
It's been said that if you ask three multiple myeloma specialists a question, you'll receive six answers. While this can be true, the Beyond the Guidelines: Clinical Investigator Perspectives on the Management of Multiple Myeloma session moderated by Neil Love, MD of RTP (Research to Practice) revealed that when it comes to providing concise answers for important myeloma decisions, most specialists tended to agree with one another.
Let's look more into these questions and decisions below.
Dr. Neil Love asked twenty myeloma specialists to participate in a survey regarding myeloma treatment decisions in preparation for this event. The twenty myeloma specialists who responded to Dr. Love's survey were:
- Melissa Alsina, MD
- Jesús Berdeja, MD
- Natalie Callander, MD
- Rafael Fonseca, MD
- Carol Ann Huff, MD
- Jonathan Kaufman, MD
- Amrita Krishnan, MD
- Shaji Kumar, MD
- Ola Landgren, MD, PhD
- Sagar Lonial, MD
- Tom Martin, MD
- Joseph Mikhael, MD, MEd
- Philippe Moreau, MD
- Robert Orlowski, MD, PhD
- Krina Patel, MD, MSc
- Noopur Raje, MD
- Paul Richardson, MD
- Keith Stewart, MB, ChB
- Sascha Tuchman, MD, MHS
- Jeffrey Zonder, MD
Before we get started, please remember that none of the information presented below should be taken as personal medical advice, but rather serve as a resource support to discuss with your doctor and treating medical team.
What is your preferred induction regimen for a younger 65-year-old patient with standard-risk multiple myeloma?
This question was asked to the 20 specialists, who were asked to put regulatory and reimbursement issues aside. The responses were actually quite similar considering how many specialists were asked the question.
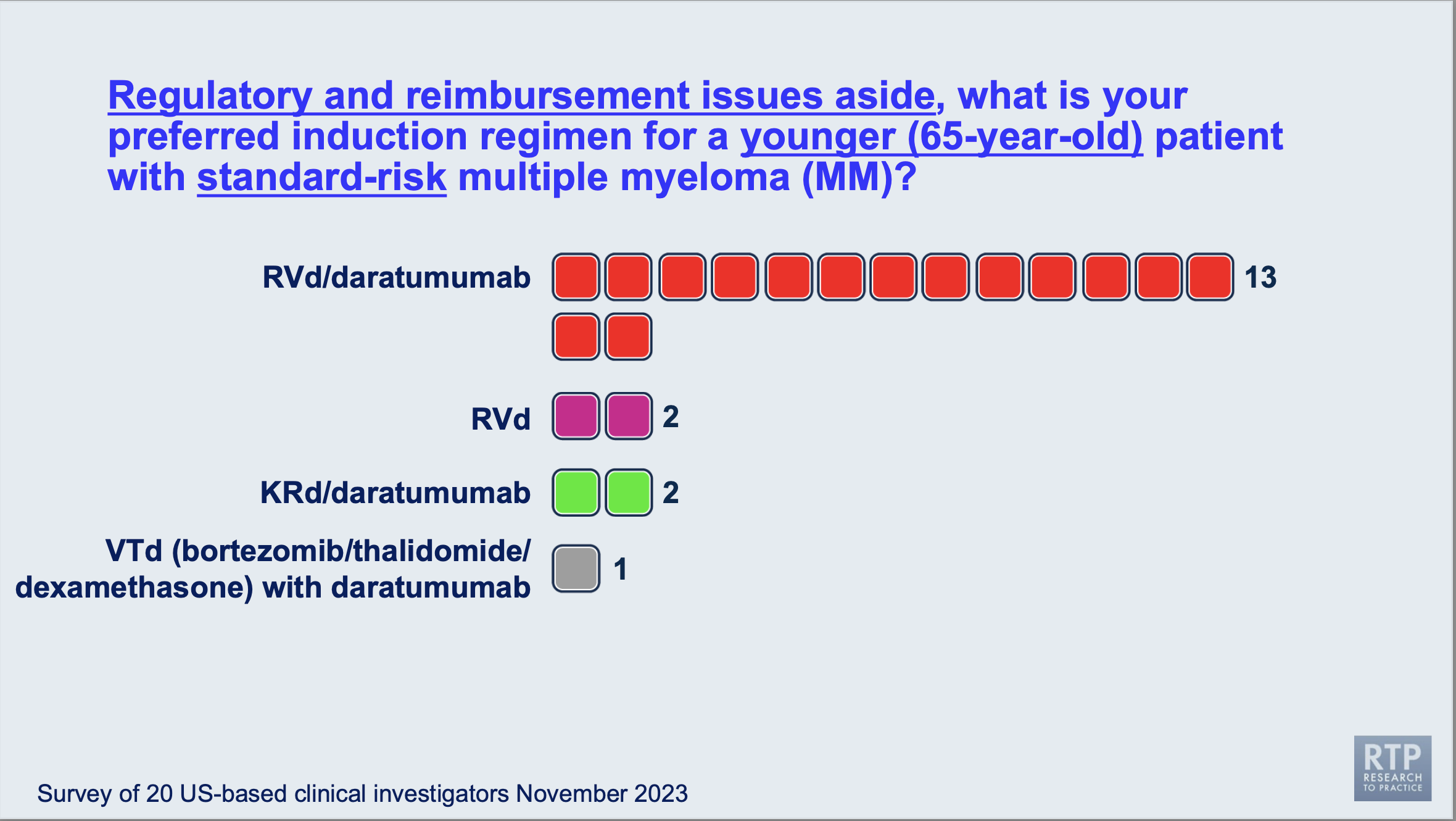
As you can see above, 13 of the myeloma specialists polled agreed that a quadruplet combination of lenalidomide (REVLIMID®), bortezomib (Velcade), and dexamethasone combined with daratumumab (DARZALEX®).
This seems to be a common trend, especially among myeloma specialists in academic centers but hasn't been a common approach for newly diagnosed myeloma patients seen only by hematologists/oncologists at community clinics or hospitals. If you are looking into induction therapy and have not yet made a decision, consider speaking with your treating team and see if adding daratumumab to your induction regimen would be right for you.
What post-transplant maintenance therapy regimen would you recommend for a younger 65-year-old patient with standard-risk multiple myeloma?
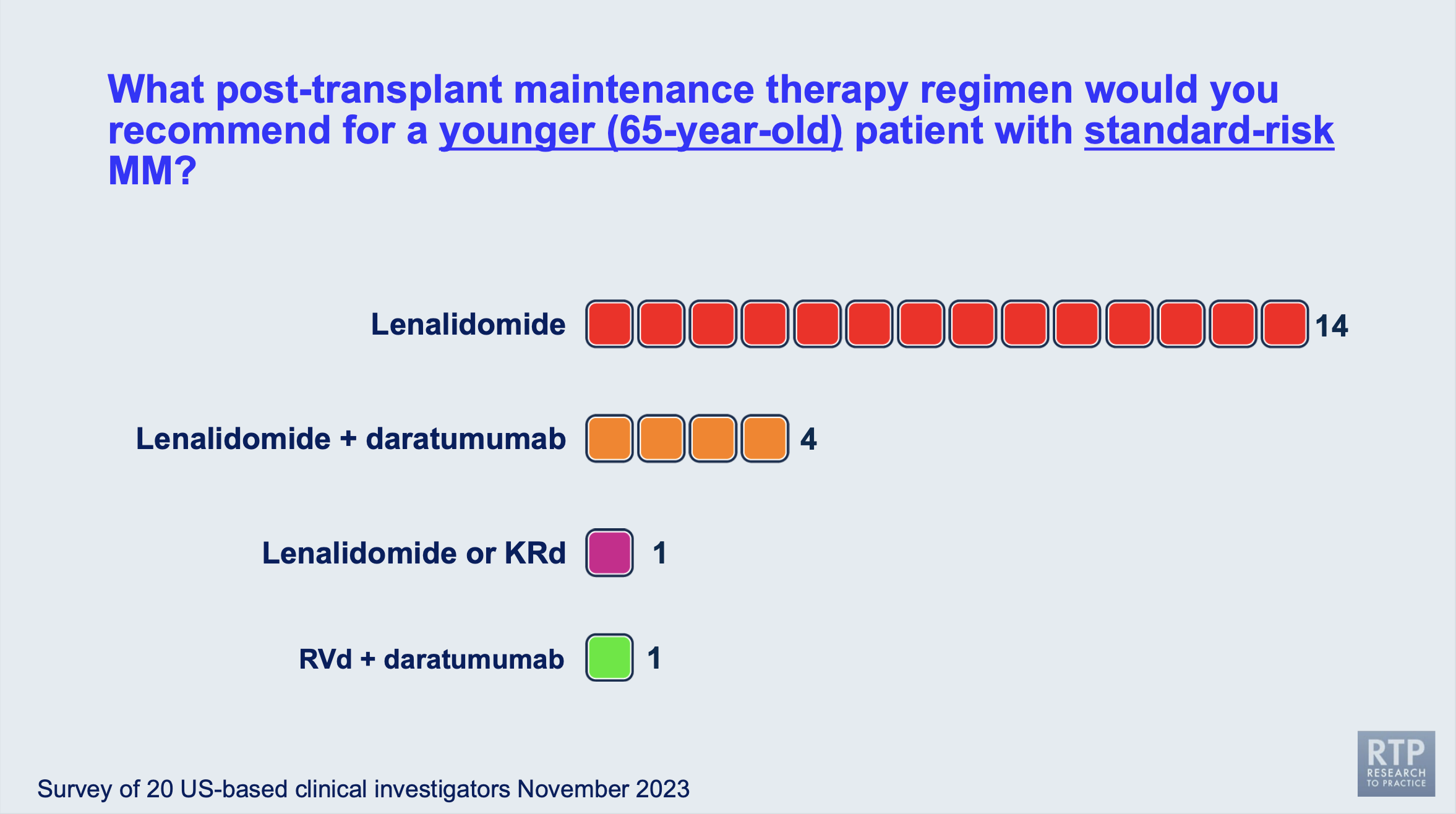
This answer was expected, but it's always good to see most myeloma specialists agree on a treatment tactic. Lenalidomide is the most commonly recommended maintenance therapy (post-transplant) by the twenty myeloma specialists surveyed. Other options included combinations of lenalidomide with daratumumab, carfilzomib, dexamethasone, or bortezomib.
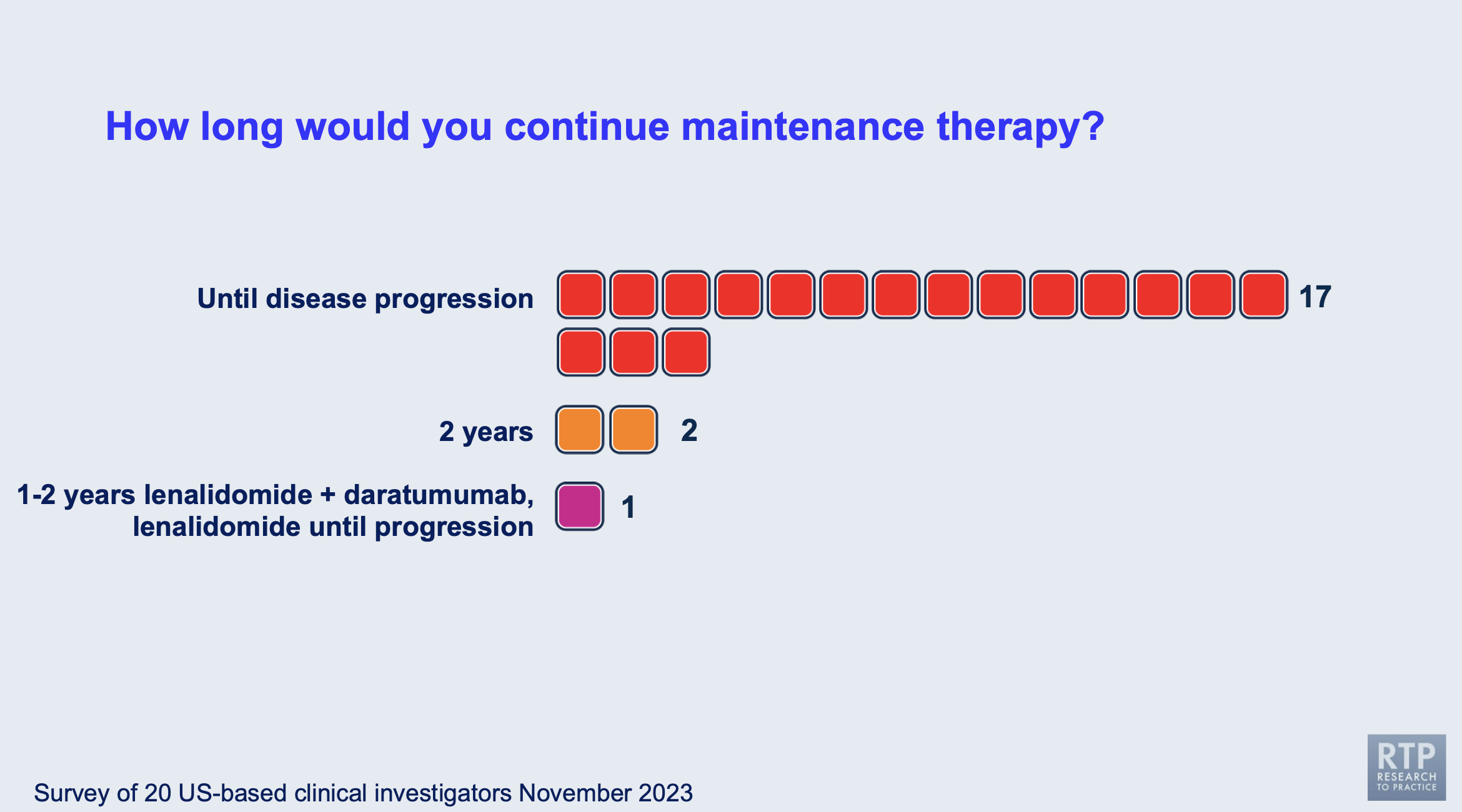
How long would you continue maintenance therapy for a standard-risk, younger myeloma patient after their stem cell transplant?

While the duration of multiple myeloma maintenance therapy is highly debated and investigated by multiple myeloma specialists, it's nice to see that thirteen of the twenty specialists currently agree on providing maintenance therapy until disease progression. The second highest response was 3 years.
Stopped maintenance therapy usually depends on the patient's response levels, disease genetics, and quality of life. You can talk to your physician to learn their philosophy on the maintenance therapy duration. Seek a second opinion to see what other myeloma specialists might recommend in your personal case.
In the live session, Dr. Paul Richardson emphasized the importance of deciding the length of maintenance therapy based on the individual patient, as myeloma is so heterogeneous and each case is unique.
What is your preferred initial regimen for an older (80-year-old) patient with standard-risk multiple myeloma who is transplant-ineligible?
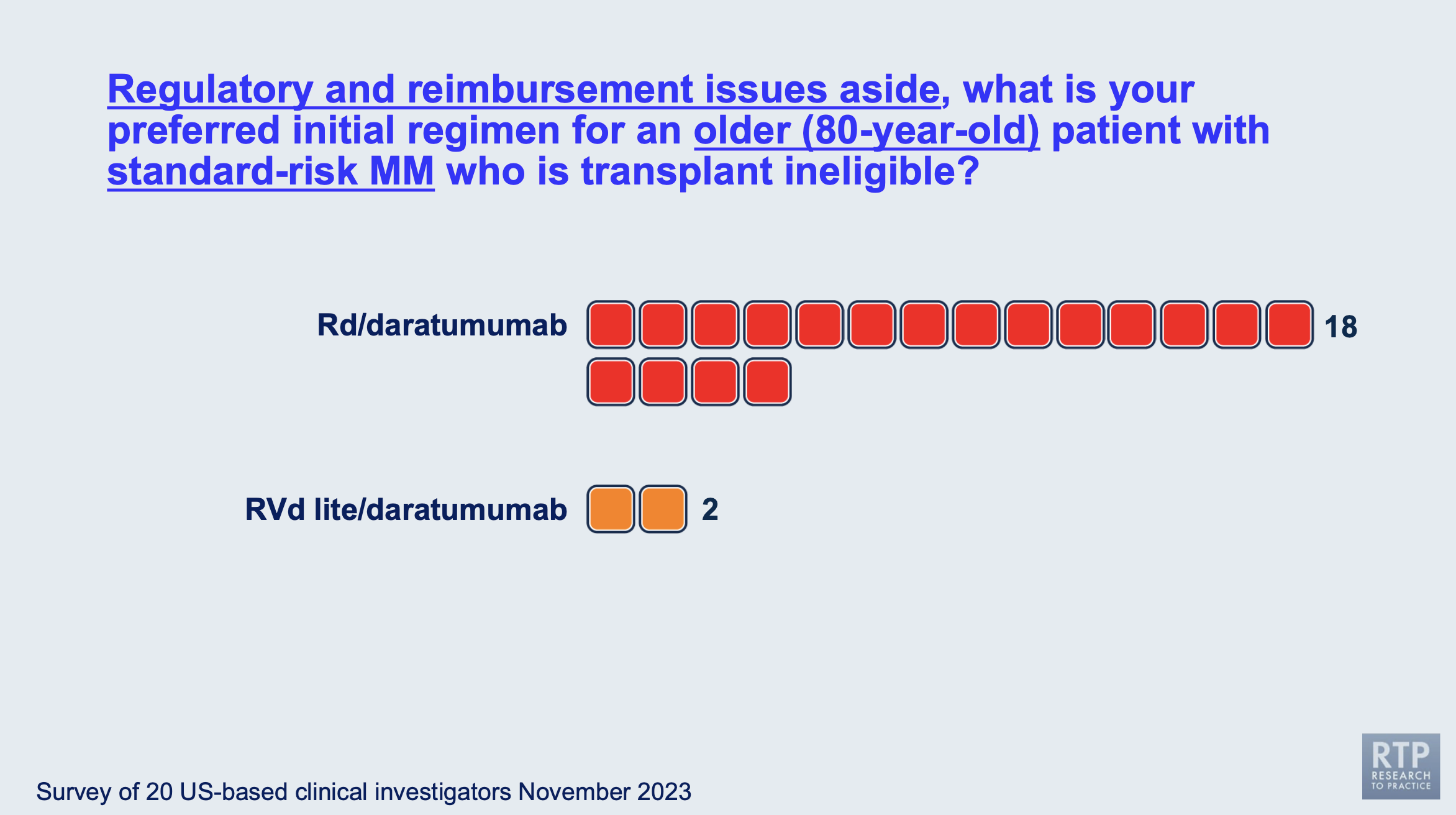
Most of the myeloma specialists agreed that for an 80-year-old myeloma patient who was standard risk and transplant-ineligible, lenalidomide (REVLIMID®), dexamethasone, and daratumumab (DARZALEX®) would be the best option for induction therapy.
That being said, in the live session the panel specialists agreed that the regimen dosing should be based on the individual patient and that these patients should be monitored for side effects and infections.
What is your recommended maintenance therapy for an older (80-year-old) patient with standard-risk multiple myeloma who is transplant-ineligible?
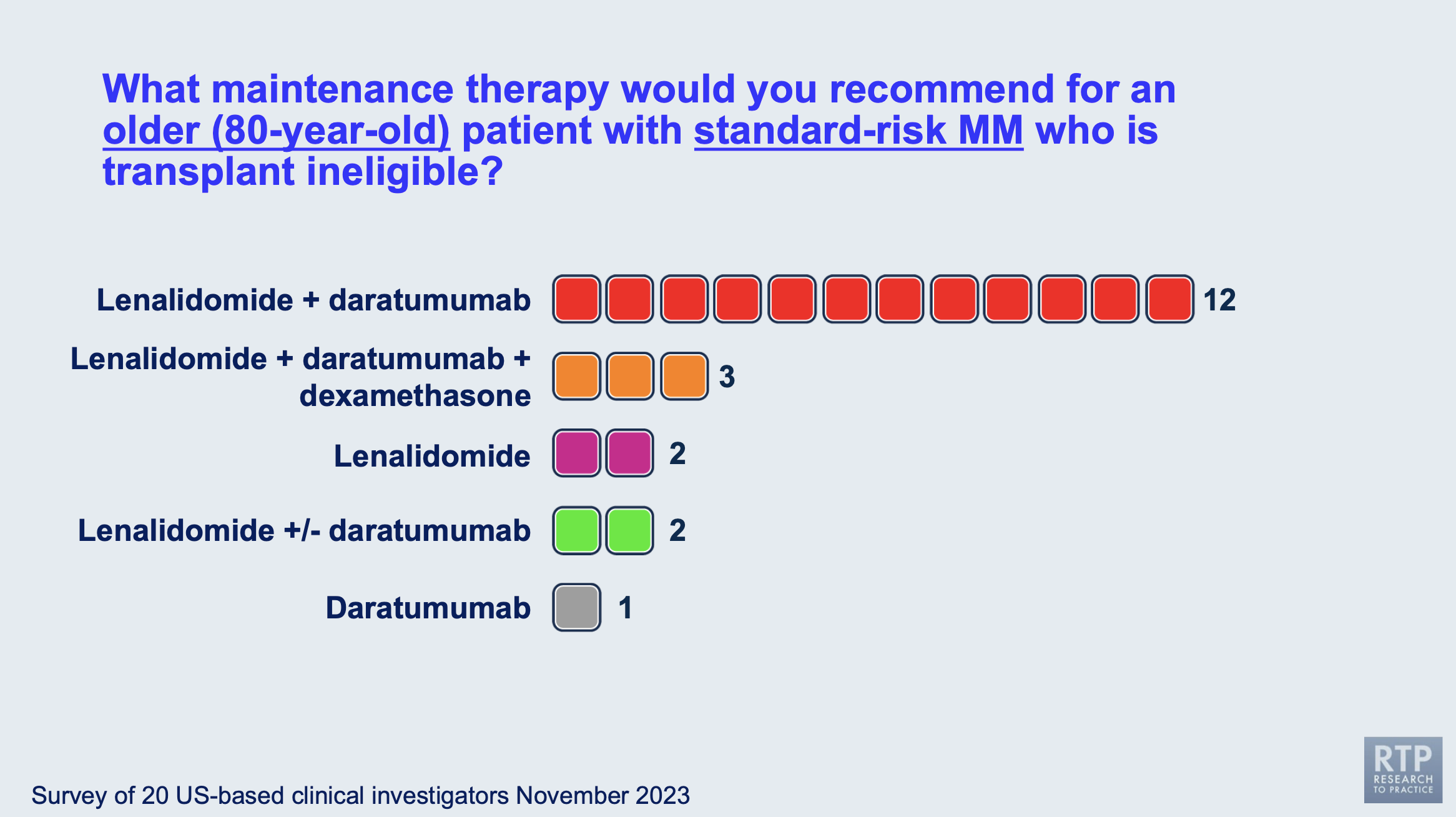
Most of the myeloma specialists agreed that for an 80-year-old myeloma patient who had standard-risk disease and was transplant-ineligible, lenalidomide (REVLIMID®) and daratumumab (DARZALEX®) would be the best option for maintenance therapy.
As you can see in the image above, the responses to this question were more mixed than the responses when asked about induction therapy.
How long would you continue maintenance therapy for an older (80-year-old) patient with standard-risk multiple myeloma who is transplant-ineligible?
Most myeloma specialists would continue maintenance therapy for older, transplant-ineligible patients until disease progression, while the minority answered other options could be made available, such as starting the patient on a doublet maintenance therapy, and only including a single agent until disease progression.
What would be your preferred induction treatment for a younger, transplant-eligible patient with high-risk multiple myeloma (for example, del[17p])?
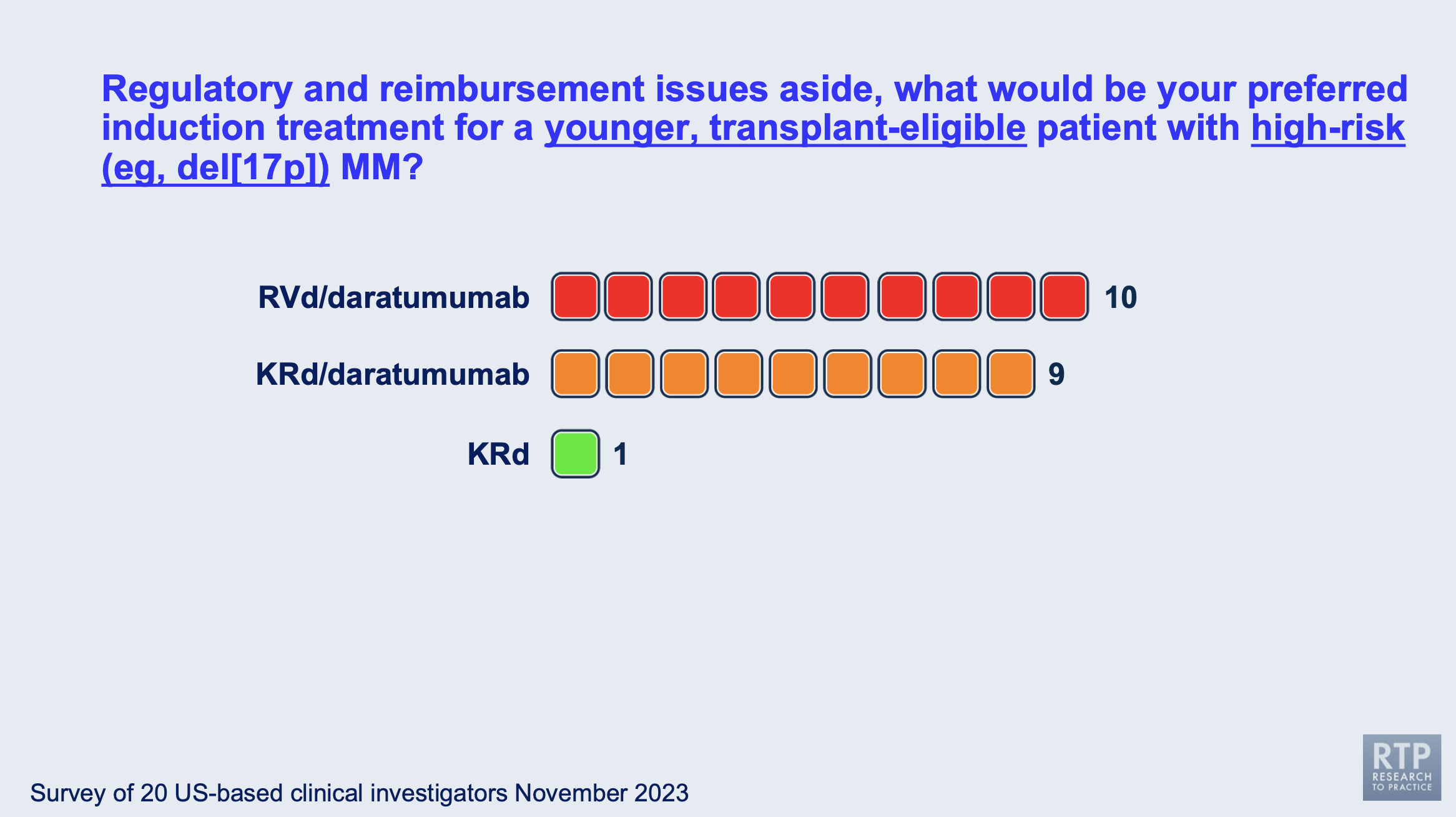
This question was one of the most divided, with most myeloma specialists splitting between using bortezomib (Velcade) or carfilzomib (Kyprolis®) in the induction therapy in combination with lenalidomide (REVLIMID®) and dexamethasone.
During the live meeting, Dr. Bob Orlowski shared his input that not every myeloma patient should receive a stem cell transplant as those with standard risk who achieve MRD negativity after induction have no need for an immediate transplant, though collection would be recommended. However, with high-risk myeloma, an immediate stem cell transplant might be recommended.
This is certainly something to keep in mind when considering a stem cell transplant with your physician.
What is your preferred initial regimen for an (80-year-old) patient with high-risk multiple myeloma (del[17p]) who is transplant-ineligible?
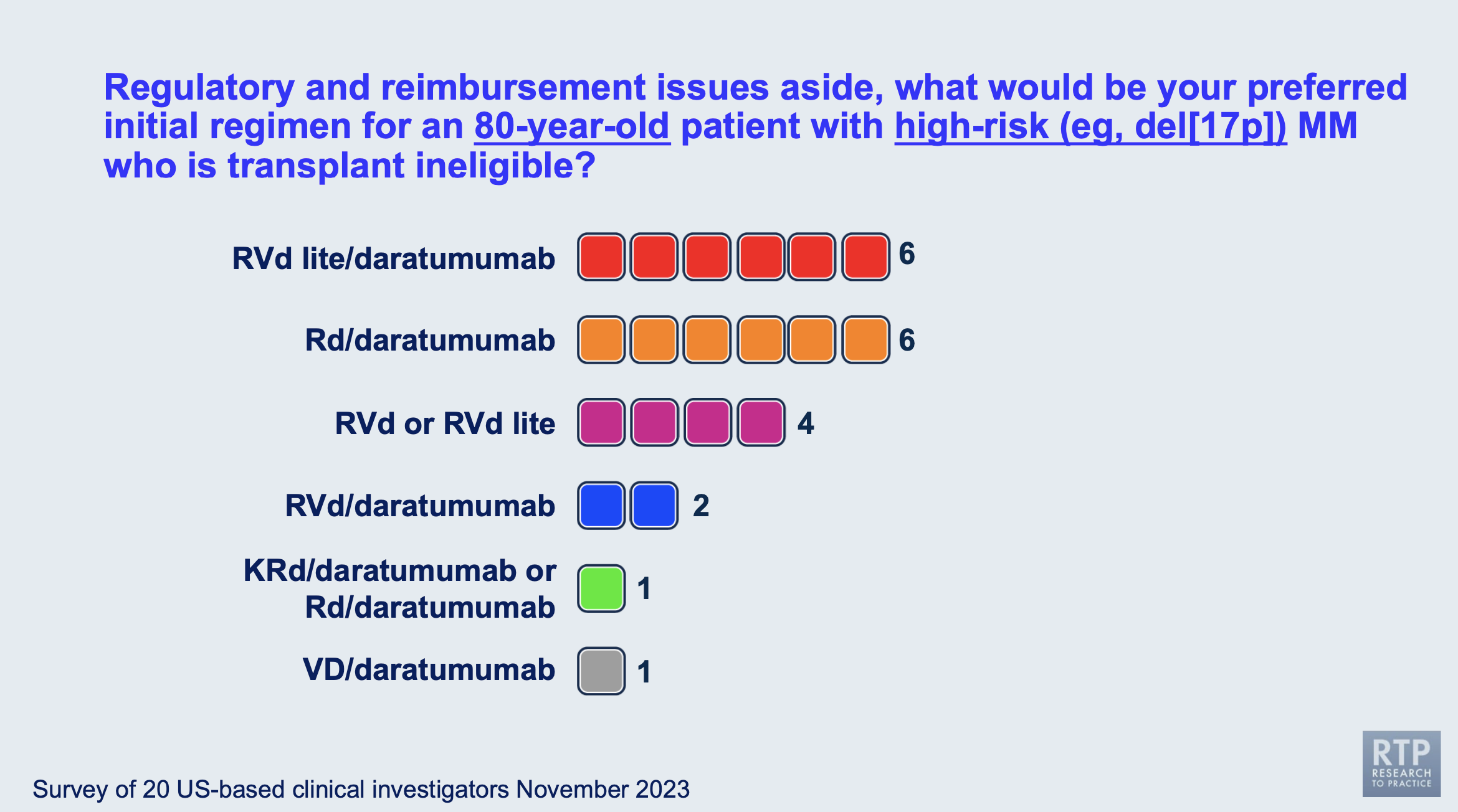
This was a highly divided question with many specialists differing in their answers. Most of the specialists chose either an RVd lite (lower than standard dose combination of lenalidomide, bortezomib, and dexamethasone) with daratumumab added, and a combination of lenalidomide, dexamethasone, and daratumamab.
How do you approach the stem cell transplant within your own myeloma practice?
One of the most important topics discussed during the live session was the issue of stem cell transplants within the specialists' own myeloma practice.
Dr. Paul Richardson agreed with Dr. Bob Orlowski’s previous comment that those with high-risk disease probably need the transplant, while the options remain more flexible for those patients with standard-risk myeloma.
Quadruplet combinations (such as Dara-RVd) are taking over the induction field, and are changing the treatment landscape. This causes myeloma specialists to take a step back and think about questions like this for the next generation of myeloma patients.
The younger standard-risk patients who have high-quality responses to a quadruplet induction therapy have less likelihood of needing a transplant, especially with the risk that comes with high-dose melphalan that could cause more harm/lower the quality of life that they are currently experiencing.
Dr. Sagar Lonial shared his perspective that the rumors of the demise of stem cell transplants are premature- the transplants have incredible results for a lot of patients and those incredible results haven't changed with the emerging novel therapies being approved.
Having the discussion is reasonable but undertreating a standard-risk patient can lead to a higher-risk patient in the future. It's also important to note that there are patients who are considered "functionally high-risk" in which their disease biology shows all the "standard-risk" signs, but the disease responds like a high-risk patient, with shorter response times and less deep responses. When considering the survival benefit of stem cell transplants, there may not be an overall survival benefit, but there is a progression-free survival benefit.
Dr. Noopur Raje reminded the audience of the importance of presenting all of the data to the patients but respecting the patients' decisions in the end. She emphasized the importance of encouraging patients to collect their stem cells for possible future use since the results of a stem cell transplant did not depend on the timing of their SCT.
Conclusions
While there is a lot of debate surrounding important myeloma decisions, most myeloma specialists can come together and agree on a treatment strategy that benefits their patients the most. Make sure to keep honest and open communication with your doctor and have a treating specialist from an academic center on your team. To look for a myeloma specialist in your area, check out our directory: Myeloma Specialist Directory
With how fast the myeloma research field is moving, it's imperative you include a specialist on your treating team to make sure that you are receiving the best care possible for your overall survival and quality of life.
Resources
If you are interested in reading more articles for the 2023 American Society of Hematology (ASH) Conference, read them here: ASH 2023 Articles
It's been said that if you ask three multiple myeloma specialists a question, you'll receive six answers. While this can be true, the Beyond the Guidelines: Clinical Investigator Perspectives on the Management of Multiple Myeloma session moderated by Neil Love, MD of RTP (Research to Practice) revealed that when it comes to providing concise answers for important myeloma decisions, most specialists tended to agree with one another.
Let's look more into these questions and decisions below.
Dr. Neil Love asked twenty myeloma specialists to participate in a survey regarding myeloma treatment decisions in preparation for this event. The twenty myeloma specialists who responded to Dr. Love's survey were:
- Melissa Alsina, MD
- Jesús Berdeja, MD
- Natalie Callander, MD
- Rafael Fonseca, MD
- Carol Ann Huff, MD
- Jonathan Kaufman, MD
- Amrita Krishnan, MD
- Shaji Kumar, MD
- Ola Landgren, MD, PhD
- Sagar Lonial, MD
- Tom Martin, MD
- Joseph Mikhael, MD, MEd
- Philippe Moreau, MD
- Robert Orlowski, MD, PhD
- Krina Patel, MD, MSc
- Noopur Raje, MD
- Paul Richardson, MD
- Keith Stewart, MB, ChB
- Sascha Tuchman, MD, MHS
- Jeffrey Zonder, MD
Before we get started, please remember that none of the information presented below should be taken as personal medical advice, but rather serve as a resource support to discuss with your doctor and treating medical team.
What is your preferred induction regimen for a younger 65-year-old patient with standard-risk multiple myeloma?
This question was asked to the 20 specialists, who were asked to put regulatory and reimbursement issues aside. The responses were actually quite similar considering how many specialists were asked the question.
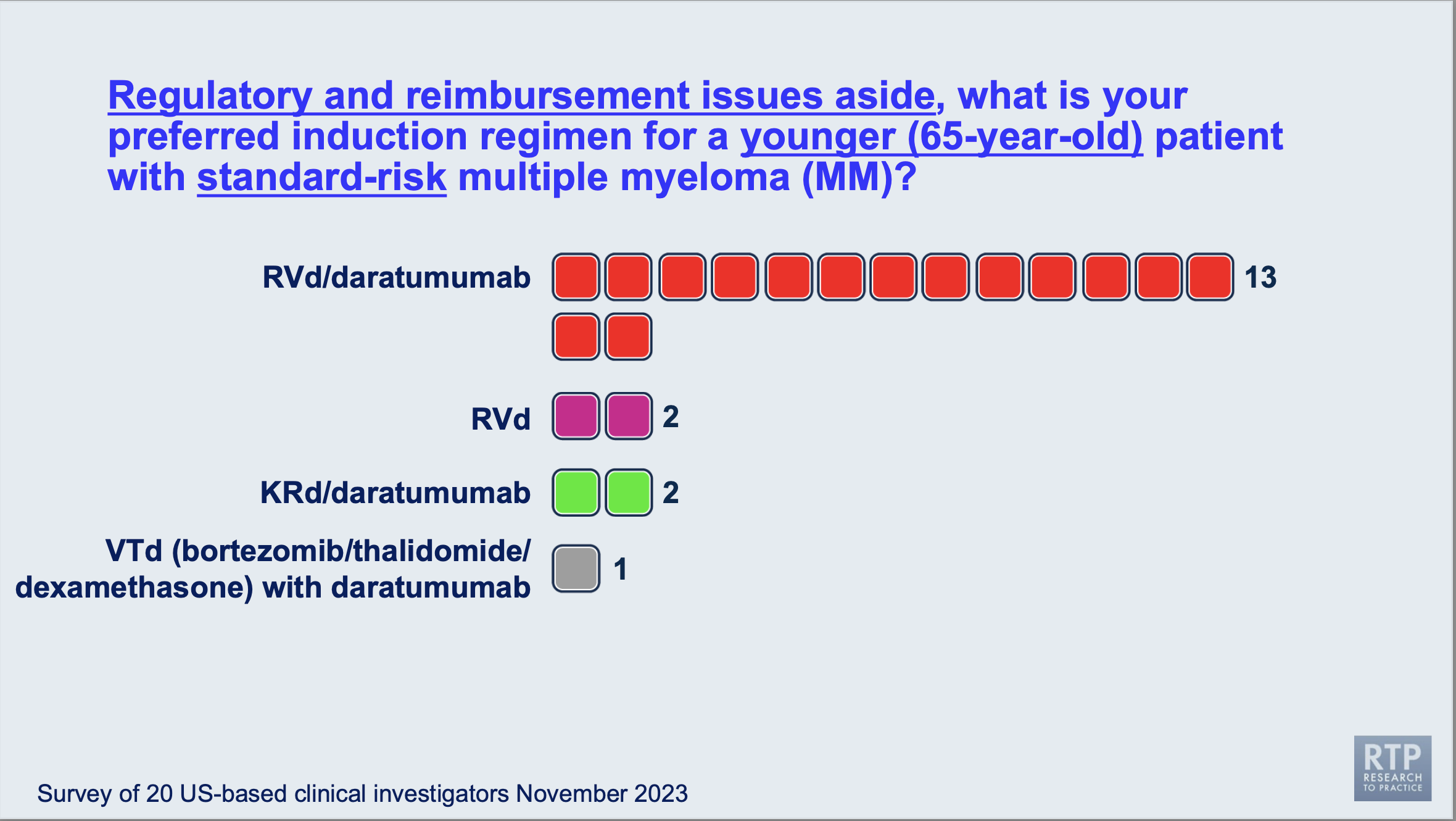
As you can see above, 13 of the myeloma specialists polled agreed that a quadruplet combination of lenalidomide (REVLIMID®), bortezomib (Velcade), and dexamethasone combined with daratumumab (DARZALEX®).
This seems to be a common trend, especially among myeloma specialists in academic centers but hasn't been a common approach for newly diagnosed myeloma patients seen only by hematologists/oncologists at community clinics or hospitals. If you are looking into induction therapy and have not yet made a decision, consider speaking with your treating team and see if adding daratumumab to your induction regimen would be right for you.
What post-transplant maintenance therapy regimen would you recommend for a younger 65-year-old patient with standard-risk multiple myeloma?
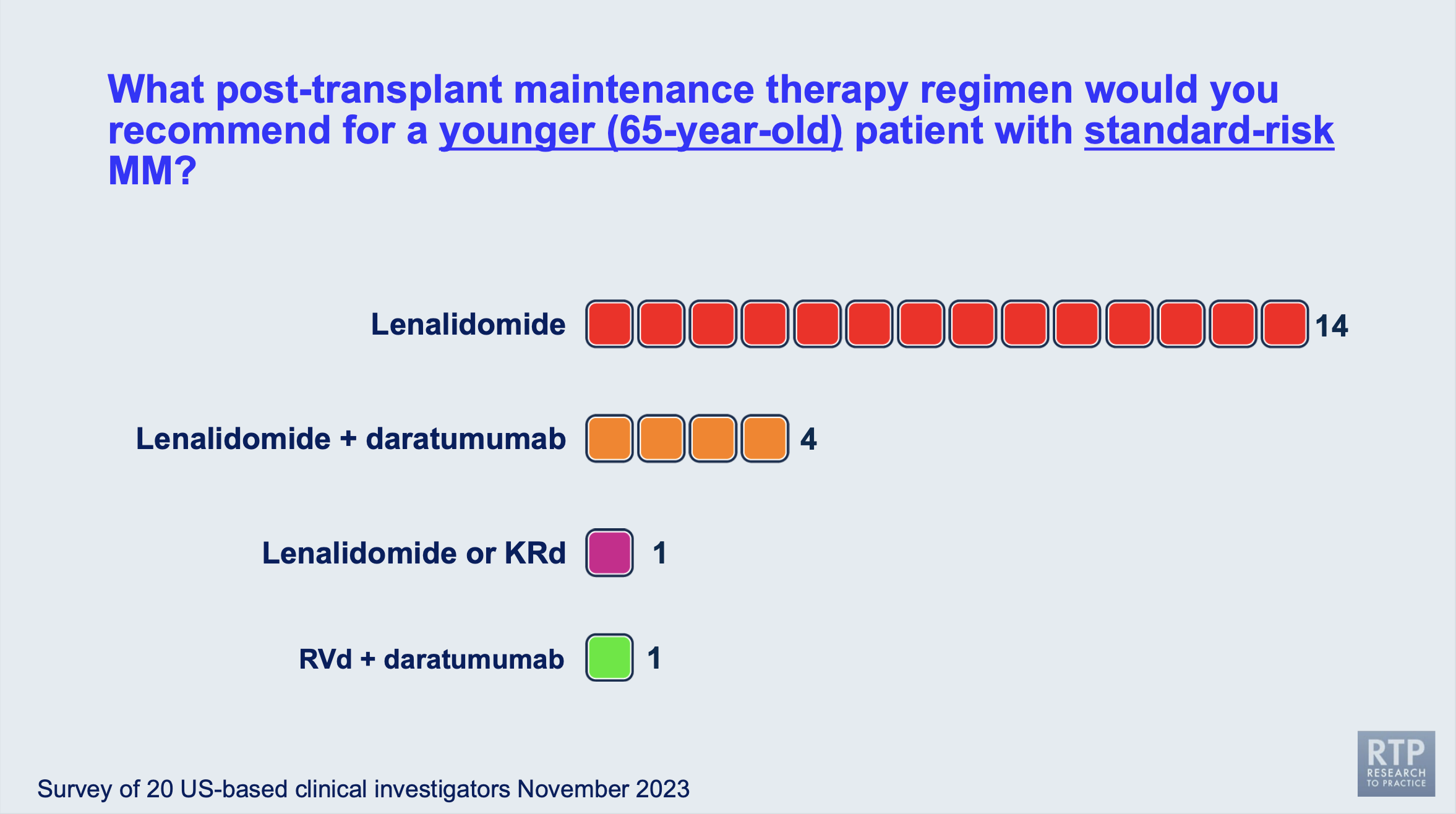
This answer was expected, but it's always good to see most myeloma specialists agree on a treatment tactic. Lenalidomide is the most commonly recommended maintenance therapy (post-transplant) by the twenty myeloma specialists surveyed. Other options included combinations of lenalidomide with daratumumab, carfilzomib, dexamethasone, or bortezomib.
How long would you continue maintenance therapy for a standard-risk, younger myeloma patient after their stem cell transplant?

While the duration of multiple myeloma maintenance therapy is highly debated and investigated by multiple myeloma specialists, it's nice to see that thirteen of the twenty specialists currently agree on providing maintenance therapy until disease progression. The second highest response was 3 years.
Stopped maintenance therapy usually depends on the patient's response levels, disease genetics, and quality of life. You can talk to your physician to learn their philosophy on the maintenance therapy duration. Seek a second opinion to see what other myeloma specialists might recommend in your personal case.
In the live session, Dr. Paul Richardson emphasized the importance of deciding the length of maintenance therapy based on the individual patient, as myeloma is so heterogeneous and each case is unique.
What is your preferred initial regimen for an older (80-year-old) patient with standard-risk multiple myeloma who is transplant-ineligible?
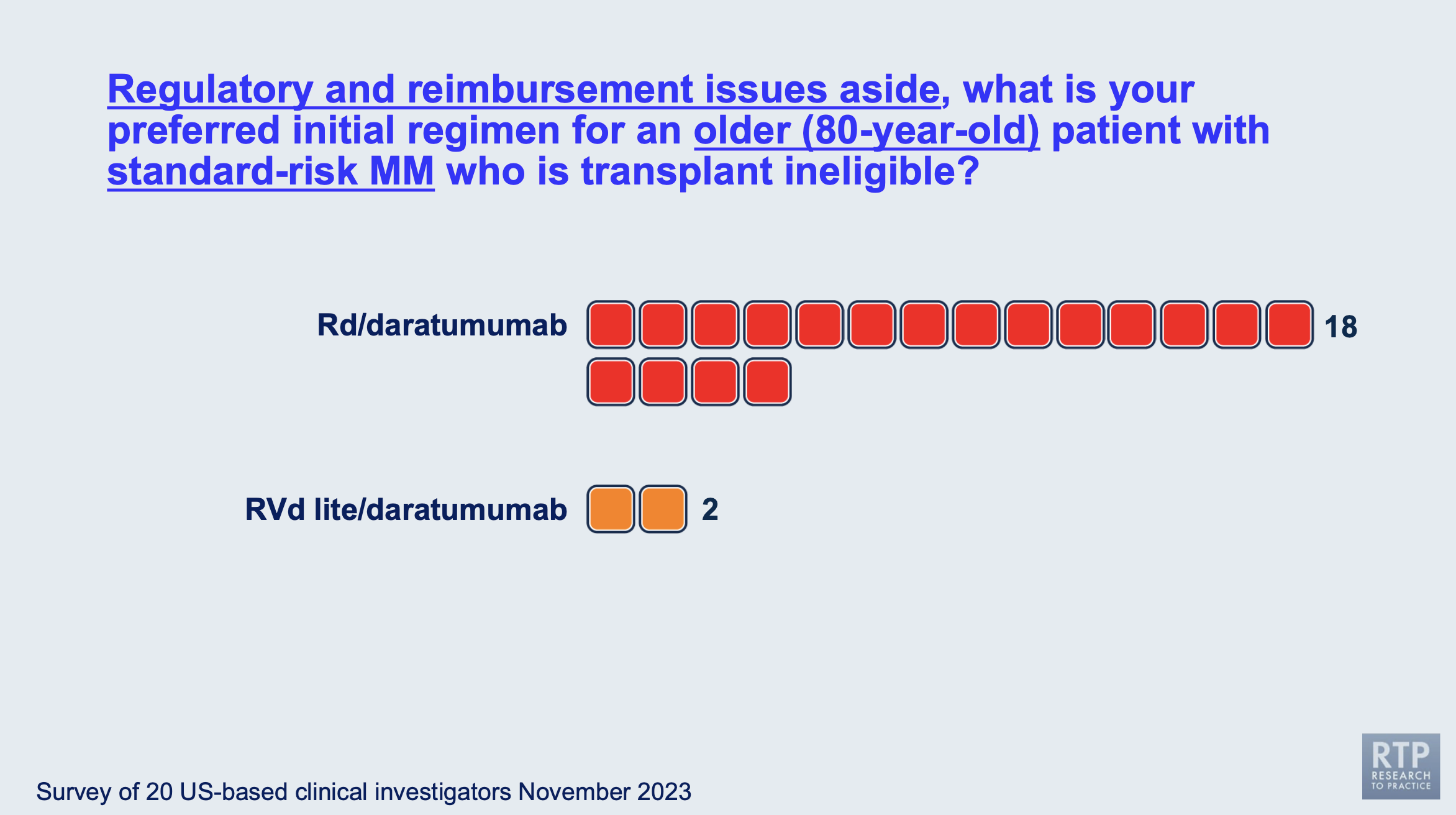
Most of the myeloma specialists agreed that for an 80-year-old myeloma patient who was standard risk and transplant-ineligible, lenalidomide (REVLIMID®), dexamethasone, and daratumumab (DARZALEX®) would be the best option for induction therapy.
That being said, in the live session the panel specialists agreed that the regimen dosing should be based on the individual patient and that these patients should be monitored for side effects and infections.
What is your recommended maintenance therapy for an older (80-year-old) patient with standard-risk multiple myeloma who is transplant-ineligible?
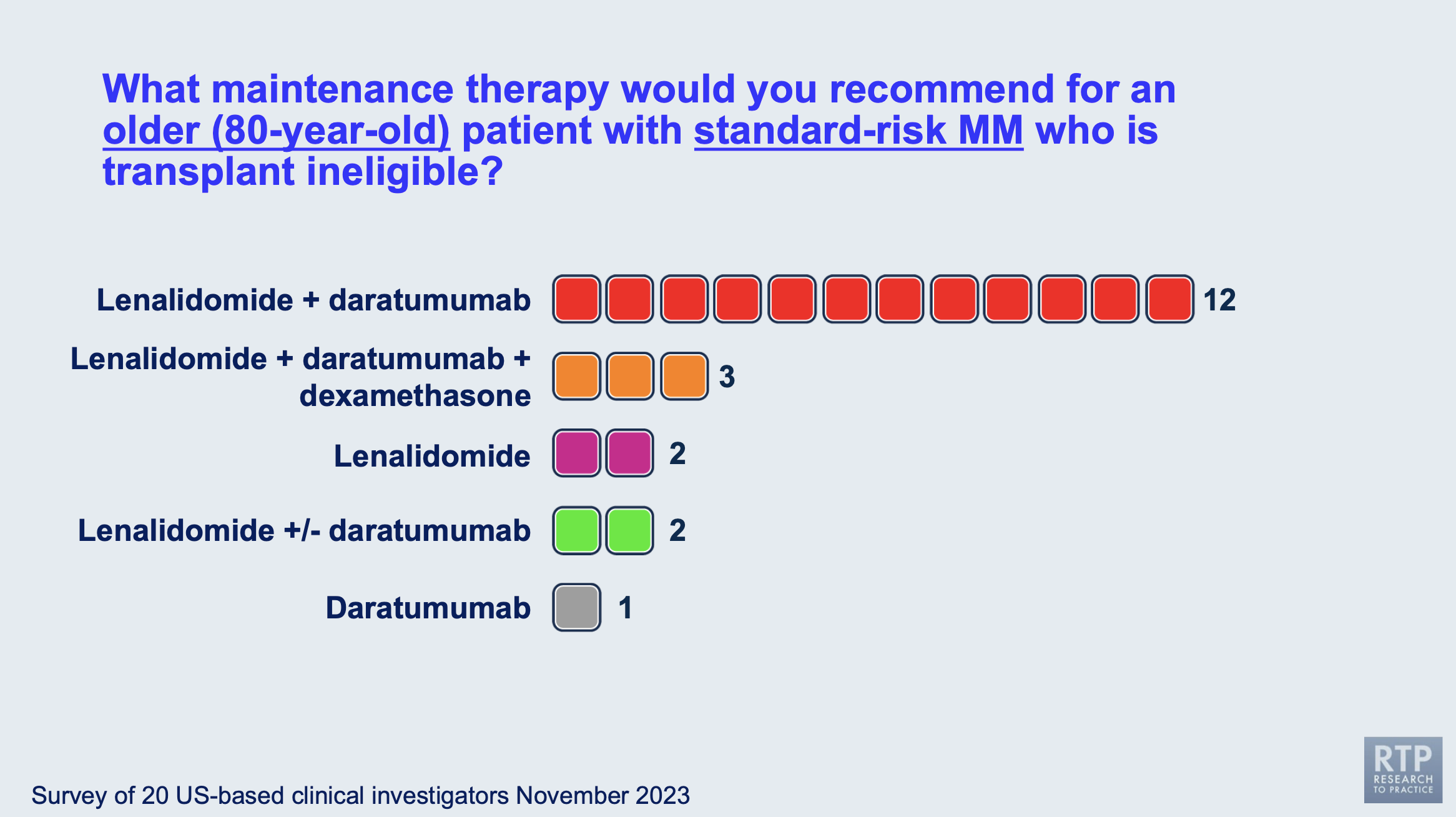
Most of the myeloma specialists agreed that for an 80-year-old myeloma patient who had standard-risk disease and was transplant-ineligible, lenalidomide (REVLIMID®) and daratumumab (DARZALEX®) would be the best option for maintenance therapy.
As you can see in the image above, the responses to this question were more mixed than the responses when asked about induction therapy.
How long would you continue maintenance therapy for an older (80-year-old) patient with standard-risk multiple myeloma who is transplant-ineligible?
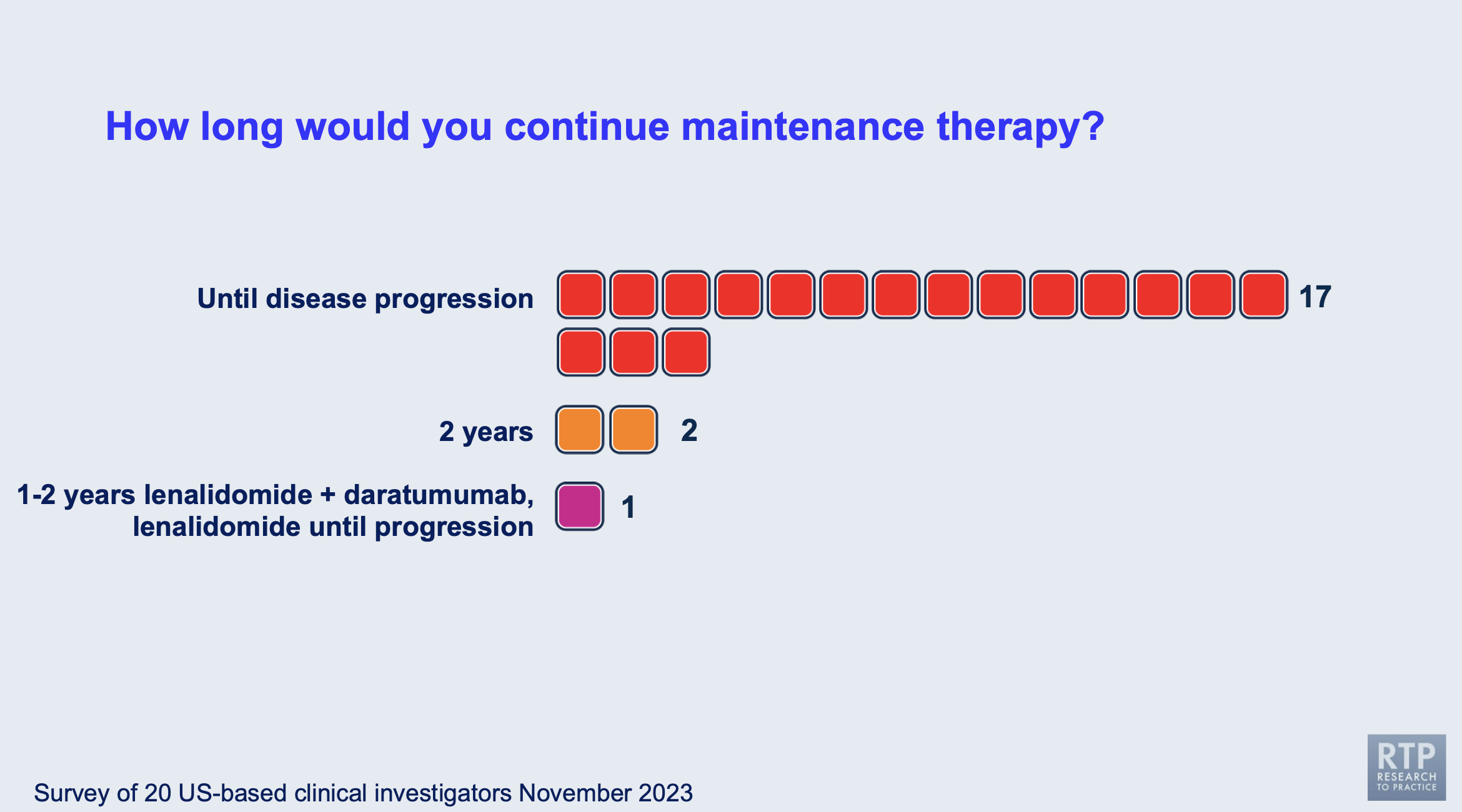
Most myeloma specialists would continue maintenance therapy for older, transplant-ineligible patients until disease progression, while the minority answered other options could be made available, such as starting the patient on a doublet maintenance therapy, and only including a single agent until disease progression.
What would be your preferred induction treatment for a younger, transplant-eligible patient with high-risk multiple myeloma (for example, del[17p])?
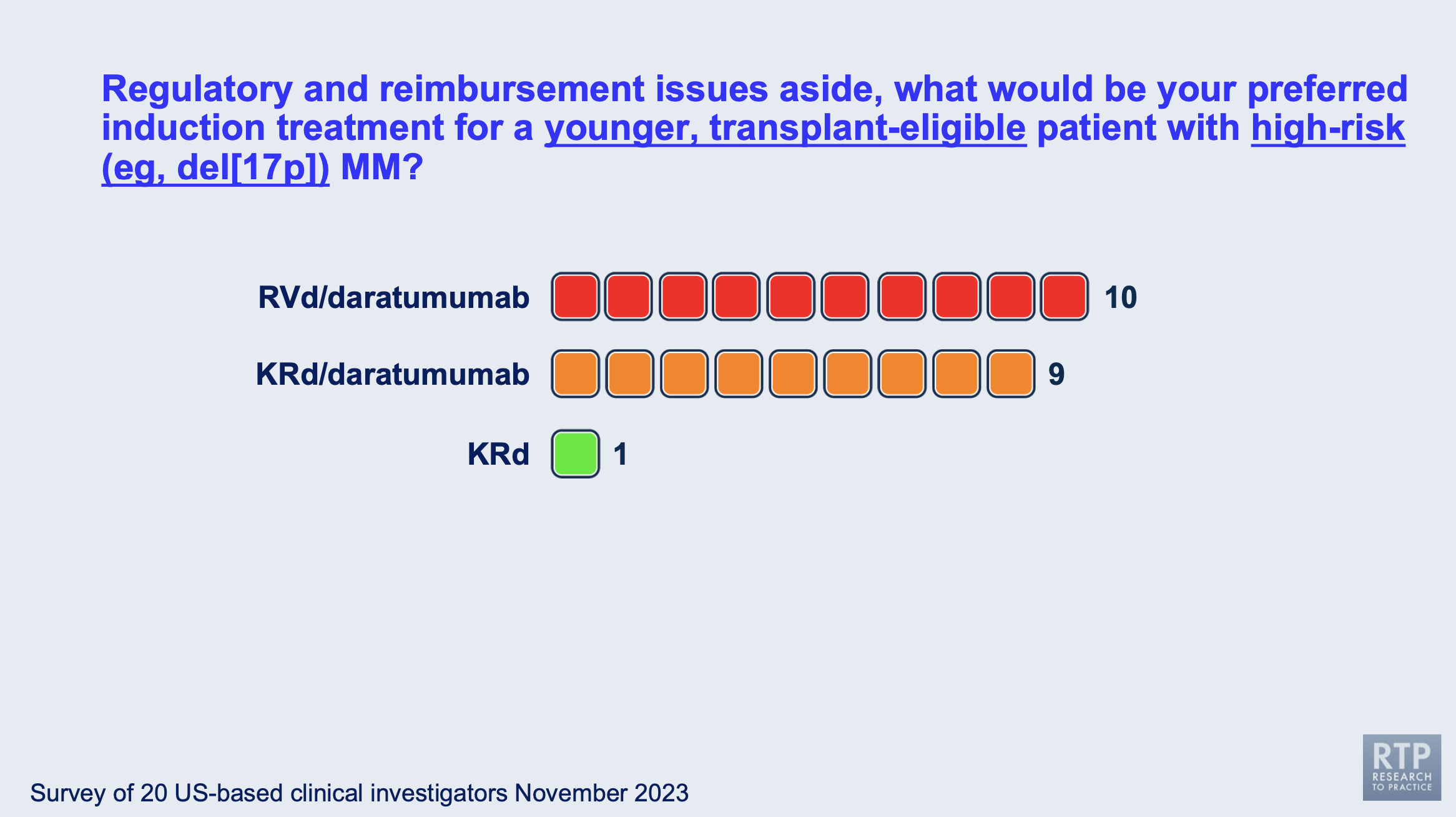
This question was one of the most divided, with most myeloma specialists splitting between using bortezomib (Velcade) or carfilzomib (Kyprolis®) in the induction therapy in combination with lenalidomide (REVLIMID®) and dexamethasone.
During the live meeting, Dr. Bob Orlowski shared his input that not every myeloma patient should receive a stem cell transplant as those with standard risk who achieve MRD negativity after induction have no need for an immediate transplant, though collection would be recommended. However, with high-risk myeloma, an immediate stem cell transplant might be recommended.
This is certainly something to keep in mind when considering a stem cell transplant with your physician.
What is your preferred initial regimen for an (80-year-old) patient with high-risk multiple myeloma (del[17p]) who is transplant-ineligible?
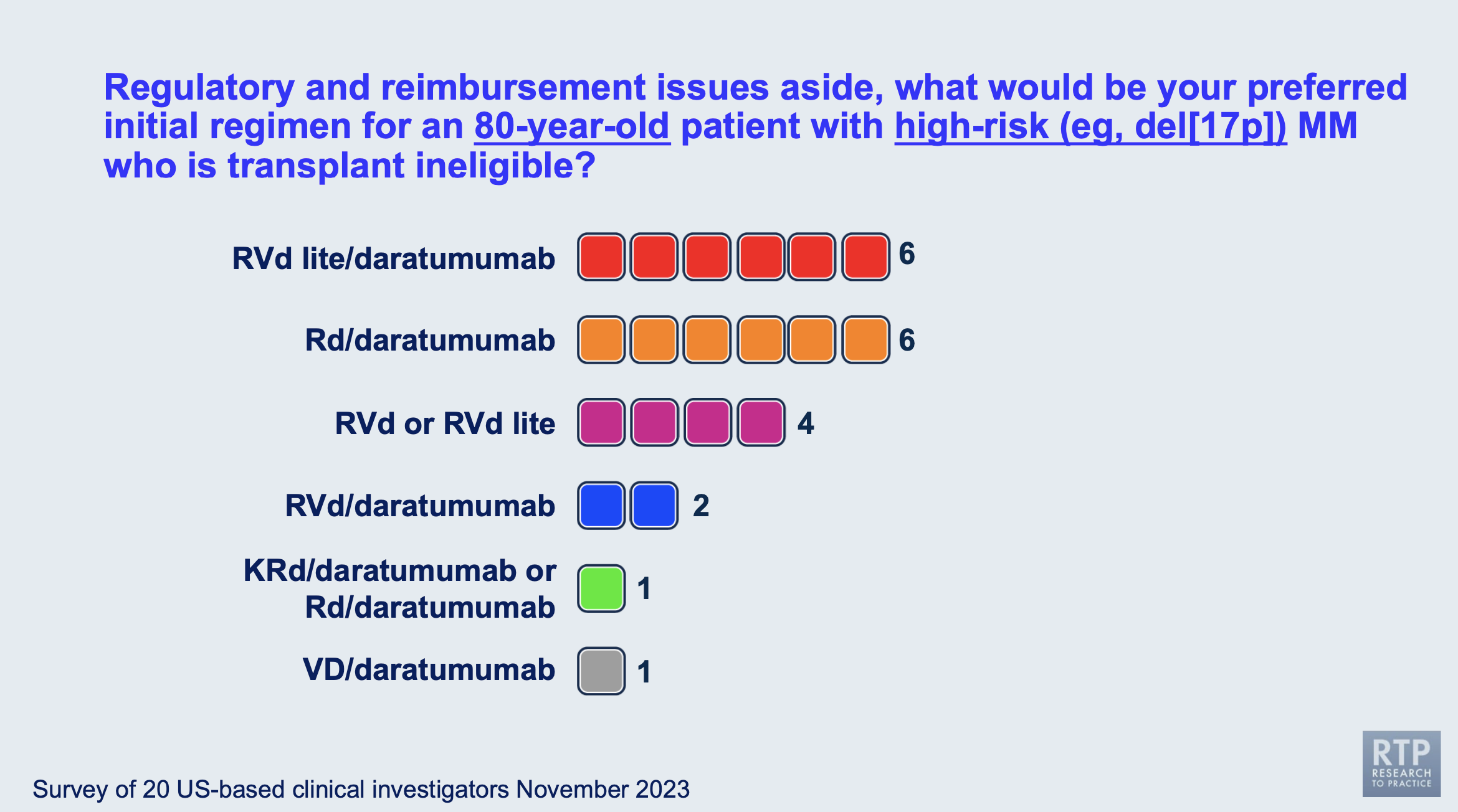
This was a highly divided question with many specialists differing in their answers. Most of the specialists chose either an RVd lite (lower than standard dose combination of lenalidomide, bortezomib, and dexamethasone) with daratumumab added, and a combination of lenalidomide, dexamethasone, and daratumamab.
How do you approach the stem cell transplant within your own myeloma practice?
One of the most important topics discussed during the live session was the issue of stem cell transplants within the specialists' own myeloma practice.
Dr. Paul Richardson agreed with Dr. Bob Orlowski’s previous comment that those with high-risk disease probably need the transplant, while the options remain more flexible for those patients with standard-risk myeloma.
Quadruplet combinations (such as Dara-RVd) are taking over the induction field, and are changing the treatment landscape. This causes myeloma specialists to take a step back and think about questions like this for the next generation of myeloma patients.
The younger standard-risk patients who have high-quality responses to a quadruplet induction therapy have less likelihood of needing a transplant, especially with the risk that comes with high-dose melphalan that could cause more harm/lower the quality of life that they are currently experiencing.
Dr. Sagar Lonial shared his perspective that the rumors of the demise of stem cell transplants are premature- the transplants have incredible results for a lot of patients and those incredible results haven't changed with the emerging novel therapies being approved.
Having the discussion is reasonable but undertreating a standard-risk patient can lead to a higher-risk patient in the future. It's also important to note that there are patients who are considered "functionally high-risk" in which their disease biology shows all the "standard-risk" signs, but the disease responds like a high-risk patient, with shorter response times and less deep responses. When considering the survival benefit of stem cell transplants, there may not be an overall survival benefit, but there is a progression-free survival benefit.
Dr. Noopur Raje reminded the audience of the importance of presenting all of the data to the patients but respecting the patients' decisions in the end. She emphasized the importance of encouraging patients to collect their stem cells for possible future use since the results of a stem cell transplant did not depend on the timing of their SCT.
Conclusions
While there is a lot of debate surrounding important myeloma decisions, most myeloma specialists can come together and agree on a treatment strategy that benefits their patients the most. Make sure to keep honest and open communication with your doctor and have a treating specialist from an academic center on your team. To look for a myeloma specialist in your area, check out our directory: Myeloma Specialist Directory
With how fast the myeloma research field is moving, it's imperative you include a specialist on your treating team to make sure that you are receiving the best care possible for your overall survival and quality of life.
Resources
If you are interested in reading more articles for the 2023 American Society of Hematology (ASH) Conference, read them here: ASH 2023 Articles
about the author
Jennifer Ahlstrom
Myeloma survivor, patient advocate, wife, mom of 6. Believer that patients can contribute to cures by joining HealthTree Cure Hub and joining clinical research. Founder and CEO of HealthTree Foundation.










