers found that the need for blood transfusions significantly increased during this bridging therapy period and peaked in the first month after CAR-T-cell therapy, where over half of the patients required at least one blood transfusion.
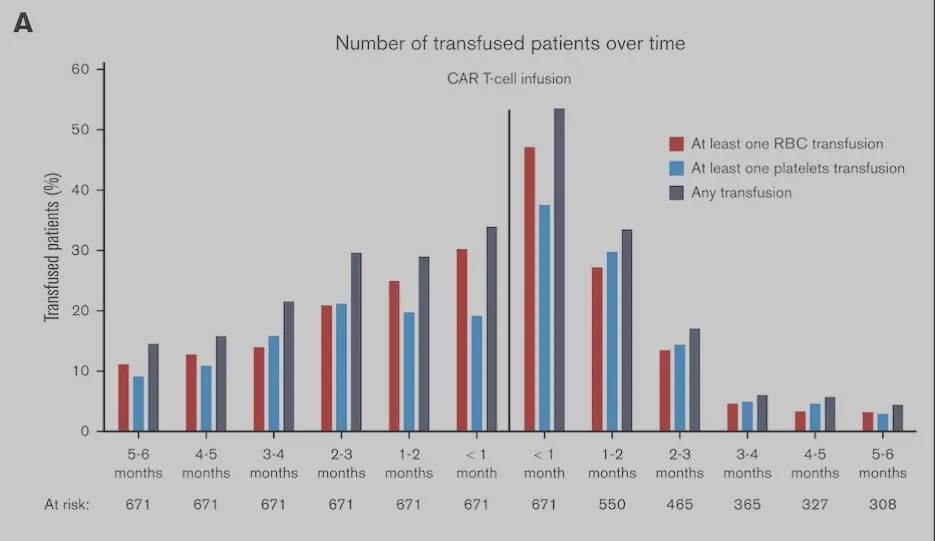
Figure adapted from: Vic, S., & Thibert, J. (2024). Transfusion needs after CAR T-cell therapy for large B-cell lymphoma: predictive factors and outcome (a DESCAR-T study) Blood Adv, 2024(6), 1573–1585.
What Increases My Risk For Needing Blood Transfusions After CAR T-Cell Therapy?
The researchers found that there were several risk factors that influenced whether patients needed blood infusions after their CAR T-cell therapy. They separated their findings into risk factors related to an early stage and a late stage following CAR T-cell therapy.
Risk factors for needing red blood cell and platelet transfusions in the early stages (0-30 days) after CAR T-cell therapy included:
- Over 60 years old
- Had difficulty taking care of themselves/frail (ECOG score of 2 or higher)
- Had been treated with the CAR T-cell therapy axi-cel (Yescarta) instead of tisa-cel (Kymriah)
- Had received at least 1 blood transfusion before CAR T-cell therapy
- Had high inflammation and low blood cell counts before CAR T-cell therapy
Risk factors for needing blood cell transfusions in the late stages (30 days to 6 months) after CAR T-cell therapy included:
- Received at least 1 blood transfusion before CAR T-cell therapy
- Had high inflammation and low blood cell counts before CAR T-cell therapy
- Patients with high brain inflammation (nervous system damage that may be caused by CAR T-cell therapy) have higher needs of red blood cell transfusions
- Patients who had been treated with tocilizumab (a steroid used to treat CAR T-cell therapy side effects) increased their need for platelet transfusions
Impact of Blood Transfusions on Relapse and Patient Survival Outcomes
The majority of patients (71.8%) achieved remission following CAR T-cell therapy (significantly reduced disease signs/symptoms). The researchers did not find that blood infusions impacted the response to the treatment.
The researchers did find, however, that blood transfusions impacted the average time to relapse (disease coming back after treatment) and overall survival following CAR T-cell therapy.
This study suggests that early red blood cell transfusions after CAR T-cell therapy may be linked to higher risk of relapse and lower overall survival rates. Conversely, patients who didn’t need early red blood cell transfusions, experienced longer relapse-free periods and improved overall survival. For platelet transfusions, the timing seems less critical, but overall, patients who did not require transfusions within the first month or up to 6 months after treatment had a better prognosis.
This study provides crucial insights that could lead to better management strategies for DLBCL patients undergoing CAR T-cell therapy. Understanding areas that increase the need for blood transfusions surrounding CAR T-cell therapy, may help healthcare providers better prepare for, manage, and reduce the need of blood transfusions for these patients, potentially improving their quality and length of life.
Join the HealthTree for DLBCL Newsletter to Learn More!
We invite you to join the HealthTree for DLBCL newsletter by clicking the button below to stay up to date on the latest advancements in diffuse large B-cell lymphoma.
Join the HealthTree for DLBCL Newsletter
Sources

about the author
Megan Heaps
Megan joined HealthTree in 2022. She enjoys helping patients and their care partners understand the various aspects of the cancer. This understanding enables them to better advocate for themselves and improve their treatment outcomes.
More on Treatment Advances
Trending Articles
Get the Latest Large B Cell Lymphoma Updates, Delivered to You.
By subscribing to the HealthTree newsletter, you'll receive the latest research, treatment updates, and expert insights to help you navigate your health.
Together we care.
Together we cure.