Using all the Myeloma Tools in the Toolbox with Clifton C. Mo, MD Dana-Farber Cancer Institute

Episode Summary
Dr. Clifton Mo of Dana Farber Cancer Institue shares a multitude of tools available in the myeloma toolbox. This includes all of the "standard of care" drugs that we are familiar with such as immunomodulators, proteasome inhibitors, steroids, monoclonal antibodies as well as tools in development.
He reviews triplet combo treatment options at first relapse and his preference to use Kyprolis in the mix, especially when given a more aggressive myeloma.
Dr. Mo explains how antibody drug conjugates (ADCs) work and how the first ADC, BLENREP, may be making a comeback. He shares how dexamethasone can be reduced or stopped under certain conditions. He explains BCL-2 inhibitors like venetoclax and how they are making their way through clinical trials.
Dr. Mo describes celmods and how they work and are a promising new class of drugs. He also described how an XPO1 inhibitor called selinexor is being used both with the celmods and alone as an agent that works well for higher risk myeloma.
This shows myeloma patients how fortunate we are to have these tools available and speaks to the importance of having a myeloma specialist on your team who can help you make treatment decisions. This can be done alone or in partnership with your local oncologist. There is data that shows that having a specialist on year team leads to longer life.
Full Transcript
Jenny: Welcome to today's episode of the Health Tree Podcast for Multiple Myeloma, a show that connects patients with myeloma researchers. I'm your host, Jenny Ahlstrom, and we'd like to thank our episode sponsor, Karyopharm, for support of this program. Now, before we get started with today's show, I'd like to share our major announcement for Myeloma Action Month.
On Friday, March 1st, we announced the launch of our Health Tree Research Hub and our call for myeloma research proposals during the month of March. HealthTree Research Hub is a portal where myeloma investigators can submit proposals and study anonymized data from myeloma patients. We opened this portal with the goal to accelerate myeloma cures. We want to facilitate research in faster ways, and it's because of you that this is possible. When you share your myeloma story and information in Health Tree Cure Hub, and answer survey and study questions from myeloma experts you are contributing to cures.
We now have over 14,000 myeloma patients participating in Health Tree Cure Hub with thousands of completely validated patient records. This is called real-world data. HealthTree is the only organization that has had the technology capabilities to build this data and research portal, and nothing like it exists anywhere else. HealthTree Research Hub is the companion tool for myeloma researchers who before today did not have access to complete and up-to-date data sets to use for their research.
Our goal is to complete 100 research projects from now until the end of 2025. So please tell your doctor about the March call for proposals and please join HealthTree Cure Hub and become a contributor for cures.
Not everyone can join a clinical trial, but everyone can share their data with the experts who are developing cures on our behalf.
Now onto our show. We've heard a lot lately about immunotherapies like bispecifics and CAR T therapies, but there are a significant number of additional tools in the myeloma toolbox. In the last 20 years, over 19 drugs have been approved with more on the way.
In today's show, Dr. Clifton Mo of the Dana-Farber Cancer Institute will be joining us to share how he and others are using all the myeloma tools in the Toolbox and how additional tools are in development. So Dr. Moe, welcome to the program. Thank you, Jenny. Happy to be here. Thanks for joining us.
So let me give an introduction for you before we get started. Dr. Clifton Moe is Assistant Professor of Medicine at Harvard Medical School and Senior Physician of Medical Oncology at Dana-Farber Cancer Institute. He is Director of the Autologous Stem Cell Transplantation Program for Multiple Myeloma and is Associate Director of Clinical Research at the Jerome Lippert Multiple Myeloma Center.
He is a former medical officer in the United States Army serving in Iraq and Bulgaria. So we thank you very much for your service. Incredible. In this role, he's won multiple awards, including the Associate Master Clinician Award and the Army Commendation Medal and Order of the Spur, just to name a few. Dr. Mo serves on multiple committees, including the Dana Farber Clinical Trials Advisory Board and Executive Committee of the Convalescent Plasma study.
He serves as a reviewer of major publications including Bone Marrow Transplantation, Journal of Clinical Medicine, Cancer Biology and Therapy, and Clinical Cancer Research, just to name a few. He is also co-editor of the Advances in Hematologic Malignant Disease newsletter at Harvard.
Dr. Mo is instrumental in the development of many clinical trials spanning very different myeloma drug classes. So again, welcome to the program. We probably have a lot to talk about in today's show, but we hear so much about CAR-Ts and bispecifics. I feel like everything else is getting ignored and it's important to know there are a really wide variety of treatment options available beyond those specific immunotherapies. So maybe you want to walk us through different drug classes and I'm not sure how you want to approach it, but maybe we can start with some very familiar standard of care options and then work our way down the list.
Dr. Mo: Absolutely. Thank you, Jenny, for that kind introduction. And I want to start by agreeing with you wholeheartedly that although CAR T-cell therapy and bispecific antibody therapy have very deservedly gotten the majority of the attention, in terms of discussion about recent therapeutic advances in myeloma.
The treatment advances that have been collectively made over the past two decades, as well as just over the past five plus years, encompasses much more than those two modes of therapy.
While I am just as excited as every other myeloma oncologist to talk about CARs and bispecific antibodies. I'm very excited today to talk about everything else with you. Well, there was a lot of everything else, right? I mean, absolutely. So to start things off, perhaps we should address with, we should start off by addressing what would currently be considered the quote unquote “standard therapies” for relapsed and refractory myeloma in earlier lines. I hesitate to use the word “standard” because I think that implies that there's one right answer for all patients, which I think increasingly, at least in the myeloma world, is becoming not the case. And I think increasingly there are a number of reasonable options at every bridge that a patient has to cross that all have their pros and their cons, advantages and disadvantages. And I think increasingly, need to take time with our patients, laying these pros and cons, and then make an informed decision together with the patient.
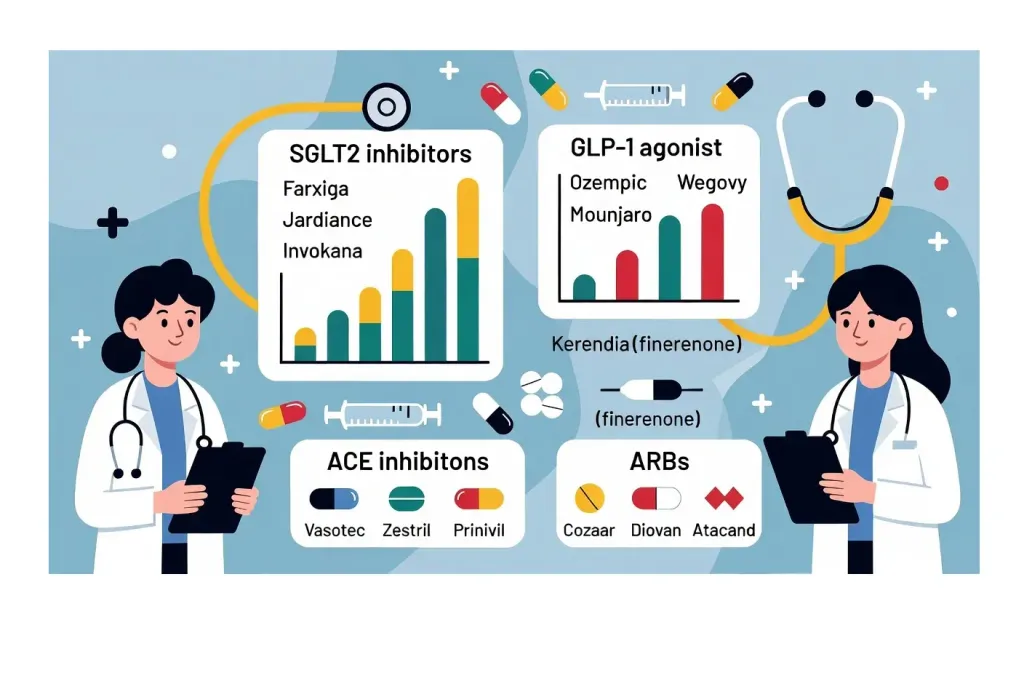
That being said, if not the standard approach, I would say the most popular or most commonly adopted approach in the second line would be a triplet regimen or a three-drug regimen that's based on number one, an anti-CD38 monoclonal antibody, and for years we had one of them, daratumumab, and now we have two of them, the more recent approval being isatuximab.
And then the second drug within that triplet regimen would usually be either an immunomodulatory or Revlimid-like drug or a proteasome inhibitor or a Velcade-like drug. And then as with most myeloma regimens, the third drug class as almost always steroids or dexamethasone specifically.
So we have a total of six of these triplet regimens from which to choose. And by that, I mean six regimens that have full approval in the United States. I'm happy to list them out quickly. So that would be a dara/Revlimid/dex, dara/Velcade/dex, dara/carfilzomib/dex, dara pomalidomide/dex and then isatoxamab/carfilzomib/dex and isatoxamab/pomalidomide/dex.
So I think most patients in the second line will still get one of those regimens. And I think they all have their, again, their advantages and disadvantages. When you compare across trials, which is something that we always caution each other not to do, and then we all go ahead and do that anyway, because in reality, what else are we supposed to do when we don't have head -to -head data to compare every single regimen. So what you do pair across trials cautiously, I do think that at least numerically, the most durable or the longest duration of responses I think are seen with the carfilzomib and the Kyprolis-based regimens. I think that's a very attractive regimen for most patients with the exception of those who either have known cardiac disease or multiple and or uncontrolled cardiac risk factors that may raise one's risk for cardio toxic complications of Kyprolis, which we all know is a very real risk, although it is still relatively uncommon and in the single digit percentage incidents in most clinical trials that we look at.
I think each triplet regimen has its own risks and possible rewards, but I think that would be the first kind of class of regimens from which to choose in earlier lines. Now, I know I just said that I'm happy to talk about everything other than CAR T -cell therapy, and now I'm immediately going to talk about CAR T -cell therapy. One of the biggest developments over the past year has been the reporting of a couple of randomized phase three clinical trials, which have pitted anti-BCMA CAR T cell therapy directly against standard of care, more classical regimens to include some of these triplet regimens. And both of those studies, KARMMA-3, looking at ide-cel and CARTITUDE-4 looking at cilta-cel, have shown significant improvement in progression free survival, with the CAR T compared with the standard of care therapy.
So on the one hand, I think these studies are very important and may or may not lead to changes in the labels of either one or both of these CAR T cell therapies, which I think I can confidently say in the myeloma community, we're all hoping for that. But at the same time, both of these trials included only some but not all of these three drug regimens in the comparator arm and arguably, you know, the ones that have the most promising efficacy numbers, the carfilzomib -based regimens, the DaraKd, IsaKd, either of those regimens were included in the comparator arms of either of those studies. So again, that's not to say that CAR T -cell therapy should not be used early, but it is to say that as with most things in myeloma, the story and the take-home point may not necessarily be as straightforward as the headlines might suggest.
Jenny: Well, there's a lot to think about, right? You're thinking about what does this person's disease look like? How aggressive is it? What do they respond to? For how long did they respond? And getting a sense of their disease status when you're thinking, did we do an early bispecific or did we do an early CAR T compared to these other treatment arms?
And I guess those are some of my question too. You listed those six different therapies combinations. How do you decide as a clinician, which one you pick for which patient? And then you mix the bispecific and CAR -T's into all of that, then you have a lot of decision -making to do.
Dr. Mo: Absolutely. There are an increasing number of permutations under the umbrella of treatment options. And I think you said it best, you have to take multiple factors into account, patient-specific factors, disease biology-specific factors, as well as the patient's previous treatment history. Which drugs have they already seen? Which drugs have they seen but aren't necessarily refractory to yet? And also, which complications and side effects have or have not been problematic for them in prior lines of treatment?
I think these all help to inform treatment decisions and should all be valued as opposed to just looking at one efficacy endpoint from one clinical trial and saying that that's the right answer for everyone. For me personally, I think it's becoming increasingly difficult, if not impossible, to sketch out a how I treat algorithm onto one page or one slide and apply it to all myeloma patients.
And it’s probably impossible for me now to do that even over two or three slides. I like to, in my mind, sketch out how I treat algorithms for each individual patient now based on all of these factors, which on the one hand may be a little bit of a cop-out answer because I can't give clear guidance from how to get from point A to point B to point C for a general group of patients. But at the same time, it's the most honest answer I could give because I think that approach gives doctors and patients, you know, the highest likelihood of a high arriving at the right answer for that specific patient at that specific moment in time.
Jenny: That means you need a myeloma specialist on your team. Period. Absolutely. These treatment decisions. It just doesn't make sense to have somebody who's treating hundreds, if not thousands of cases of multiple myeloma on an annual basis, compared to a general oncologist who's treating one, two, five, maybe cases of multiple myeloma in their clinic. The pattern recognition has just got to be so much better with you. A lot of data that's showing that's the case. You live longer.
Dr. Mo: Absolutely. So I think that for most patients, it's important to have both. It's important to have a dedicated, conscientious, communicative primary oncologist as well as a myeloma specific oncologist, at a center that may be a longer drive from the patient's home. A good primary oncologist is important for a number of reasons. Not the least of which is the fact that the majority of our myeloma therapies, still require long-term dosing strategies, anywhere from weekly to monthly injections combined with monthly refills of poorly available drugs. And a big part of one's quality of life is, for many of my patients, is being able to get the best therapies as close to home as possible. But where I come in as a consultative oncologist, helping the patient and their primary oncologist decide what locally available therapies make the most sense, from both a long -term disease control as well as a quality of life standpoint.
And that's where I think in this day and age, it would be way too much to ask of a primary general oncologist to be able to do that all by themselves because they have 97 other diseases to be knowledgeable about and to stay up-to-date about. So you're absolutely right that it's the partnership, I think, that's going to become increasingly important within the myeloma community.
We used to call it the the Tom Brady-Bill Belichick approach here in Boston, but now they both left, so I don't know what we should call them.
Jenny: Well, you just described this perfectly. You mentioned dex. So maybe this steroid has been around forever. Maybe you can talk about strategies that limit or even eliminate dexamethasone as a steroid.
Dr. Mo: Great question. So as you just said, dex has been around the longest out of all of these drugs and is the one drug in myeloma that isn't classified as a myeloma specific or novel agent therapy. And yet it is arguably the one that still causes the most problems in terms of side effects.
So I think the first important point is that while dex is an integral component of these regimens, and I do believe it's important, I think having it on board in general is much more important than being on or staying on the full dose. I've heard it referred to by colleagues as the WD-40 of one's regimen. So as long as you spray enough on to grease the wheels, you don't necessarily need to throw the whole can at it. And I think that's largely true in the landmark study by Vincent Rajkumar at Mayo Clinic of low dose dex, which is what nowadays, we refer to as dex which is 40 milligrams once weekly, as opposed to high dose dex, which is what actually used to be given commonly to patients of 40 milligrams for four consecutive days, and then repeating that pulse at regular intervals. There was actually a survival advantage seen in the low dose arm. It wasn't just a matter of less side effects.
It was a statistically significant OS advantage due to significantly lower rates of toxic events happening to patients on the low dose arm. It's not the only example, but I think it's a very important example of more not always being better. I do tend to have a very low threshold to reduce the dose of dexamethasone after initial disease control has been established, which with our modern day regimens, you know, can be as early as a month or two after you start the regimen. And then to essentially titrate the dose of dexamethasone to what is tolerable and, you know, quality of life improving for the patient. So sometimes that lands at 20 milligrams weekly, sometimes it lands at less. And sometimes I do, you know, transition from...
once weekly dexamethasone to less frequent dosing if reductions in the dose alone as opposed to the frequency don't necessarily do the trick in terms of making the drug more tolerable from a sleep, fluid retention, anxiety or standpoint. I still remember a patient who walked into my office and said, I just gave a nasty gesture to someone on the highway and I don't ever do that. What's wrong with me? And said, we might want to cut your dex.
Jenny: You call it the WD-40 and patients call it the drug that makes everyone else stupid. They want to get off.
Dr. Mo: Both probably true.
Jenny: As fast as they can.
It's interesting to see these immunotherapies come out not using dexamethasone in some of the lines.
Dr. Mo: Perhaps that helps in those kinds of therapies not only with the side effects and quality of life, but it actually would help with efficacy because these newer immune therapies lie on T cell function and that's one thing that steroids are known to do is to somewhat suppress that function.
Jenny: Okay, let's talk about the others. Antibody drug conjugates, I think there was an announcement even today about some of the BLENREP data that's coming out. So maybe you want to explain what antibody drug conjugates are and how they work.
Dr. Mo: Sure. Antibody drug conjugates or ADCs as they're known by shorthand are a form of therapy that involves direct delivery of an active myeloma drug to the myeloma cell via monoclonal antibody binding to that cell. Until very recently, when we've talked about monoclonal antibodies in myeloma, we've been talking about daratumumab and less frequently about elotuzumab, which I can talk about later. But these are essentially naked antibodies, meaning that they're immune proteins that will latch on to the surface of the myeloma cell by recognizing a protein on that cell. And in and of themselves, that's all the antibodies do. But that triggers components of the immune system to directly attack the myeloma like the immune system would ordinarily fight off an infection.
So that's what monoclonal antibody immunotherapy is. With an ADC, you have an antibody, a monoclonal antibody that latches onto the myeloma cell, but linked to that antibody is a core payload or an active drug. And in the case of belantamab mafodotin, it's a classic chemotherapy drug called MMAF, which disrupts the architecture of the cell and when the payload is attached to the antibody, it is inactive. What happens when the antibody binds to the cell is it essentially tricks the myeloma cell into engulfing or swallowing the drug and then once the ADC is inside the myeloma cell, the payload will essentially cleave away from the antibody and into its active form and destroy the myeloma cell from the inside out.
It's referred to as the Trojan Horse approach to chemotherapy. So a classic chemotherapy drug that's not just delivered into somebody, into a patient's vein is more or less like a, and I'm sorry to use the military analogies, but like a smart missile where it's directly transported into the myeloma cell specifically for maximal efficacy. So in a nutshell, that's what an ADC is. And in myeloma now, we have one ADC called belantamab mafodotin or BLENREP that has had an interesting story over the past few years. The first part of that story was a positive chapter, and that was an accelerated approval by the FDA of BLENREP for patients with relapsed refractory myeloma and four prior lines of treatment. And that approval was based on the DREAMM-2 study and found just shy of a 30% response rate, which again is not a wonderful batting average.
Jenny: It’s pretty normal, though.
Dr. Mo: But the setting of heavily pretreated disease is nothing to dismiss and in responders, the average duration of response was about a year, which again was pretty good. So we were all able to use commercially available BLENREP for a short period of time. And what happened next was the DREAM-3 study results were released and this was supposed to be the confirmatory phase 3 study to lead to full FDA approval. And the design of the study was essentially pitting BLENREP directly against pomalidomide plus dexamethasone in patients with relapsed refractory disease. But interestingly, this study failed to meet its primary endpoint of superior progression-free survival. More than that, the hazard ratio for overall survival was just a little bit north of one, which gave the FDA a bit of pause in terms of whether these numbers were sufficient to warrant a full approval.
And in fact, instead of a full approval, what happened was a withdrawal of the approval based on the failure of DREAMM-3 to demonstrate superiority. And the hazard ratio of one, maybe you can explain like that means that both sides are the same kind of, right?
Dr. Mo: (A hazard ratio of 1) that means that there is no detectable increase or decrease risk of progression or death between both arms, between either arm of the study, a wash essentially.
We became unable to do so outside the context of a clinical trial, which brings us essentially to today when we now have two reported phase three trials of BlendRep, this time looking not at BlendRep by itself, but as a component of a triplet regimen.
We have reported and now published results from DREAMM-7, which pitted BLENREP, Velcade and dexamethasone or BVD against daratumumab, Velcade, and dexamethasone or DVD. And in that study, we see a clear advantage in favor of the BLENREP arm in terms of progression-free survival with essentially a tripling of median PFS compared to the DVD arm.
And also in a pretty early and relatively immature overall survival analysis, there does appear to be a trend in favor of BVD, not just in terms of progression-free interval, but in terms of overall survival (OS) as well. So I think it's going to be really interesting to see how the FDA digests and reacts to those data. I think are pretty impressive data that at least historically would be enough to lead to a full approval.
And now we have a very early, very recently report of the DREAMM-8 data, which was similar to DREAMM-7. Instead of comparing a BLENREP or evaluating BLENREP against daratumumab, this evaluated BLENREP against Velcade. And it appears to be a similar story with a significant improvement in progression-free survival.
So a very short period of time, we've gone from accelerated approval to phase three trial failure to drug withdrawal, and now to what appears to be two phase three combination trial successes.
Jenny: Comeback.
Dr. Mo: So could BLENREP be the comeback kid over the next year? I think it's entirely possible. And clearly with BlendRep, either by itself or as a part of a triplet regimen results in significantly more ocular toxicity than our other drugs due to keratopathy or the formation of these very tiny microcysts within the corneal layer of the eye, which I think we still incompletely understand why that happens, but we know that it happens commonly and it's very unique within the, in the myeloma world, it's very unique.
Now the majority of these events are low grade.
Jenny: Yes, this is like vision, blurriness and dry eye.
Dr. Mo: Exactly. The most common complaint is blurry vision. Then, dry eye is probably number two and certainly this drug has the potential to cause clinically significant eye side effects, even after only a couple of doses of the drug. That being said as with most other drugs in myeloma, as we gain more experience with it, I think we are increasingly able to avoid severe toxicities, both by regular eye exams, as well as by adopting a lower threshold to hold additional doses in the setting of low grade. There are other strategies being looked at, lower dosing, less frequent doses amongst others.
So I don't think it's going to result in a situation where this drug is going to be irrevocably looked at as an eye toxic drug for which the risks outweigh the benefit. I think especially in light of these new phase three trial data, I think all of us myeloma oncologists need to take a second look at BLENREP and really start to figure out how best to incorporate this drug into a patient's myeloma journey, assuming that we will be allowed to give it in the near future, which again is an assumption and not necessarily a prediction.
Jenny: Interesting to see because I know some of those side effects are reversible. And like what you said, you can dose reduce, you can spread the doses out. And just as a BCMA therapy, this is an off-the-shelf thing compared to a CAR T.
Bispecifics are also off the shelf and you have a lot of those coming out.
Dr. Mo: Exactly.
Jenny: So, but those come with infections. And so like, it'll be really interesting to see how this all plays out. It'll just depend maybe on the patient, how they respond to it or how they don't respond to it or the level of different side effects with these different BCMA targeted therapies.
Dr. Mo: Yes. I tend to joke with my patients that in myeloma, there's always a,”but” right? It's a pretty remarkably well tolerated gentle drug when you're not considering the eye toxicity. As you just mentioned, it's not a T-cell redirecting, BCMA directed therapy. We don't see cytokine release syndrome, we don't see neurotoxicity. There's no requirement for inpatient step-up dosing. So again, other than the eye toxicity, this drug has a lot going for it. Something I do want to mention is that we do see that the responses can be relatively durable even when the patient has to stop treatment for the eye toxicity. I have one patient I'm thinking of right now who got maybe three or four doses of BLENREP. We stopped the drug and then I think it took maybe 10 months for her kappa light chain level to even start to rise again from normal.
Sometimes the benefits can significantly outlast the duration of the eye toxicity and can hold up for a meaningful amount of time, even when you do have to stop the treatment.
Jenny: Well, we have a lot to talk about still. There's a lot going on in myeloma. BCL2 inhibitors, do you just want to touch on that, like in terms of a genetic approach?
Dr. Mo: Great question. So BCL2, is what we call an anti-apoptotic protein. It essentially prevents cancer cells that ordinarily should auto-destruct and die. It gives them some degree of immortality and prevents that from happening. And direct inhibitors of this BCL2 protein have been approved for chronic lymphocytic leukemia, as well as more recently, acute myeloid leukemia.
In those malignancies, the clinical trial data have been very impressive and have essentially transformed the standard of care for these kinds of diagnoses. We were hoping that it would be a similar story in myeloma, and there was reason to hope based on earlier phase studies. However, then along came the phase three Bellini study, which didn't work out the way we were hoping in the sense of the study being put on hold and stopped because of a signal for increased risk of death in the venetoclax arm of the study. This study was comparing the venetoclax plus Velcade and dexamethasone versus Velcade dex alone and there was a signal for a mortality risk with the addition of venetoclax, which is of course the very last thing that you want to see in that kind of trial.
Following that hold, an important subgroup analysis was done showing that the concerning events were being seen in patients without the t(11;14) translocation and in patients with low Bcl2 expression in their myeloma cells.
In patients who did have the t(11;14) translocation, which we also refer to as the cyclin D1 IGH gene rearrangement, seen in about 15% of patients with myeloma. In people who were positive for t(11;14), we didn't see that signal. And in fact, we saw patients responding very well with the hazard ratio for PFS (progression free survival).
Again, the lower the ratio, the better in favor of the investigation alarm, the hazard ratio being 0 .1 in favor of the venetoclax arm of the study. That really taught us a lesson that from a biological standpoint, there truly are multiple myelomas within the diagnosis of multiple myeloma. And that one drug that could be bad, for one patient may be great for another based on differences in disease biology and driver mutations. So after the initial fallout of Bellini, the FDA allowed resumption of venetoclax studies in myeloma, but restricted the studies to patients with t(11;14).
In combination studies, recently presented study of t(11;14) venetoclax, dara, dex versus dara venetoclax, dex, the efficacy numbers looked to favor the venetoclax arm of that study. However, we were all really waiting until last year, we were all really waiting on the results of the phase three CANOVA study, which compared venetoclax, dex versus pomalidomide, dex. And unfortunately, the study failed to reach the primary endpoints of a PFS advantage in favor of the venetoclax arm.
Now when you look at that study, pretty much every efficacy metric that there is, trended in favor of venetoclax, but it just did not reach statistical significance. Does Canova tell us that venetoclax dex is no better than pomalidomide/dex? Perhaps there are issues with adequate powering of the study. Unfortunately, the horizon is looking a bit dimmer for venetoclax now.
in terms of likelihood of FDA approval. That being said, even without an approval for myeloma, I still feel comfortable treating patients with off-label venetoclax-based regimens when they have the 11;14 translocation, and I will continue to offer them as options to this subpopulation of patients when I think it's appropriate, when the patient is comfortable receiving such therapy. And of course, when their insurance company is also willing to support that decision.
Jenny: I hear that from a lot of myeloma doctors, they still need to be providing this to patients.
Dr. Mo: I’ll briefly mention that there are some next generation BCL2 inhibitors that are under study right now. One particular in myeloma that we now have early efficacy data for that looks pretty promising. Venetoclax, at the end of the day, if venetoclax is not destined to be approved for myeloma, I think we're still hopeful that perhaps a next generation BCL two inhibitor may have better luck.
Jenny: Right. Good to know. We have two more things to talk about. Then I have other questions as well. So celmods are new up and coming therapy. I think we should probably talk about that.
Dr. Mo: So the celmods are very similar in how they work to Revlimid and Pomalyst and that they bind to cereblon in the myeloma cell, which then allows proteins that are crucial for myeloma cell survival to be tagged for degradation by the waste disposal system of the cell.
However, they are much more potent in terms of how they bind to cereblon, which leads to significant improvement in the ability to directly kill the myeloma cells through that binding, and also seems to result in greater stimulation of important immune cells that can then help to further attack the myeloma. This improvement in potency and tightness of binding is not a coincidence.
These drugs were designed with their specific mechanism in mind, as opposed to Revlimid, which we were all using to treat patients, we were all using in myeloma for years, even before we figured out how the drug actually worked.
Ben Ebert, who is now our chief of medical oncology at Dana-Farber, he and his colleagues in the lab actually identified how Revlimid works - cereblon binding process, which results in degradation of Icaros and Iolos, these important nuclear transcription factors. And he presented those data close to a decade after Revlimid was actually FDA approved for myeloma. These drugs, they have been designed to maximally exert their mechanism of action against the myeloma cell.
To put it very bluntly, I think these drugs are on their way, and I think they will hopefully supplant Revlimid and perhaps even Pomalyst in the not-too-distant future. What we know now is that they are very active as single agents or in combination with dexamethasone in heavily pretreated relapse refractory myeloma patients, just under a 30% response rate of iberdomide plus dex in patients with median five prior lines of treatment and just over a 40% response rate of mezigdomide plus dex in a triple class refractory myeloma patient population.
Both of these drugs appear to partner well with other bread and butter myeloma drugs such as daratumumab. And importantly, they also appear to be very well tolerated. We definitely see cytopenia, most notably neutropenia, with both of these cell mods. But I do believe that we are seeing less of the non-hematologic toxicities that we see with Revlimid to include rash, diarrhea, fatigue. So these are so far looking like cleaner upgrades from the currently available IMiDs (immunomodulators). So I have a lot of optimism about this drug class.
Selinaxor is a first in class drug that has been approved for patients with relapsed refractory myeloma for about, for just under five years now. It first received accelerated approval in 2019 for heavily pretreated or penta-refractory myeloma patients in combination with dexamethasone.
That regimen was clearly an active regimen with some impressive responses seen, but the problem back then was in terms of tolerability. In the initial approval, the dose of selinexor was 80 milligrams by mouth twice weekly. And with that dose, a lot of patients had considerable difficulty with fatigue and nausea as well as with low blood cell counts. Since then, the drug has gotten full FDA approval in patients with at least one prior line of therapy in combination with Velcade and dexamethasone. I think the most important take home point from the BOSTON study is that when the frequency of the selinexor was dropped to once weekly, the rate of high grade toxicities, both hematologic and non-hematologic, dropped considerably and it became a significantly more tolerable regimen.
Also notably on that study, the subgroup analysis seemed to indicate that patients who have the 17P deletion, also known as a TP53 deletion, the hazard ratio…
Jenny: A high-risk feature, right?
Dr. Mo: Yes, high-risk feature. The hazard ratio was about, I believe, 0 .3, which again is a pretty suggestive evidence that this may be a particularly active drug in patients with that mutation, which when you think about it makes total sense in terms of how the drug works. It's what's called a selective inhibitor of nuclear export or a SINE, S -I -N -E. And essentially what that means is there is a protein on the myeloma cell that essentially shuttles tumor suppressor proteins, which are good proteins, out of the nucleus of the cell where they exert a suppressive effect on cancer cell proliferation. They shuttle those good proteins out of the nucleus into the cytoplasm where they can't do their job.
And they also shuttle bad, what we call oncogenic mRNA, into the cytoplasm where the mRNA can be used as a code to create oncoproteins, or bad proteins. So essentially it's the myeloma cell’s way of kicking good proteins out of their home and increasing delivery of bad proteins, or increasing the ability for the cell to create bad proteins.
And selinexor essentially shuts off the function of that shuttling protein, which results in nuclear retention of these proteins. An analogy that sometimes is used is it's like a group of teenagers that throw a house party when their parents go on vacation.
Jenny: I have one of those teenagers.
Dr. Mo: Exactly. And then this drug essentially brings the parents home to get things back in order. So it's now fully approved in combination with Velcade-dex for myeloma. We also have efficacy and safety data from phase two studies in combination with pomalidomide and daratumumab as well as carfilzomib.
And across the board, we see that, this is an active drug in all of these combinations, again, with improved tolerability with once weekly dosing, which is not to say that there aren't patients who still have difficulty tolerating it with once weekly dosing because there are. But interestingly, there was an analysis done of all the patients treated to date in the clinical trials of using seli/pom/dex (selinexor plus pomalidomide and dex).
The two doses were looked at, 40 milligrams once weekly and 60 milligrams once weekly. And what that analysis showed was that although the response rate was higher in patients who got the 60 milligram dose, the progression free survival was longer in patients who got the 40 milligram dose. Wow, that's unusual. So again, another example of more not always being better, sometimes less being more. You know, unfortunately, because of the initial STORM study, which led to the accelerated approval, selinexor did quickly get a reputation as being a difficult-to-tolerate drug, which was a fair criticism. But again, I think that it is very premature, especially given what we know about the activity of this drug in myeloma and particularly in high risk disease. I think it's very premature to give the drug that label and to give up on it when we're seeing very encouraging data in terms of not only efficacy, but tolerability with lower less frequent dosing strategies.
Jenny: Well, this just goes to show that there's so much that you still have to learn once something gets approved and how it's being used in the clinic, what the real side effects are. Can you lower the dose? Can you space the doses out? Like all of that practical life experience that you're seeing in the clinic is really informing these future trials.
Dr. Mo: So along those lines, we are going to be studying low dose selinexor in combination with mezigdomide in an upcoming study with support from both Karyopharm and BMS. So I think that it of course remains to be seen how active and how tolerable this combination will be. But I'm very hopeful given everything that we've learned about selinexor that I just mentioned, as well as given the very promising data we're seeing from the mezigdomide studies to date. I think this combination has a number of potential advantages.
Number one, it's all oral therapy, which again, not for every patient, but for some patients, can be as ideal and very attractive to be able to take their pills at home and not necessarily be tied to an infusion clinic that they have to go to once a week.
And also in terms of access, there are patients who have issues with transportation or who live in rural or semi-rural communities. When get to their primary oncologist, they may have to drive for hours. And for that reason, I think oral therapies can be very advantageous.
Also, you know, thinking about the CAR T cell therapies and the bispecific antibody therapies, clearly these are highly efficacious, very attractive treatments. I'm so happy that we've gone from zero to five FDA approvals in the past few years. But that being said, I think we have to temper our excitement with a certain degree of humility in the sense that, this is still largely an incurable disease, right?
And we to see a curative signal from the CAR-Ts or the bispecifics. Yeah, we were all hoping. Yeah, not to get too off topic, but who knows, first line. Or other things after. But at least right now, I think we have to recognize that none of the treatments we have available right now have curative potential. And especially with the bispecific antibodies, one of the reasons that they may ultimately stop working is because of T cell exhaustion. Essentially every time you get an injection of a bispecific, you're kind of asking your T cells to run a 400 meter sprint and activate and kill the myeloma. And we clearly see markers of T cell exhaustion as patients go months and years into these kinds of therapies. And that may have implications not just in terms of loss of efficacy, but perhaps in terms of infection risk. One could hypothesize that giving a T cell redirecting therapy in the immediate setting of T cell redirecting therapy failure may not be a patient's best option.
And therapies that don't exhaust T cells. So again, game changing, as game changing and as the CARs and bispecifics have been and continue to be, I think we still need to look at myeloma therapy from a strategic standpoint and ask ourselves, can we improve on our ability to control a patient's disease independent of T cell function?
And I think that potentially could be where these orally available drugs I've just described could fit in. We actually do have preclinical data for both selinexor and for mezigdomide that they may actually lessen T cell exhaustion.
Jenny: Oh, so interesting.
Dr. Mo: The data was actually presented at ASH last year. And again, that's not to definitively say that giving either one of these drugs or both of them in combination will actually do that in a patient to then let them get a T-cell redirecting therapy that works very well on the next line. I think it's possible or it's conceivable that such an approach might actually work.
I don't think we should look at these drugs themselves necessarily as competitors with the T cell redirecting therapy, but I think it's important to see, it's important to study whether or not they could actually be potentially partners. And by that, I mean, can you give a bispecific potentially with a low dose of a celmod and have that ultimately work much better? Or if not direct partners, could they be allies? Could you sequence one therapy after another and attack things that way.
I think that's why I'm very excited to study this combination.
Jenny: That’s fantastic.
Dr. Mo: Which I will give us even better non-CAR and non-bispecific options to not necessarily be used in lieu of CARs and bispecifics, but to really provide support for these therapies.
Jenny: We have a question from Renee who wrote in, “please explain the role and or advantages of stem cell transplant in the light of these newer therapies.”
Dr. Mo: It’s a great question and unfortunately not an easy one to answer directly. What I can say is that is that high dose melphalan with autologous stem cell transplant remains a standard of care and certainly a treatment to seriously consider in early lines of therapy because of its long-term track record over decades of improving longevity in the pre-novel agent era, as well as continuing to improve duration of remission in the triplet novel agent era.
What makes things less clear is the fact that in both IFM 2009 and DETERMINATION studies, which were both RVD with or without early transplant studies, the overall survival curves continue to look completely superimposed, which is not to say that transplant does not help some patients live longer in the long run, but it's just becoming increasingly difficult to prove that in a clinical trial.
I can no longer look my patients in the eye and say, you absolutely have to get a transplant in first remission because it's clearly going to help you live longer because I don't think that I can confidently say that anymore, which again is not to say that it's the wrong option.
It's just to say that it's the more intensive option that clearly will come with increased short-term toxicities, a very small risk of fatal complications as long as the patient is healthy enough, and may provide the patient with a significantly longer duration of disease control than were they not to get an early transplant.
But I think increasingly it's becoming a very reasonable option for transplant-eligible patients, to defer early transplant, but still have their stem cells collected and stored so they can retain the option of a stem cell transplant in second remission or perhaps even in later lines.
Now, I think, Jenny, if you'd asked me that question 10 years ago or maybe even five years ago, I think it would have been a shorter answer and that answer would have been, think very strongly consider transplanted first remission and if you pass on that, consider even more strongly a transplant in second remission. Right?
In light of all of these newer therapies that are already here and the other ones that are on the way, do I think it's completely wrong or absolutely crazy for a patient to continue to defer transplant even after first relapse? Most of us, myeloma doctors, myself included, are not yet to the point.
Where we can in good conscience suggest to a transplant-eligible patient that they let that ship sail entirely. Meaning that I still think it makes all the sense in the world to me to do an early stem cell collection at the very least and to have a comprehensive sit down discussion with their primary and oncologist and myeloma specialist, at each subsequent bridge that they have to cross for that team to make the most informed decision that's best for that individual, together.
Jenny: You don't have the data yet. So, okay, another caller question that's from Wendy. And I know you can't answer specific patient questions because you don't have the full context of their situation. But for somebody who's relapsing early after first line of therapy and has higher risk disease, you said the six combinations that you would think about at first relapse, but they were wanting to know between like isatuximab/Kyprolis and dex versus like a dara/Revlimid and dex. How would you look at those things for the higher risk patient who has not had transplants?
Dr. Mo: Great question. Again, I do think that the Kyprolis-based triplet regimens generally look pretty attractive from an efficacy standpoint compared to Revlimid or Pomalyst-based triplets.
That being said, that statement is derived from cross trial comparisons, which are educated guesses at best. And also, I think it's important to have a healthy respect for the potential for cardiovascular complications of Kyprolis based therapies. So in someone who has known coronary artery disease, history of heart failure, or perhaps uncontrolled high blood pressure or multiple cardiac risk factors. You know, I generally would be more hesitant to make a strong recommendation for a Kyprolis-based triplet.
But if that is not a prohibitive factor, that is usually my standard of care go-to. I should mention that quad therapy has been and is being looked at in clinical trials here in Boston.
We've looked at both dara/Kyprolis/pom/dex as well as elotuzumab/pom/Velcade/dex and are seeing some pretty encouraging results. That's still considered a non-standard approach, but we are seeing some encouraging efficacy data with fairly reassuring safety profiles looking at quad therapy. So for a patient who is high risk, who’s say not yet refractory to daratumumab, I would give at least some consideration for a careful quad type of approach in the second line if I'm not limited by insurance rejection.
Jenny: And last question, Lynn was asking, stem cell transplant is not a prerequisite for CAR -T, correct?
Dr. Mo: It is not. So as of today, the prerequisite is the four prior lines of therapy. Right. And in terms of what the labels will look like in another year or another month. We don't know, but I'm personally hoping for a label change that will allow CAR T cell therapy to be used much earlier and potentially to even be used prior to stem cell transplant. But admittedly, that last statement I think is probably still a controversial one to make.
Jenny: You need to see a little more data, don't you?
Dr. Mo: And we will see head-to-head data in the not too distant future in terms of CAR T cell versus high dose melphalan, specifically the CARTITUDE-6 trial, which is ongoing, is trying to answer that specific question.
There are other studies looking at transplant versus bispecific therapy. One in particular I'm very excited about coming out of Dana-Farber in the hopefully near future, which I'd be happy to talk about more with you perhaps a little bit later. So I think we will start to get more answers to these important questions. But right now we're left with an increasing number of options and not a lot of definitive answers in terms of optimal sequence. On the one hand, I know it can be very confusing and frustrating for a patient as well as for a physician. But on the other hand, this is all a direct result of things getting much better in a very short period of time. And ultimately, I think that's a great thing.
Jenny: It’s fantastic. Well, Dr. Mo, thank you so much for taking time to talk to us. You can see the breadth of what we have to work with, and it's really incredible. The innovation is totally stunning. And to have investigators like you working through all these issues in clinical trials is completely amazing. So thank you for everything that you're doing for us.
Dr. Mo: It's totally my pleasure and speaking for my whole myeloma group here at Dana-Farber, you know, we are hard at work. We're very happy about all the advances that have been made, but we all know that we still have a lot of work left to do and we're, we're doing our best.
Jenny: Thanks for listening to HealthTree Podcast for Multiple Myeloma. Join us next time to learn more about what's happening in myeloma research and what it means for you.
Trending Articles
Have Any Questions?
Thank you for your interest in the event. If you have any questions, we would love to help!
Feel free to give us a call or send us a message below.

Get In Touch With Us
1-800-709-1113
Support@healthtree.org
Get the Latest Blood Cancer Updates, Delivered to You.
By subscribing to the HealthTree newsletter, you'll receive the latest research, treatment updates, and expert insights to help you navigate your health.
Together we care.
Together we cure.