The Use of Bispecifics and CAR-T in Myeloma Treatment
In this interview, Aimaz Afrough, MD from the UT Southwestern Harold C. Simmons Comprehensive Cancer Center, discusses advancing bispecifics in myeloma treatment. Currently, bispecifics are approved as a 5th line of treatment. This requires patients to have failed their first 4 treatment attempts.
The Goal
Dr. Afrough and her team are trying to bring bispecifics to first-line treatments. They are hoping to offer this treatment after the initial diagnosis. The goal is to offer this option even when the patient’s overall health and T cells are healthy so that a deeper response can be achieved and remission can last longer. CAR-T trials are also being conducted to achieve the same remission results.
What Are Bispecifics?
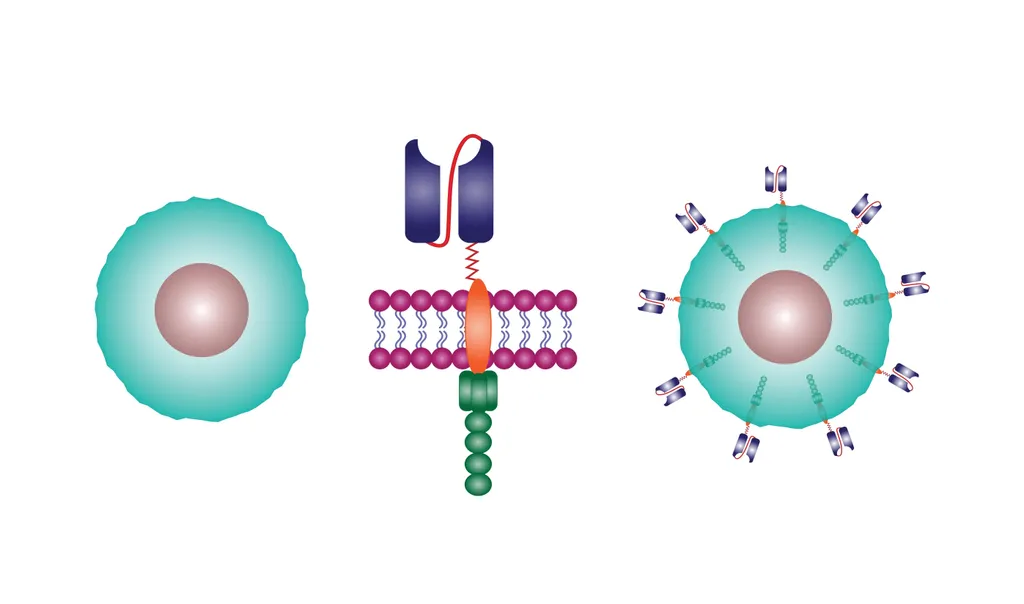
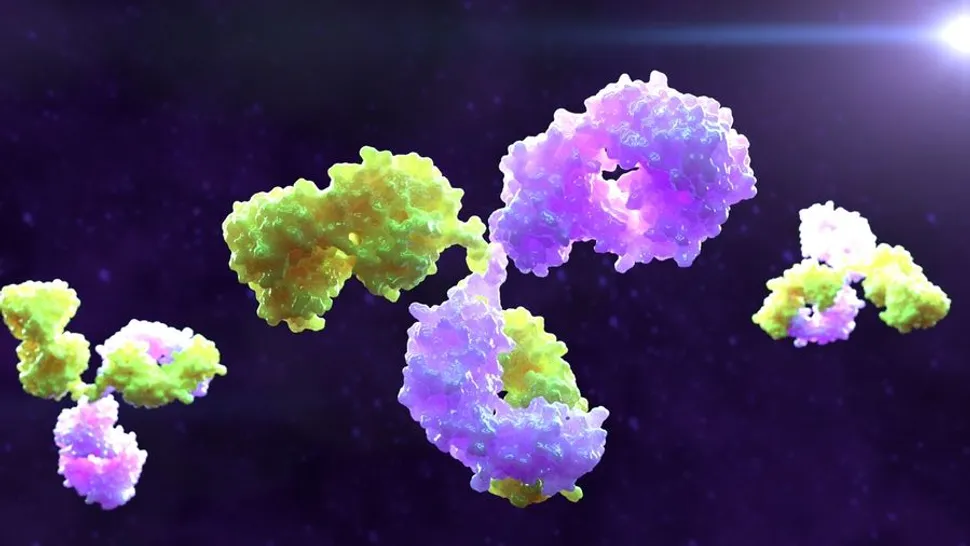
Bispecific antibodies, also known as 'bispecifics' or BsAbs, are a new generation of immunotherapy drugs showing promise in treating multiple myeloma. Unlike traditional antibodies that bind to a single target, bispecifics boast a unique "dual attack". Imagine a bridge connecting two targets: one arm of the BsAb acts like a bridge, attaching specifically to a protein found on the surface of myeloma cells; the other arm binds to immune system fighters called T cells or natural killer (NK) cells. By acting as a bridge, the BsAb essentially brings the immune cells right to the doorstep of the myeloma cells. This targeted approach allows the immune system to recognize and destroy myeloma cells more effectively.
Bispecifics are effective for relapsed/refractory or high-risk myeloma. They may also be helpful for patients who do not qualify for CAR-T treatment. They are administered in a ‘step-up’ plan and are given on a continued basis.
Learn more about bispecific antibodies from myeloma experts:
- A HealthTree Podcast: Navigating Bispecific Antibodies in Myeloma Care with Alfred Garfall, MD and Bea Razzo
What is CAR-T Therapy?
CAR T-cell therapy is a revolutionary approach to cancer treatment that harnesses the power of your own immune system. Imagine your immune system as an army trained to fight off invaders. Cancer cells, however, can sometimes develop ways to evade this army's detection. CAR T-cell therapy acts like a retraining program for your immune system's soldiers (T cells), empowering them to recognize and destroy cancer cells.
The process involves:
- T cell extraction: A sample of your T cells is collected through a simple blood draw.
- Engineering the T cells: In a specialized lab, scientists modify these T cells by equipping them with a special tool called a chimeric antigen receptor (CAR) specifically designed to recognize and target your cancer cells.
- Reinfusion: The modified T cells, now CAR-T cells, are then reintroduced back into your body through an intravenous (IV) line.
CAR T-cell therapy is currently FDA-approved for patients with relapsed or refractory multiple myeloma, meaning the disease has either come back after previous treatments or hasn't responded well to them.
Read more about CAR-T for multiple myeloma:
- My CAR-T Therapy Experience: A Myeloma Patient Story
- Myeloma CAR-T Achieves 100% Response Rate in High-Risk Patients
- Physicians Take On CAR-T Therapy Secondary Cancer Risks
Check the open clinical trials looking for participants in your area with our Clinical Trial Finder
CREATE A FREE HEALTHTREE CURE HUB ACCOUNT
In this interview, Aimaz Afrough, MD from the UT Southwestern Harold C. Simmons Comprehensive Cancer Center, discusses advancing bispecifics in myeloma treatment. Currently, bispecifics are approved as a 5th line of treatment. This requires patients to have failed their first 4 treatment attempts.
The Goal
Dr. Afrough and her team are trying to bring bispecifics to first-line treatments. They are hoping to offer this treatment after the initial diagnosis. The goal is to offer this option even when the patient’s overall health and T cells are healthy so that a deeper response can be achieved and remission can last longer. CAR-T trials are also being conducted to achieve the same remission results.
What Are Bispecifics?
Bispecific antibodies, also known as 'bispecifics' or BsAbs, are a new generation of immunotherapy drugs showing promise in treating multiple myeloma. Unlike traditional antibodies that bind to a single target, bispecifics boast a unique "dual attack". Imagine a bridge connecting two targets: one arm of the BsAb acts like a bridge, attaching specifically to a protein found on the surface of myeloma cells; the other arm binds to immune system fighters called T cells or natural killer (NK) cells. By acting as a bridge, the BsAb essentially brings the immune cells right to the doorstep of the myeloma cells. This targeted approach allows the immune system to recognize and destroy myeloma cells more effectively.
Bispecifics are effective for relapsed/refractory or high-risk myeloma. They may also be helpful for patients who do not qualify for CAR-T treatment. They are administered in a ‘step-up’ plan and are given on a continued basis.
Learn more about bispecific antibodies from myeloma experts:
- A HealthTree Podcast: Navigating Bispecific Antibodies in Myeloma Care with Alfred Garfall, MD and Bea Razzo
What is CAR-T Therapy?
CAR T-cell therapy is a revolutionary approach to cancer treatment that harnesses the power of your own immune system. Imagine your immune system as an army trained to fight off invaders. Cancer cells, however, can sometimes develop ways to evade this army's detection. CAR T-cell therapy acts like a retraining program for your immune system's soldiers (T cells), empowering them to recognize and destroy cancer cells.
The process involves:
- T cell extraction: A sample of your T cells is collected through a simple blood draw.
- Engineering the T cells: In a specialized lab, scientists modify these T cells by equipping them with a special tool called a chimeric antigen receptor (CAR) specifically designed to recognize and target your cancer cells.
- Reinfusion: The modified T cells, now CAR-T cells, are then reintroduced back into your body through an intravenous (IV) line.
CAR T-cell therapy is currently FDA-approved for patients with relapsed or refractory multiple myeloma, meaning the disease has either come back after previous treatments or hasn't responded well to them.
Read more about CAR-T for multiple myeloma:
- My CAR-T Therapy Experience: A Myeloma Patient Story
- Myeloma CAR-T Achieves 100% Response Rate in High-Risk Patients
- Physicians Take On CAR-T Therapy Secondary Cancer Risks
Check the open clinical trials looking for participants in your area with our Clinical Trial Finder
CREATE A FREE HEALTHTREE CURE HUB ACCOUNT

about the author
Lisa Foster
Lisa Foster is a mom of 3 daughters and 1 perfect grandchild, a puzzle lover, writer and HealthTree advocate. She believes in the mission of the foundation and the team that builds it forward. She calls Houston, Texas home.
More on Clinical Trials
Get the latest thought leadership on your Blood Cancer delivered straight to your inbox
Subscribe to the weekly newsletter for news, stories, clinical trial updates, and helpful resources and events with cancer experts.